CHAPTER 172 Percutaneous Cordotomy and Trigeminal Tractotomy-Nucleotomy
History
The first discoveries of the anatomy and function of the spinal cord in clinical and experimental studies were accomplished by Galen in the 2nd century AD.1,2 Further clinical suggestions about the function of the spinal cord emerged from empirical observations. In 1871, Müller reported a patient in whom isolated analgesia was observed after lesioning of the spinal cord.3 A few years later, Gowers reported a case of localized injury to the anterolateral column at the level of the third cervical segment that resulted in complete analgesia with preservation of tactile sensation on the opposite half of the body. Gowers concluded that the afferent pathway for pain was located in the anterolateral column.3 The spinothalamic tract was first identified by Edinger in 1889 while conducting experiments on amphibians and newborn cats. In 1905, Spiller reported that pain and temperature sensation ascends in the anterolateral spinal cord based on autopsy findings in patients with tuberculoma at the thoracic level of the spinal cord.4 Schüller sectioned the anterolateral tract in monkeys in 1910 and termed the procedure chordotomie.5 The first cordotomy in a human was carried out by Martin at Spiller’s instigation, and numerous technical difficulties were encountered.6 In 1920, Frazier published a series of six patients who underwent cordotomy, five of whom experienced postoperative pain relief.7 After this publication, cordotomy was accepted as an important type of intractable pain–relieving procedure. Since its first description, open cordotomy has usually been performed via the posterior approach. The anterior approach was described by Collis and Cloward but has not been widely used because of inherent technical difficulties.8,9
Denervation of the craniofacial region by sectioning of a special pain-conducting pathway was first described by Olof Sjöqvist in 1938.3 He sectioned the tractus at the inferior olive level in an open technique via craniectomy in the posterior fossa. In 1942, White and Sweet observed hypoalgesia after trigeminal tractotomy in the innervation area of the 7th, 9th, and 10th cranial nerves.10 Sweet then used this procedure for the treatment of glossopharyngeal neuralgia. Kunc performed selective tractotomy 12 mm above the second cervical root level, which successfully relieved glossopharyngeal neuralgia.11
Cordotomy and tractotomy are performed mostly in (cancer) patients with poor health status who cannot tolerate open surgery. Clinicians have labored for years to develop noninvasive treatments in an effort to accommodate this patient subgroup. Percutaneous cordotomy and tractotomy are relatively new treatment modalities performed with a needle electrode system and, conventionally, radiographic guidance. Cordotomy was first described and performed by Mullan and colleagues in 1963 with a radioactively tipped strontium needle.12 Because of undesirable effects of the radioactive source, Mullan and coworkers began making unipolar, anodal electrolytic lesions in 1965.13 In the same year, Rosomoff and associates described the technique of percutaneous cordotomy with a radiofrequency (RF) electrode system, which facilitated making a small, discrete lesion in the pain-conducting system of the spinal cord.14 With the help of impedance measurements and stimulation, evaluation of the target’s neurophysiologic function became possible. The percutaneous method was performed in the lower cervical region via an anterior approach by Lin and coworkers in 1966.15
In 1967 and 1968, Crue and colleagues and Hitchcock independently developed a percutaneous technique using RF thermocoagulation and performed the first stereotactic trigeminal tractotomies.16,17 Trigeminal tractotomy was used for the treatment of postherpetic facial pain in 1972 by Hitchcock and Schvarcz.18 Schvarcz also used the same procedure to create lesions primarily in the second-order neurons at the oral pole of the nucleus caudalis at the level of the occipitocervical junction19 and termed this procedure trigeminal nucleotomy.20
Radiography, the conventional visualization system in stereotactic pain procedures, cannot demonstrate a patient’s spinal cord morphology. In 1988, Kanpolat and coauthors published the first experience with computed tomographic (CT) visualization in a stereotactic pain procedure and later used CT guidance as a visualization method for percutaneous cordotomy.21,22 CT visualization offers the advantage of topographic orientation. Using this contribution, Kanpolat and colleagues described selective unilateral and bilateral cordotomy and trigeminal tractotomy in the following years.23,24 Morphologic orientation and neurophysiologic evaluation of the target allowed the use of this truly stereotactic method with RF energy. CT-guided application of trigeminal tractotomy was described and published in 1989.25 These procedures define the concept of CT-guided destructive procedures in classic percutaneous pain surgery.
Anatomy of the Targets and Their Environs
Computed Tomography–Guided Percutaneous Cordotomy
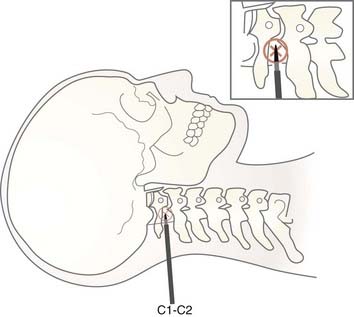
Morphometric studies of the spinal cord at the level of the surgical approach (C1-2) provide the most critical information pertaining to anatomic orientation for cordotomy. At the C1-2 level, the diameters of the spinal cord were reported by Mullan as being 10 mm anteroposteriorly (AP) and 13 mm transversely (T).26 We measured the spinal cord diameters of 63 patients who underwent CT-guided percutaneous cordotomy at the C1-2 level as being 7.0 to 11.4 mm (AP) (mean, 8.66 ± 0.72 mm) and 9.0 to 14.0 mm (T) (mean, 10.9 ± 1.56 mm).27 Kameyama and associates found spinal cord diameters at the C2 level to be 6.4 ± 0.4 mm (AP) and 10.5 ± 0.8 mm (T). These values were 6.0 ± 0.4 mm (AP) and 12.2 ± 0.8 mm (T) and 5.5 ± 0.5 mm (AP) and 10.6 ± 0.7 mm (T) at the C5 and T1 levels, respectively.28 In contrast, Poletti found the transverse diameter of the spinal cord of a cancer patient at the T2 level to be 5.2 mm.29
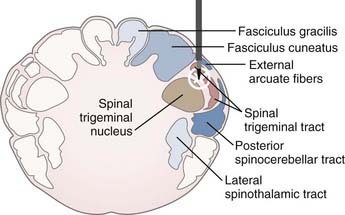
The target in cordotomy is the lateral spinothalamic tract, which is located in the anterolateral part of the spinal cord (Fig. 172-1).10,30–32 This ascending tract primarily carries information about pain and temperature and relays some tactile information. The distribution of the pain-conducting fibers within the anterolateral spinal tract is such that the small, ventrally located fibers generally conduct pain sensation. The organization of fibers from the outside inward is superficial pain, temperature, and deep pain.33 Because most of the fibers in the anterolateral system decussate over two to five segments before entering the anterolateral columns, spinothalamic cordotomy aims to interrupt the spinothalamic tract ascending contralaterally to the painful side. Although the majority of pain-transmitting fibers decussate normally, the rate and position of decussated axons may vary considerably among individuals; thus, unilateral cordotomy can, on rare occasion, produce ipsilateral analgesia in some individuals because of nondecussated neurons.10
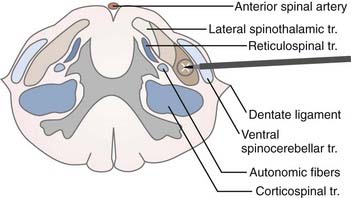
FIGURE 172-1 Schematic representation of the target (lateral spinothalamic tract) and its environs at the C1-2 level.
The anterolateral sensory system has a somatotopic relationship, with fibers from higher levels laminating medially and ventrally and fibers from lower levels laminating laterally and dorsally within the lateral spinothalamic tract.30,31,33 In 1926, Peet stated that deeper cordotomy incisions, particularly in the anterior portion of the anterolateral tract, cause analgesia in the upper parts of the body.32 In 1939, Hyndman and Van Epps suggested the possibility of producing high-level analgesia with preservation of pain and temperature sensibility in the lower half of the body.30 Segmentation of the fibers provides the opportunity for selective cordotomy, given that anteromedial lesions denervate the contralateral arm and upper chest region whereas posterolateral lesions denervate the sacral and lumbar area (Fig. 172-1).
The pyramidal tract is usually located posterior to the dentate ligament. It must be remembered, however, that in rare instances the dentate ligament is posterior to its normal location.10 Moreover, there is considerable variation in the size and location of the ventral corticospinal tract; for instance, it sometimes fails to decussate at all. Because motor decussation may extend from the obex to the C1 level, contralateral leg weakness may also occur if the lesion is too high.33 The ventral spinocerebellar tract is located in the lateral part of the lateral spinothalamic tract. Lesions of this tract cause ipsilateral ataxia of the arm. Autonomic fibers related to bowel and bladder function are found in the lateral part of the lateral horn of the gray matter. Immediately posterior to the autonomic fibers are vasomotor fibers, bilateral lesioning of which causes hypotension.33
The most important region related to the practice of upper cervical cordotomy is the medial aspect of the lateral spinothalamic tract, where the descending respiratory pathway is located. Nathan emphasized the importance of this region as follows: “The descending respiratory pathway may be considered to be the most important tract of the spinal cord; yet its position in man is unknown. It is important to work out the location of these descending fibers not only to complete anatomic knowledge but also to provide those practicing surgery on the cervical cord with essential information. The absence of this knowledge contributed to the death of some of our patients after cordotomy and this has also been a cause of death in patients from other series of cordotomies.”34 Belmusto and colleagues concluded that fibers associated with respiration in humans occupy an area from C1 to C3, 3.0 to 5.5 mm from the lateral margin of the cord.35 Hitchcock and Leece suggested that the anterior portion of the respiratory tract is largely related to diaphragmatic function whereas the posterior portion supplies the remainder of the respiratory musculature—namely, the intercostal muscles, as well as the abdominal and lumbar musculature used in respiration.36
Computed Tomography–Guided Percutaneous Trigeminal Tractotomy-Nucleotomy
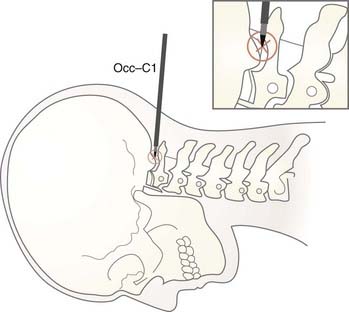
CT-guided percutaneous trigeminal tractotomy-nucleotomy (TR-NC) is performed at the occiput-C1 level. Upper spinal cord diameters at this level were measured in 30 patients. Anteroposterior measurements were 7.0 to 12.8 (mean, 9.13 ± 0.83), and transverse diameters were 9.3 to 14.0 mm (mean, 11.6 ± 0.76).27
Trigeminal afferent fibers, which carry the sensations of pain and temperature, enter the pons and send a caudal branch (the descending trigeminal tractus) into the medulla. The descending trigeminal tractus overlies the spinal trigeminal nucleus in the posterolateral part of the spinal cord at the cervicomedullary junction. Primary sensory fibers from the 7th, 9th, and 10th cranial nerves also enter the descending tractus of the trigeminal nerve.37,38 The three divisions of the trigeminal nerve have a special topographic organization in the descending tractus of the nerve. Fibers from the 7th, 9th, and 10th cranial nerves lie slightly medially behind the tractus; trigeminal afferents that carry the sensations of pain and temperature, unlike other sensory modalities, descend in the spinal trigeminal tractus and enter the nucleus.39 The spinal trigeminal nucleus has three distinct subdivisions along its pontospinal extent: (1) the nucleus oralis, located rostrally between the pons and medulla; (2) the nucleus interpolaris, located interomedially; and (3) the nucleus caudalis, located at the medullospinal junction and extending down to the C2 segment level. The nucleus caudalis represents the substantia gelatinosa, and there is extensive overlap between the facial and high cervical afferents, where the 7th, 9th, and 10th cranial nerve afferents also end. Destruction of the oral pole of the nucleus caudalis plays a special role in pain relief.40
There is a topographic representation of the ipsilateral face on the spinal tractus of the trigeminal nerve; that is, the most central areas of the face terminate highest on the nucleus caudalis, whereas the most peripheral areas of the face end lowest.37,41
The target in tractotomy is located in the posterolateral part of the spinal cord. At this point, the descending trigeminal tractus is located in the lateral part and the nucleus caudalis in the median part. For this reason, during lesioning, the tractus as well as the oral part of the nucleus caudalis are destroyed. The procedure was designated TR-NC in view of this relationship (Fig. 172-2).
Patient Selection
Cordotomy
Cordotomy is the preferred method if the surgeon is certain that the patient’s intractable pain is transmitted in the lateral spinothalamic tract (see Figs. 172-1 and 172-3). The best candidates for cordotomy are patients with unilateral nociceptive somatic cancer pain and compression of the plexus, roots, or nerves.42 Tasker defined two types of pain as indications for cordotomy: (1) intermittent, neuralgia-like, shooting pain into the legs associated with a spinal cord injury, which is typically at the thoracolumbar level, and (2) evoked pain, allodynia or hyperpathia, associated with neuropathic pain syndromes that arise from peripheral neurological lesions.42,43
In our practice, percutaneous cordotomy is generally preferable. Open cordotomy is recommended if the necessary equipment is not available or the surgeon’s experience is inadequate to perform percutaneous cordotomy. The presence of any anomalies or other diseases of the upper cervical region would also be an indication for open cordotomy.42
Contrary to popular opinion, unilateral upper body pain (secondary to lung carcinoma, mesothelioma, or Pancoast’s tumors) and bilateral somatic intractable pain in the lower part of the body and extremities can be controlled by CT-guided, unilateral or bilateral selective cordotomy.23,24 Standard practice is to use neurodestructive procedures only after narcotic analgesics prove inadequate.44,45 Gybels proposed infusing opioid into cerebrospinal fluid (CSF) and performing percutaneous neurolytic procedures instead of percutaneous cordotomy if the patient has only a 2- to 5-month life expectancy.46 At present, with the help of imaging techniques and the recent contribution of electrode technology, cordotomy can be performed safely and effectively. Thus, CT-guided percutaneous cordotomy should be considered the treatment of choice even before morphine therapy.23,24 I believe that the new version of percutaneous cordotomy is a simple, safe, and preferable procedure, especially for intractable pain states in malignancy, to stop patient dependence on pumps, stimulation systems, drugs, and doctors. Percutaneous cordotomy provides a rare opportunity to improve patients’ quality of life in their final and most difficult stages.
Cordotomy is contraindicated in patients with severe pulmonary dysfunction, those who are unable to stay in a supine position for 30 to 40 minutes, and patients whose oxygen saturation is less than 80%. For patients with bilateral intractable pain of the chest and arms, bilateral high cervical cordotomy is not recommended. For this group, the anterior approach must be used—open or percutaneous and unilateral or bilateral.23,24,42,47,48
Percutaneous Trigeminal Tractotomy-Nucleotomy
Trigeminal tractotomy-nucleotomy is based on the destruction of descending trigeminal tractus and nucleus caudalis at occiput-C1 level (Figs. 172-2 and 172-4). Trigeminal tractotomy or nucleotomy procedures, or both, are used for pain denervation in selected cases: cancer pain and deafferentation pain, atypical facial pain (AFP), atypical trigeminal pain, chronic cluster headache, and vagoglossopharyngeal and geniculate neuralgias located not only in the area of the 5th nerve but also in the area of the 7th, 9th, and 10th nerves and nucleus caudalis.16,19,49–55 AFP is a throbbing pain situated deep in the eye and malar region that often radiates to the ear, neck, and shoulders. The pain is not generally within any dermatomal or anatomic boundaries. AFP and psychological pathologies such as depression are strongly associated, and anxiety is known to exacerbate the condition. The term atypical is used to distinguish facial pain from trigeminal neuralgia because this pain syndrome is neither responsive to anticonvulsant drugs nor present in the sensory area of the trigeminal nerve.56 Some neurosurgeons do not recommend surgery for these patients, but we still accept patients if referred by psychiatrists for intractable AFP.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree