Chapter 4
Peripheral Laryngeal Motor Innervation
The laryngeal functions of respiration involve baseline, unconscious input from the brainstem, as well as rapid, reflexive responses to sensory receptors from the pulmonary system. Deglutination and airway protection similarly require highly reliable responses from the brainstem and sensory system. Phonation requires rapid adduction and abduction as well as fine control of cord tension for pitch adjustments.1 In addition, high tensile strength is needed to resist the forces produced at the vibratory margin of the vocal fold. The laryngeal muscles and nerves are adapted to be rapid, reliable, and highly resistant to fatigue. Anatomic dissection and histologic analysis have revealed several specialized features of the motor innervation system in the intrinsic larynx that differ markedly from other skeletal muscles groups.
Nerve Anatomy
Recurrent Laryngeal Nerve Anatomy
The recurrent or inferior laryngeal nerve (RLN) and the superior laryngeal nerve (SLN) are responsible for the motor function of the larynx. These nerves carry a mixture of motor and sensory fibers from the brainstem. The vagus nerve is supplied by four nuclei within the medulla: the nucleus ambiguus, the nucleus of the tractus solitarius, the dorsal nucleus of the vagus, and the sensory nucleus of the trigeminal nerve.
The nucleus ambiguus is the source of motor innervation carried to the RLN via the vagus nerve to the larynx. Within the vagus, the laryngeal motor axons are located in the anterior aspect of the trunk superiorly. It rotates medially as the vagus nerve trunk descends the neck. The vagus leaves the jugular foramen anterior to the jugular vein, but as it descends within the carotid sheath, it assumes a posterior position. The left RLN loops under the aorta before beginning its ascent along the tracheoesophageal groove to enter the larynx at the cricothyroid membrane. The right RLN has a shorter course and loops underneath the right subclavian artery. The right RLN is approximately 5 to 6 cm in length, whereas the left RLN is approximately 12 cm. As the RLN enters the larynx, it divides into motor and sensory branches to innervate the laryngeal muscles and carry sensory information from the subglottis.2
Superior Laryngeal Nerve
The anatomic course of the SLN is more variable than that of the RLN. The SLN originates from the nodose ganglion and then travels with the vagus nerve. The external branch of the SLN (EBSLN), which carries the motor fibers to the cricothyroid (CT) muscle, separates from the vagus nerve via the superior laryngeal nerve approximately 4 cm above the bifurcation of the common carotid. The larger internal branch of the SLN carries primarily sensory fibers from the ipsilateral hemilarynx. The EBSLN then descends along the larynx crossing dorsal to the superior thyroid artery. In approximately 42 to 62% of cases, the EBSLN crosses behind the superior thyroid artery 2 cm or greater in the cranial direction from the superior pole of the thyroid gland. In 11 to 27% of patients, the distance is less than 2 cm. In 13 to 14% of cases, the EBSLN passes behind the superior lobe of the thyroid gland. In 13% of cases, the EBSLN does not cross the thyroid artery at the trunk, but runs dorsal to the artery until it has ramified.3 The variability in relationship to the thyroid gland is important for prevention of inadvertent injury during thyroidectomy.
The EBSLN lies lateral to the inferior constrictor when it reaches the CT muscle. It then divides into two main branches to supply the two bellies of the CT muscle.4 The action of the CT is to reduce the anterior angle between the cricoid and thyroid cartilages. The result of this action is to increase the distance between the anterior thyroid lamina and the arytenoids, which are anchored to the posterior cricoid. This tenses and thins the vocal cords, resulting in higher pitch.
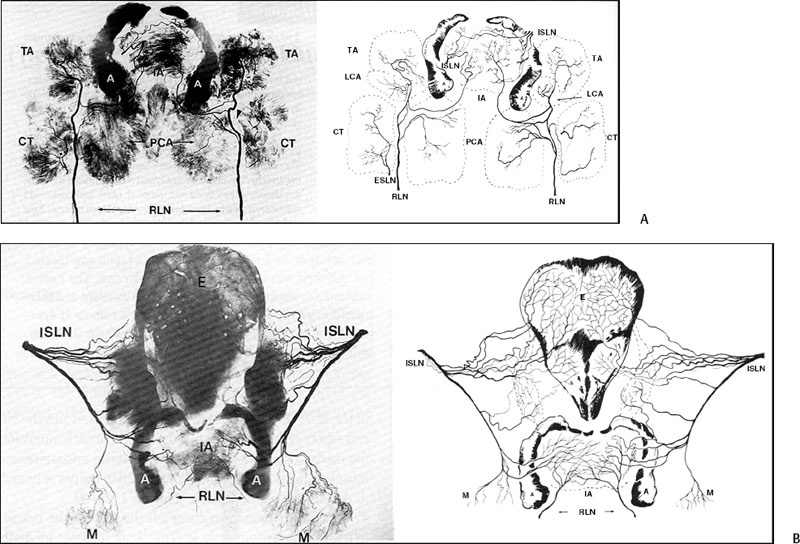
Fig.4.1 Innervation of the recurrent laryngeal nerve and superior laryngeal nerves in the intrinsic muscles of the larynx. CT, cricothyroid; IA, interarytenoid; PCA, posterior cricoarytenoid; RLN, recurrent laryngeal nerve; TA, thyroarytenoid. (From Sanders I, Wu B, Mu L, Li Y, Biller H. The innervation of the human larynx. Arch Otolaryngol Head Neck Surg 1993;119:934–939. Reprinted with permission.)
Intralaryngeal Anatomy
A modification of Sihler’s staining, a technique that stains nerves and in the process renders nonneural tissue opaque, has been used successfully to trace the small nerve branches to the individual laryngeal muscles. Sanders et al4 published a series of papers utilizing this technique, uncovering more complexity and variability of the intralaryngeal nerve distribution than previously recognized. After the RLN enters the larynx, the first branch innervates the posterior cricoarytenoid (PCA) muscle. The PCA was innervated by two branches in 50% of the specimens studied. It is estimated that the PCA may receive 25% of all motor axons carried by the RLN, underscoring its importance as the primary abductor of the glottis. The next branch to come off the RLN goes to the interarytenoid muscle. This branch passes medially around the cricoarytenoid joint and underneath the PCA. The interarytenoid receives bilateral innervation, and the right and left sides of the nerve anastomose with each other and with branches from the SLN. The terminal branches of the RLN innervate the lateral cricoarytenoid (LCA) and thyroarytenoid (TA) muscles. The LCA is innervated by a single nerve branch. The RLN terminates in the thyroarytenoid muscle, forming multiple dense anastomotic networks throughout the muscle (Fig. 4.1).
Intralaryngeal connections between the RLN and SLN have been studied. The anastomosis of Galen (a connection between the inferior division of the SLN and RLN) has been found with variable frequency and is thought to be primarily sensory.5 The existence of an anastomosis between the branches of the SLN with RLN fibers between the interarytenoid and thyroarytenoid muscles has also been described.6,7 Human anatomic studies have revealed another connection between the EBSLN and RLN in the paraglottic space that is thought to be sensory for the subglottis.8 As of yet, a motor anastomosis between the SLN and RLN has not been confirmed.
Based on Sanders et al’s examination of individual laryngeal muscles and nerve branches, they hypothesized that the laryngeal muscles may be partitioned into subcompartments that can undergo individualized activity and perform far more complex actions than previously known. Sanders et al have shown two to three compartments for the PCA, TA, and CT muscles. The CT muscle has two muscle bellies that are innervated by two branches of the external branch of the SLN. One branch enters the oblique belly, whereas the second supplies the rectus. The PCA was found to have multiple neuromuscular compartments divided by fascial planes. The human vocalis muscle appears to contain two subcompartments – a superiorly based compartment composed of multiple small fascicles, and an inferiorly based compartment made of a single large muscle fascicle.9
The composition of slow and fast twitch muscle fibers as well as the arrangement of the muscle fascicles and neural innervation suggest an ability to individually stimulate different subcompartments of the muscle.10 Within the larynx, individual muscles have different composition of fast and slow muscle fibers that display multiple innervation.11,12 In the TA muscle, type I (slow) muscle fibers had multiple innervations in 67% of fibers. In type II (fast) muscle fibers, 28% had multiple innervations. This feature may reflect the highly elastic and tremendous vocal range of the human larynx.
Nerve Physiology
The RLN and SLN carry both motor and sensory fibers. Early histologic examination of the RLN and SLN showed a mixture of myelinated and unmyelinated fibers. Myelin is the component of the nerve sheath, the Schwann cell, that provides many support functions for the nerve including increasing transmission velocity for neural signal. Motor signals are generally carried via the large and intermediate myelinated nerves, whereas sensory signals are carried by small myelinated fibers. Autonomic parasympathetic fibers are also carried by myelinated fibers. The unmyelinated fibers are thought to be branches of cervical sympathetic fibers and postganglionic parasympathetic fibers.13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







