Finding |
Peak Age |
State |
Location |
Frequency |
Duration |
Characteristics |
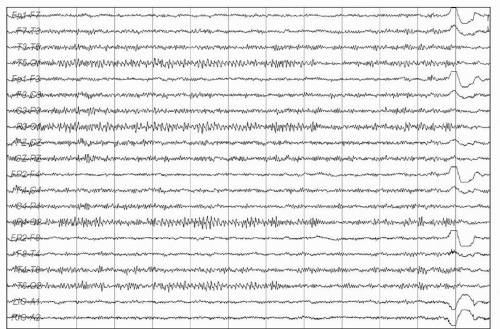
Slow or fast alpha variant |
Children and adults |
Awake, eyes closed |
Occipital |
Half or double the posterior dominant rhythm |
Brief or lasting many seconds |
Sinusoidal, archiform, notched, flat-topped |
Alpha squeak |
Children and adults |
Awake, immediately on eye closure |
Occipital |
Initially fast (beta) slowing rapidly to the posterior dominant rhythm |
Typically 0.5-2 seconds |
Sinusoidal, spindle-shaped |
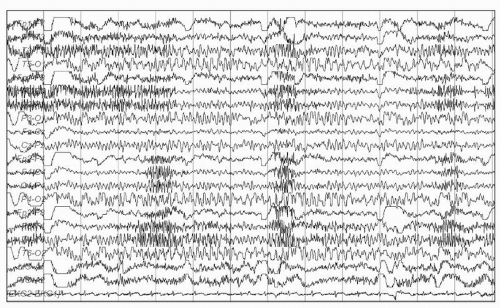
Rhythmic of midtemporal theta bursts of drowsiness (“RMTD”) |
Younger to middle-aged adults |
Drowsiness, light sleep |
Midtemporal, at times with spread to parasagittal or occipital-temporal region
Bilateral or independent over the right or left side |
5-7 Hz |
Several seconds, or up to a minute or more |
Arched, notched, flat-topped
Notche may give the waves a sharply contoured appearance |
Midline theta rhythm (“Cigánek rhythm”) |
Children and adults |
Common in drowsiness and during mental activation. Less common in resting wakefulness |
Midline (CZ, FZ), parasagittal |
4-7 Hz |
Brief or lasting many seconds |
Arched, notched, flat-topped |
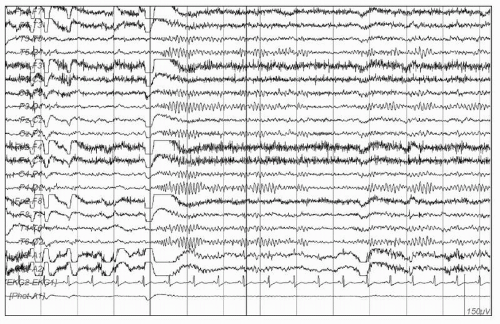
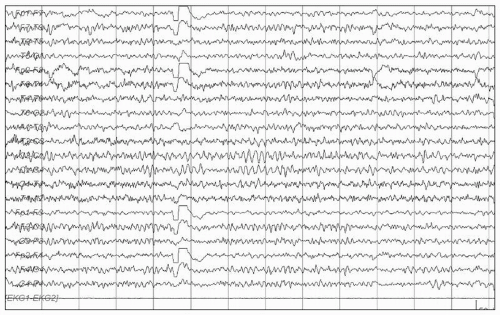
Subclinical rhythmic electrographic discharge in adults (SREDA) |
Adults, mostly age 40s-80s (mean 60s) |
Drowsiness and resting wakefulness (rare cases reported in sleep) |
Maximal in temporal and parietal regions
Usually bilateral, but may be asymmetric |
May begin with delta frequency, but then increases to 4-7 Hz |
Brief or lasting minutes |
Sharply contoured, archiform, notched, flat-topped |
14- and 6-Hz positive bursts |
Childhood and adolescence |
Drowsiness, light sleep |
Posterior temporal |
14 or 6 Hz |
0.5-1 second |
Archiform, comb-like, low amplitude |
6-Hz spike and wave bursts |
Children and adults |
Drowsiness, light sleep |
Highest amplitude over fronto-central regions |
5-6 Hz |
1-2 seconds |
Usually low-amplitude (<25 µV) and short-duration (<30 msec) spike component |
Benign sporadic sleep spikes |
Mainly in adults. Also reported in children and adolescents |
Drowsiness, light sleep |
Anterior and midtemporal |
Sporadic |
Usually < 50 msec |
Mono- or diphasic spike with steep descending arm |
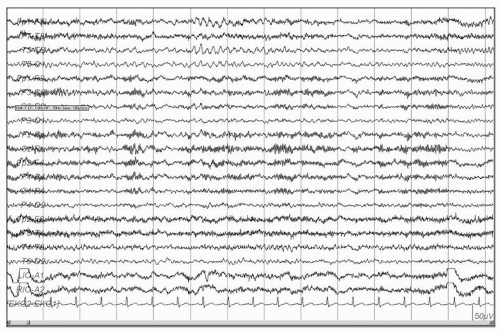
Wickets |
Adults |
Awake, sleep |
Temporal regions |
6-11 Hz if they occur in runs |
Average of 2-4-second bursts in sleep |
Archiform, monophasic |
Frontal arousal rhythm |
Children |
Awakening, arousal from sleep |
Frontal |
6.5-8.5 Hz |
Up to 13 seconds |
Monomorphic |