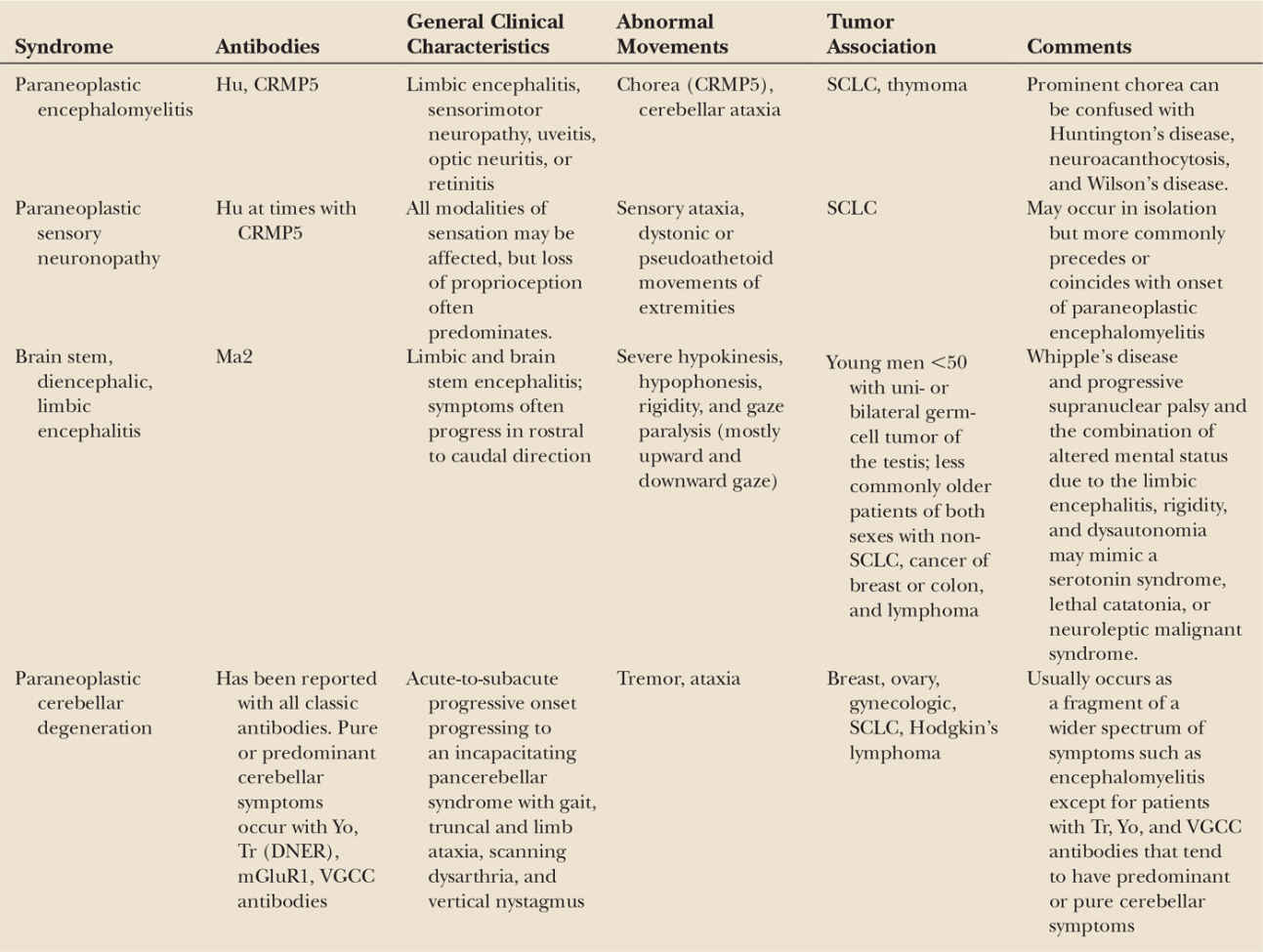
There are an increasing number of recognized and suspected immune-mediated disorders that associate with abnormal movements. The immune-mediated paraneoplastic neurologic disorders (PND) are thought to be triggered by the presence of a systemic tumor that expresses a neuronal protein leading to breakdown in the normal self-tolerance to brain antigens (1). In many PND, the autoimmune responses are marked by the presence of highly specific antineuronal antibodies (Table 32.1) (2). These antibodies target intracellular neuronal antigens and are markers of the paraneoplastic process. The neuronal dysfunction that results in PND is mediated by brain cytotoxic T-cell infiltrates (3,4). In some PND such as neuroblastoma-associated opsoclonus–myoclonus, there is strong evidence of autoimmunity, but no specific antibody has been identified (5,6). Abnormal movements are prominent in some of the autoimmune encephalitis syndromes associated to antibodies that target neuronal cell-surface or synaptic receptors (7,8). These disorders occur both with and without a cancer association, and the antibodies directly mediate the neuronal dysfunction (9). The immunologic trigger in the paraneoplastic cases is likely the tumor, but it is not clear what initiates the immune response in the nonparaneoplastic cases. Postinfectious immune-mediated movement disorders are well known and have been thought to be triggered by molecular mimicry or other, as yet unknown, mechanisms. Recent evidence demonstrates that herpes simplex infection can lead to the development of autoimmune encephalitis, providing insights into the pathogenesis of some syndromes, such as “choreoathetosis post-herpes simplex encephalitis” (HSE) (10,11). In addition, there are systemic diseases with associated movement disorders such as Sjögren’s syndrome, systemic lupus erythematosus, and poststreptococcal syndromes in which unknown immune mechanisms are suspected but have not been clearly demonstrated.
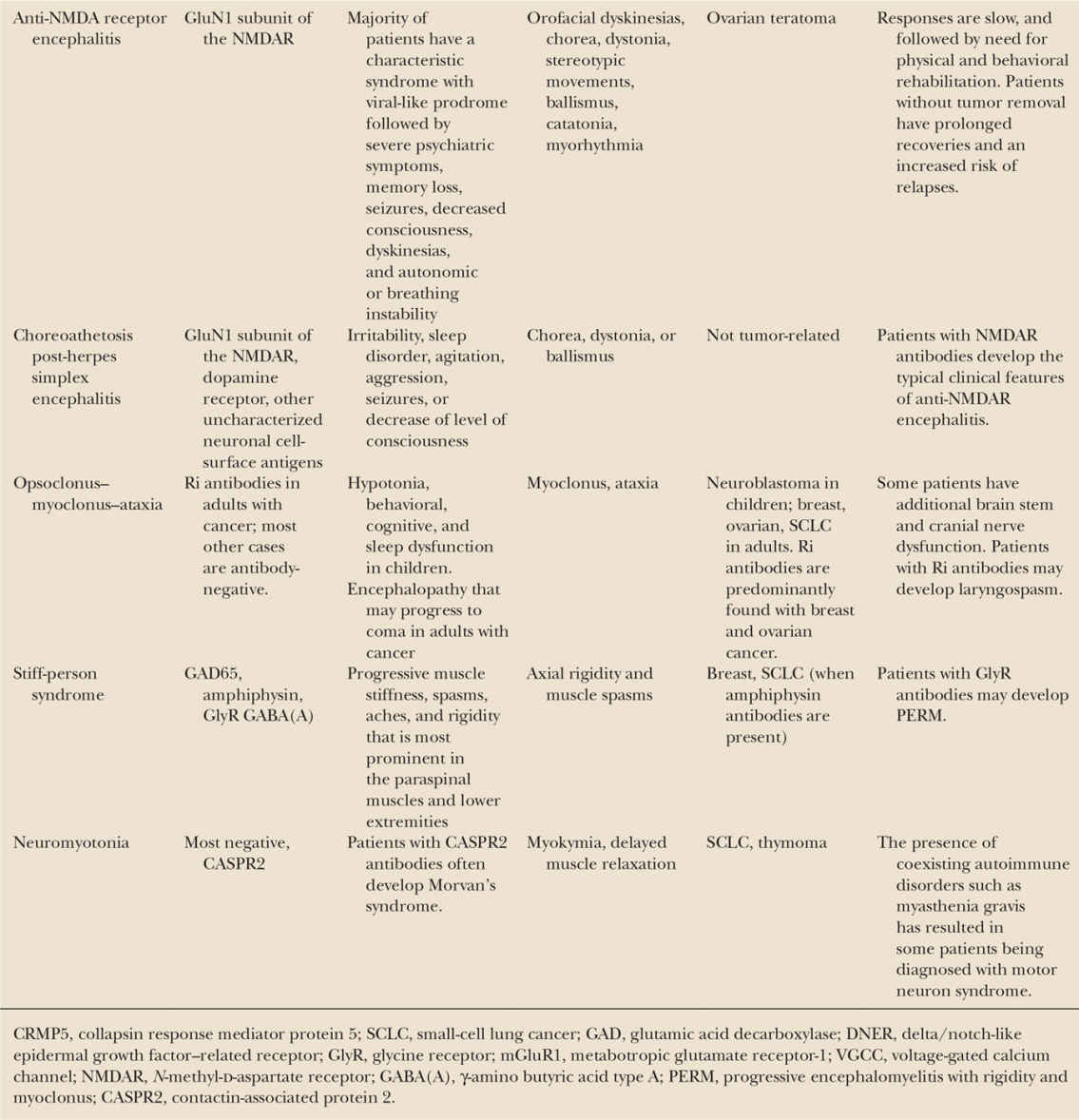
Early recognition that a movement disorder is immune-mediated is important to avoid unnecessary testing. It can also lead to early identification of an underlying cancer, and result in prompt institution of immunotherapies that for some disorders associate with faster and more complete recoveries (12). This chapter reviews several of the more common immune-mediated neurologic disorders that associate with abnormal movements.
CHOREA AND PARANEOPLASTIC ENCEPHALOMYELITIS
Prominent chorea occurs in patients with antibodies to the collapsin response mediator protein 5 (anti-CV2/CRMP5 antibodies) (13). The chorea is part of widespread dysfunction that can include limbic encephalitis, cerebellar ataxia, sensorimotor neuropathy, uveitis, optic neuritis, or retinitis. The most commonly associated cancers are small-cell lung cancer (SCLC) and thymoma. Depending on the extent of the encephalitis, the MRI may show abnormal fluid-attenuated inversion recovery (FLAIR) hyperintense signal involving limbic regions, striatum, basal ganglia, brain stem, and white matter resembling a leukoencephalopathy (14).
The associated neurologic symptoms and MRI findings exclude other causes of chorea such as Huntington’s disease, neuroacanthocytosis, and Wilson’s disease. Inflammatory causes of chorea such as systemic lupus erythematosus or antiphospholipid antibody syndrome may initially be considered in the differential diagnosis as these disorders may present with chorea and other neuropsychiatric symptoms prior to other systemic manifestations. Identification of the associated tumor or serologic screening should clarify the diagnosis.
PSEUDOATHETOID MOVEMENTS AND PARANEOPLASTIC SENSORY NEURONOPATHY
More than 80% of patients with paraneoplastic sensory neuronopathy (PSN) have SCLC, and the neurologic symptoms often develop before the cancer diagnosis has been made (15). PSN may occur in isolation but more commonly precedes or coincides with the development of paraneoplastic encephalomyelitis. The most commonly associated antibody is anti-Hu with some patients having additional antibodies to CV2/CRMP5 or others. All modalities of sensation may be affected, but loss of proprioception often predominates resulting in sensory ataxia and dystonic or pseudoathetoid movements of the extremities, predominantly the hands. Reflexes are usually absent or decreased, and electrophysiologic studies reveal absent or small amplitude sensory potentials with relative preservation of motor conduction velocities. As with most classic PND, PSN is poorly responsive to treatment (tumor and immunotherapy), although rarely a patient will stabilize or have mild improvement (16,17).
HYPOKINESIS AND BRAIN STEM ENCEPHALITIS
Patients with anti-Ma2 antibodies develop limbic and brain stem encephalitis associated with a variety of motor disturbances, including severe hypokinesis, hypophonesis, rigidity, and gaze paralysis (mostly of upward and downward gaze) (18). Patients have forceful jaw opening and closing, and involuntary masticatory movements that result in injuries to the lips and tongue. The brain stem symptoms may progress in a rostral to caudal direction, successively involving cranial nerve nuclei and cerebellar and horizontal gaze pathways. The majority of patients are young men <50 years who almost always have a uni- or bilateral germ-cell tumor of the testis (seminoma or nonseminomatous). Less frequently, the disorder occurs in older patients of both sexes. In these cases, the associated tumors are non-SCLC, breast cancer, colon cancer, and lymphoma. In some patients, the testicular tumor is intratubular and not detectable by testicular ultrasound, body CT, or positron emission tomography (PET); tumor markers can also be negative. The detection of anti-Ma2 antibodies in association with MRI or clinical features compatible with Ma2-encephalitis, life-threatening or progressive neurologic deficits, age <50 years, absence of other tumors, and new testicular enlargement or risk factors for germ-cell tumors should prompt consideration of orchiectomy. The disorder may be confused with Whipple’s disease or progressive supranuclear palsy, and the combination of altered mental status due to limbic encephalitis, rigidity, and dysautonomia may mimic a serotonin syndrome, or neuroleptic malignant syndrome (19). Prompt diagnosis of anti-Ma2 encephalitis is important because up to one-third of patients respond to immunotherapy and tumor treatment. The MRI frequently shows FLAIR/T2 hyperintense signal involving medial temporal lobes, hypothalamus, thalamus, and upper brain stem (20). In contrast to other PND in which the MRI abnormalities rarely enhance after contrast administration, the encephalitis with Ma2 antibodies often shows contrast enhancement (21).
TREMOR, ATAXIA, AND PARANEOPLASTIC CEREBELLAR DEGENERATION
Paraneoplastic cerebellar degeneration is characterized by the subacute development of cerebellar dysfunction. Many patients present with prodromal dizziness and vertigo, often initially attributed to a peripheral vestibular inflammatory process (22). The syndrome progresses within weeks or months, resulting in an incapacitating pancerebellar syndrome with gait, truncal, and limb ataxia, scanning dysarthria and vertical, usually downbeating nystagmus (23). There is often a superimposed tremor of the head that may be constant, and a predominantly kinetic tremor of the extremities. Almost all of the immune-mediated PND may include cerebellar ataxia and tremor as part of the syndrome; however, there are three types of autoimmunity that associate with predominant or pure cerebellar symptoms (predominantly cerebellar ataxia with mild or moderate tremor). Patients with anti-Yo antibodies are typically postmenopausal women, and about 75% have cancer of the ovary and 20% cancer of the breast (22). Patients with anti-Tr antibodies are usually young men with Hodgkin’s or rarely non-Hodgkin’s lymphoma (24). Anti-Tr antibody–associated symptoms may develop before the diagnosis of the lymphoma or when the tumor is in remission. A recent study showed that the target of Tr antibodies is the delta/notch-like epidermal growth factor–related receptor (DNER), which is expressed by cerebellar Purkinje neurons, and is essential for the normal development of Purkinje neurons and Bergmann glia (25). Patients with anti-voltage-gated calcium channel (VGCC) antibodies usually have SCLC, and about half of these patients also have Lambert–Eaton myasthenic syndrome (LEMS) (26). Antibodies against the metabotropic glutamate receptor type 1 (mGluR1) have been identified in a few patients with idiopathic or paraneoplastic cerebellar ataxia associated with Hodgkin lymphoma (27). In general, PCD is poorly responsive to therapy due to early and irreversible loss of Purkinje cells. However, some patients who receive antitumor treatment, with or without immunosuppressive therapy, may stabilize or improve, especially if treatment is started while symptoms are still progressing.
ENCEPHALITIS WITH STEREOTYPED COMPLEX MOVEMENTS AND NMDA RECEPTOR ANTIBODIES
Anti-NMDA receptor encephalitis most commonly occurs in young women and children. Symptoms develop and resolve in a multistage process with most patients experiencing a viral-like prodrome followed by the development of alterations of memory, behavior, cognition, psychosis, seizures, and autonomic instability (12). Movement disorders occur in up to 80% of patients and include oro–bucco–lingual facial dyskinesias, choreoathetoid movements of the limbs, dystonia, rigidity, and opisthotonic postures. The facial movements are described as kissing, pouting, fish- and rabbit-like motions with tongue protrusion and rolling, palatal elevation, grimacing or smiling-like motions, bruxism, and forceful jaw opening and closing asynchronous with tongue protrusion causing tongue and lip injuries (28,29). The limb and other movements are complex, stereotyped, sometimes with rhythmic features, described as pedaling movements of the legs, dancing movements of the arms, piano-playing movements of the hands, and rhythmic contractions of abdominal muscles and pelvic thrusting (30–32). These complex, stereotyped movements usually alternate with periods of catatonia, catalepsy, dystonia, and rigidity and may appear to be seizures, but EEG monitoring does not confirm an epileptogenic basis. Myorhythmia, a rhythmic, slow alternating resting tremor has been described in some children (7).
The diagnosis of anti-NMDA receptor encephalitis is confirmed by the detection of antibodies to the NR1 subunit of the NMDA receptor in serum or cerebrospinal fluid (CSF) (33). After treatment or in the advanced stages of the disease, the CSF antibodies usually remain elevated if there is no clinical improvement, while serum antibodies may be substantially decreased by treatments. The titer of CSF antibodies correlates more closely with clinical outcome (34).
Just over half of patients have an associated tumor, most commonly a mature or immature ovarian teratoma that can be mistaken for a benign cyst. The detection of an ovarian teratoma is age-dependent with approximately half of female patients older than 18 years having uni- or bilateral ovarian teratomas, while less than 9% of girls younger than 14 years have a teratoma. In male patients, the detection of a tumor is rare with about 5% having a tumor, usually a testicular germ-cell tumor.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree