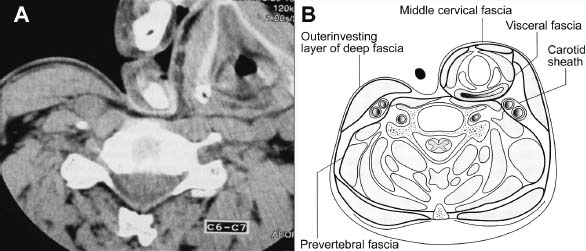
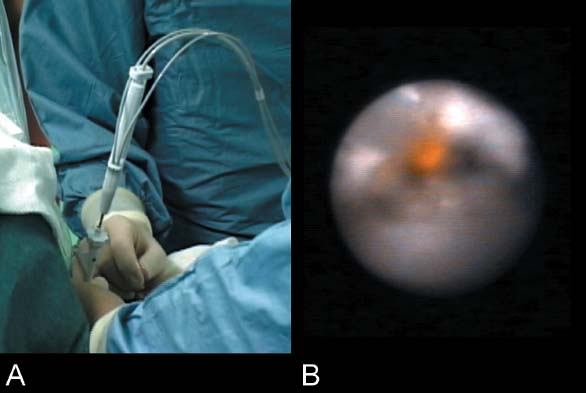
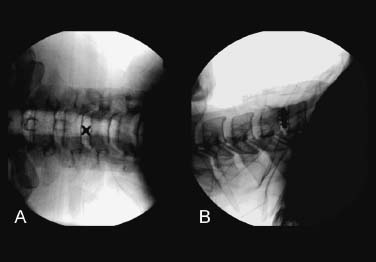
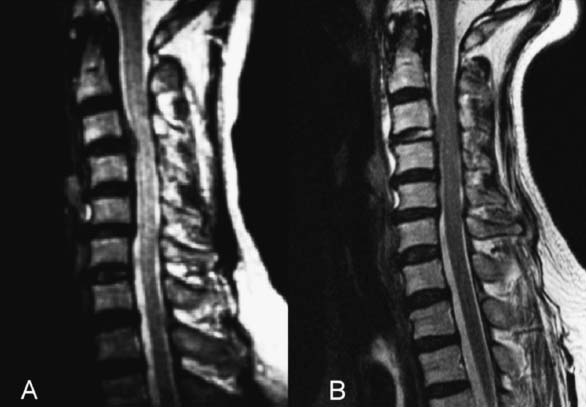
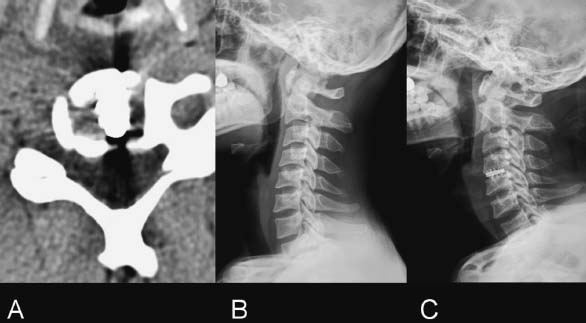
Percutaneous endoscopic cervical diskectomy (PECD) is a new surgical method for treating soft cervical disk herniations. The goal of the procedure is decompression of the spinal nerve root by percutaneous removal of the herniated mass and shrinkage of the nucleus pulposus under local anesthesia. The anterior interbody fusion, achieved by removing the intervertebral disk and inserting a bone graft under general anesthesia, remains the mainstay of surgical treatment for cervical disk herniation. The open anteromedial diskectomy with fusion, however, usually requires entrance into the spinal canal, with the accompanying risk of such complications as epidural bleeding, perineural fibrosis, transient or permanent myelopathy, graft-related problems (e.g., donor site morbidity, painful pseudarthrosis, graft extrusion or angular collapse, kyphotic deformity, graft impaction into the body), dysphasia, and hoarseness (e.g., temporary or permanent vocal cord paresis).1–7 The minimally invasive PECD under local anesthesia can avoid these complications and offers an alternative to open therapeutic methods in cervicobrachial neuralgia or radiculopathy due to soft cervical disk herniation. It has already undergone successful biomechanical tests and cadaveric studies. In cases of failure, PECD does not impede conventional surgical approaches, and it offers such numerous advantages as the absence of risk of epidural bleeding and periradicular fibrosis, maintenance of stability of the intervertebral mobile segment, and reduced risk for recurrence after performing an anterior diskal window. The procedure provides an excellent cosmetic effect, and the reduced operation time and hospital stay allow the patient to recover to normal daily activity more rapidly. Although PECD provides an effective and attractive alternative to open diskectomy and fusion, it has limitations. For example, PECD is ineffective in the presence of segmental instability or cervical discogenic pain syndromes. Spinal stabilization performed by conventional open procedures, however, often requires an extended pathway through the neck to insert the fusion/spacer devices into the disk space. Specially designed expandable holders can be used as interbody spacers to achieve stability without open diskectomy fusion, thus avoiding many approach-related complications seen with open techniques. History Since its first description of cervical percutaneous diskectomy by Tajima et al., there has been a remarkable evolution of various minimally invasive techniques for cervical disk disease. These include such percutaneous cervical diskotomy (PCD) as chemonucleolysis using chymopapain,9 automated percutaneous cervical diskectomy (APCD),10–12 the combination of chymopapain injection followed by APCD,13 and laser percutaneous cervical decompression (LPCD),14–17 all of which are well established. We have performed PECD with cervical laser-assisted spinal endoscopy (LASE) since 1993. Indications Most patients with cervicobrachial neuralgia due to disk herniation respond well to medical treatment; however, symptoms related to perineural cicatricial fibrosis due to a prolonged pressure on the nerve root can become irreversible. The occurrence or aggravation of a neurologica deficit even after an adequate period of conservative treatment therefore requires one to consider surgical decompression. PECD is indicated in the surgical treatment of soft cervical disk herniation contained by the posterior longitudinal ligament (subligamentous protrusion) and confirmed by magnetic resonance imaging. If the radicular symptoms are aggravated with neck extension and reduced by flexion of the neck, and if rotating the head toward the affected extremity and compressing the vertex of the head reproduce symptoms, whereas abduction of the shoulder and elevation of the head bring relief of symptoms, it is a good indication for PECD. Cervicoencephalic symptoms (e.g., headache and dizziness lasting for more than 1 year due to soft cervical disk herniation) diagnosed by diskography are also a good indication for PECD. A very bulky hernia is not a contraindication as long as the patient has no myelopathic symptoms and signs. Stabilization after diskectomy is considered in all patients with cervical instability and cervical discogenic syndromes. Contraindications PECD is contraindicated in patients presenting a severe neurologic deficit, segmental instability, acute pyramidal syndrome, progressive myelopathy, and other pathological conditions (e.g., fracture, tumor, pregnancy, and active infection). Instruments and Equipment The oldest working tube Tajima et al. made in 1981 was 2 mm in diameter and 8 cm in length. He added two dilators, one guide needle for diskography, and three disk forceps (i.e., small, medium, and large). The small forceps (disk rongeur) was principally utilized for excision of osteophytes. Using medium and large forceps, Tajima et al. performed diskectomy of the posterior disk. These instruments might be broken inside the disk.8 The revised instruments required for PECD include an 18-gauge spinal needle, a thin guidewire, dilating obturators, working cannulas, an anulus trephine, and various forceps with or without an irrigation hole (Fig. 6–1). Visual control of percutaneous diskectomy is possible intermittently with a small, rigid endoscope and continuously with a flexible endoscopic holmium: yttrium-aluminum-garnet (YAG) laser kit or working endoscope (cervical LASE) (Fig. 6–2). The procedure should be performed only after a clear view of the entire operative disk under lateral and anteroposterior (AP) fluoroscopic projection has been obtained. The operating table must be radiolucent. Equipment for general anesthesia and instruments for open anterior cervical diskectomy with fusion should be prepared in case of a need for conversion to an open procedure or for the rare occasion of airway obstruction due to hematoma. FIGURE 6–1 Instruments for percutaneous endoscopic cervical diskectomy WSA: 1 and 2 mm dilators; 3, 4, and 5 mm working tubes; forceps; and an annular trephine. Preparation and Anesthesia Preoperative antibiotics (i.e., usually cefazolin 1.0 g) should be given to decrease the risk of infection. Preoperative sedatives are recommended. PECD must be performed in an operating room with strict asepsis. The patient is placed in a supine position, with the neck mildly extended on a radiolucent table. The forehead must be fixed with plaster. A pillow is put under the shoulder and neck. The shoulders are sloped down with a plaster fixed on the table. The C-arm of the fluoroscope is put in front, then in profile, and the area of the operation is carefully marked on the skin with a felt pen using a metal instrument on the front and profile. The lesion is marked by counting the cervical vertebrae downward, then up from the bottom. For better visualization of the C6–C7 level, a slight slope of the fluoroscope may be necessary. The felt pen marks the internal edge of the sternocleidomastoid muscle, the median axis of the neck, and the upper edge of the sternum. The skin is distempered with an antiseptic. The fluoroscope is covered with a sterile field, then the face is surrounded with a plastic field that is held up over the patient’s head in order for an anesthesiologist to observe and speak with the patient. Communication between the operator and the patient is necessary during the procedure. The operation is typically conducted under local anesthesia and analgesia by neuroleptics so the surgeon may know immediately any changes in symptoms and signs of the patient. General anesthesia may be used in a few patients who want it or cannot tolerate the position. If the cervical diskography or other procedures aggravate the spinal cord compression, patients can recognize and comment on the development of extremity weakness only under local anesthesia. Under general anesthesia, the urgent need for conversion to open surgery may not be detected early. A solution of 1% lidocaine is usually used to infiltrate the skin and subcutaneous tissue. To minimize the thickening of underlying tissues and to allow a minute palpation of the spinal axis, we prefer not to infiltrate more deeply with lidocaine. FIGURE 6–2 WSH cervical LASE (laser-assisted spinal endoscopy) system for percutaneous endoscopic cervical diskectomy. FIGURE 6–3 (A,B) Axial MRI and drawing after pushing trachea with a finger showing a clear way toward cervical disks. Surgical Technique Needle Insertion The surgeon gently pushes the trachea or larynx toward the opposite side with the index and middle finger, then applies a firm pressure in the space between the muscle and trachea and pointed toward the vertebral surface (Fig. 6–3 A,B). The trachea and larynx are displaced medially and the carotid artery laterally. The puncture needle is then inserted through the space between the tracheoesophagus and the carotid artery (Fig. 6–4). The tip of the needle should be positioned on the center of the anterior anulus. The position is confirmed fluoroscopically, and the needle is advanced ~5 mm into the disk. Intraoperative diskography is performed to identify the herniation type or annular tear. Up to 0.5 ml of contrast media is injected to specify the posterior part of the disk. A guidewire is then inserted to replace the puncture needle. A small skin incision (>5 mm) is made. FIGURE 6–4 An 18-gauge needle is shown between the operator’s and the assistant’s index fingers. The operator’s and/or the assistant’s index finger pulls the trachea to allow the other finger to touch the anterior surface of the cervical spine. FIGURE 6–5 The position of the forceps tip. Working Cannula Insertion After skin incision, the surgeon inserts 1 to 5 mm dilation cannulas sequentially along the guidewire. It is safer to dilate the insertion site gradually. Before insertion of the final working cannula, the anterior anulus is cut by an annulotomy trephine. The final working cannula is then inserted into the disk space, and its position is confirmed by C-arm fluoroscopy. Depending on the disk space height, working cannulas of diameters from 3.0 to 5.0 mm are useful. FIGURE 6–6 (A) The endoscopic holmium: yttrium-aluminum-garnet laser. (B) Endoscopic view of disk ablation by laser. Manual Diskectomy The next step is manual diskectomy under C-arm guidance. The surgeon cuts the anterior anulus as a small hole using the annulotomy trephine, then decompresses the posterior disk widely. The surgeon can thus preserve most of the anterior structures (unlike in the open diskectomy). The forceps are used to remove the nucleus. It should be reached at the end of the posterior margin to remove the herniated mass effectively, with care taken not to injure the spinal cord (Fig. 6–5). The medial nucleus is removed first, then the lateral side according to the position of the lesion. Extraction of the tail of the hernia mass, which is more fibrotic and collagenous, is attempted. The anterior part of the disk should not be removed to avoid postoperative kyphosis. The intradiskal space is rinsed continuously with cefazolin-mixed fluid through an irrigation channel in the forceps. Endoscopic Laser Diskectomy After removal of the hernia mass by forceps, a sophisticated laser decompression is performed using the holmium:YAG laser. The endoscopic holmium:YAG laser works precisely with a 0.3 to 0.5 mm cutting depth for direct ablation and shrinkage of the disk (Fig. 6–6A). Continuous saline irrigation is performed to protect the spinal cord or nerve root from energy transmission. To ablate the tissue near or inside the hernia mass, the surgeon should see inside the disk with a small endoscope (Fig. 6–6B). Furthermore, pumping irrigation with saline during the operation has an antibacterial effect; we have observed no diskitis at all so far. FIGURE 6–7 (A) Initially narrowed form of cervical expandable holder (3.3 mm). (B) Expanded form (5/7/7/6 mm). Stabilization with Expandable Holder The expandable spinal fusion system, which can be applied by this less invasive technique, allows for spinal stability with minimal tissue dissection. The implant is introduced into the intervertebral space in a narrowed form (Fig. 6–8A). It requires an opening less than 5 mm at the skin entry site. Following the insertion of the implant into the disk space, the implant is expanded to its final form segment by segment by rotating the expander rotational handle (Fig. 6–8B). It is then fixed to the disk space to maintain the disk height (Fig. 6–9). FIGURE 6–8 (A,B) Intraoperative C-arm view of fixed cervical expandable holder at C5–C6. FIGURE 6–9 (A,B) Magnetic resonance imaging showing good shrinkage of soft disk herniation after percutaneous endoscopic cervical diskectomy. The surgeon should recognize and manually feel the pulsation of the carotid artery to insert the needle and cannula away from the carotid artery. The surgeon should confirm the position of a needle or a cannula on the AP fluoroscopic view to prevent penetration of the vertebral artery. The fingertips of the operator or the assistant should touch the anterior surface of the vertebral body to avoid perforating the trachea or esophagus. The surgeon should confirm the tip of the guidewire, the annular trephine, the pituitary forceps, and the laser fiber on the lateral fluoroscopic view, so that the ends of the instruments do not pass more than 2 mm beyond the posterior vertebral body line to protect the spinal cord. The disk space should be irrigated frequently with 1000 ml saline mixed with antibiotics to reduce the chance of diskitis or epidural abscess. Postoperative Management The patient should be observed for 3 hours to detect possible complications. All patients are permitted to go home on the day of surgery (it is an outpatient surgery). The patient does not need bed rest for more than 1 night. Postoperative oral antibiotics and analgesics are recommended for 3 to 10 days. A cervical collar is recommended for 3 to 14 days, depending on the patient’s condition. Mild physical therapy may be helpful for fast recovery within 2 weeks postoperatively if cervicobrachialgia does not disappear completely. Should pain and discomfort remain, complementary epidural injection of steroids with lidocaine may be added so that no further open procedure is necessary. This is a combined therapeutic logic of mechanical decompression with PECD and the reduction of inflammatory components by steroids.9 Rehabilitation exercises for neck muscle strengthening and improvement of range of motion are recommended twice a week for 3 months after 4 to 6 weeks postoperatively. FIGURE 6–10 (A) Postoperative computed tomography. (B,C) Restoration of normal lordotic cervical alignment after surgery. Clinical Results Between 1993 and 2002, a total of 1127 patients were treated by PECD at Wooridul Spine Hospital (Seoul, Korea). Most patients experienced immediate improvement of their pain during the procedure. Immediate postoperative magnetic resonance imaging (MRI) demonstrates that the disk herniation is removed completely (Fig. 6–9). We conducted a retrospective study with 113 patients selected randomly at 3 years after PECD. All of the 113 patients were followed by MRI and computed tomographic (CT) scans. Ninety-eight patients (86.7%) presented radiculopathies. Neck pains were noticed in 67 patients (59%), headache and dizziness in 13 (12%), and mild myelopathy in 5 (4.4%). The mean duration of symptoms was 24 months (range: from 1 to 300 months). The locations of herniation were paramedial in 48 patients (42%), central in 31 (27%), foraminal and lateral in 22 (19%), and diffuse in 13 (12%). Excellent or good results were shown in 94 patients (83%), fair in 13 patients (11%), and poor in 6 (5%) according to Macnab criteria.18 Two cases (1.8%) needed open diskectomy; one had worsened neck pain after PECD and underwent anterior cervical diskectomy with fusion, and the other had worsened shoulder and arm pain and underwent anterior cervical foraminotomy. There were no complications (e.g., esophageal, vascular, or nerve injuries), infection, or cerebrospinal fluid leakage. Since 2001, seven patients underwent the PECD and stabilization with an expandable holder. All patients had remarkable relief of pain after the procedure. Postoperative CT scans showed satisfactory positioning of the implant (Fig. 6–10A). Preoperative kyphotic alignment improved postoperatively (Fig. 6–10B and C). There were no procedure-related complications. Minimally invasive techniques combining the percutaneous C-arm-guided manual diskectomy and endoscopic holmium:YAG laser diskectomy to treat soft cervical disk herniations with radiculopathy have proven to be conservative and not destructive. The clinical results were comparable to those obtained with open diskectomy and fusion. The PECD is an outpatient surgery and can be as safe and efficacious as open anteromedial cervical diskectomy in select patients. Stabilization following PECD can be performed safely and effectively in cases of soft cervical disk herniations with segmental instability or discogenic neck pain. REFERENCES 3. Clements DH, O’Leary PF. Anterior cervical diskectomy and fusion. Spine. 1990;15:1023–1025. 4. Flynn TB. Neurologic complications of anterior cervical interbody fusion. Spine. 1982;7:536–539.
6

Percutaneous Endoscopic Cervical Diskectomy and Stabilization






< div class='tao-gold-member'>
Percutaneous Endoscopic Cervical Diskectomy and Stabilization
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








