As with all complaints in medicine, the first step is to obtain a detailed history. The first question should be one aimed at best characterizing the sensation (or lack thereof) described by the patient. It is important to differentiate between numbness as a loss of sensation as opposed to the presence of an abnormal sensation. At times, patients may also use the term numbness to describe muscle weakness, and this is important to keep in mind during one’s examination.
NEUROPATHIC PAIN
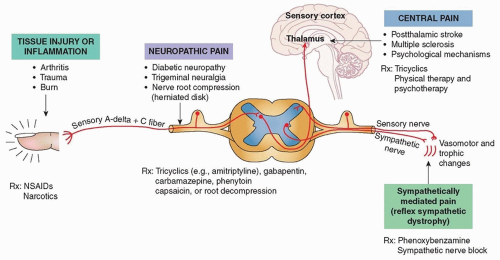
Neuropathic pain (see
Chapter 57) is a category of pain specific to that caused by nerve injury and is often described as painful paresthesias, associated with a sensation of burning or radiating pain as can be seen in cases of peripheral neuropathy or radiculopathy (
Fig. 8.1). In such cases, patients may exhibit altered sensation or abnormally increased sensations—
hyperesthesia refers to increased sensation, whereas
dysesthesia refers to an evoked unpleasant or painful sensation.
An exaggerated response to stimuli that normally evoke pain is known as hyperalgesia, whereas an exaggerated response to stimuli that should not normally invoke pain is referred to as allodynia. These abnormal sensations can be seen with various nerve injuries, both at the central and peripheral level. Conversely, hypoesthesia refers to the diminished perception of pain, anesthesia to the inability to perceive pain, and analgesia to the inability to feel pain.
Neuropathic pain must be differentiated from somatic pain caused by pathology in bones, ligaments, muscles, and other soft tissues.
Complex regional pain syndrome (CRPS; also known as
reflex sympathetic dystrophy) is a chronic disease characterized by severe neuropathic pain, skin changes, and swelling in one limb. It may occur in the absence of a known nerve injury (type 1) or in the
setting of known nerve injury (type 2). Diagnosis and treatment of CRPS is further discussed in Chapter 56.