22 Peroneal Neuropathy
Anatomy
The peroneal nerve is derived predominantly from the L4–S1 nerve roots, which travel through the lumbosacral plexus and eventually the sciatic nerve. Within the sciatic nerve, the fibers that eventually form the common peroneal nerve run separately from those that distally become the tibial nerve (Figure 22–1). In the posterior thigh, the peroneal fibers within the sciatic nerve innervate the short head of the biceps femoris, the only peroneal-derived muscle above the level of the fibular neck (Figure 22–2). More distally, the sciatic nerve bifurcates above the popliteal fossa into the common peroneal and tibial nerves. The common peroneal nerve first gives rise to the lateral cutaneous nerve of the knee, which supplies sensation to the lateral knee before winding around the fibular neck and passing through the fibular tunnel between the peroneus longus muscle and the fibula. At the fibular neck, the internal fascicular anatomy is such that the fibers destined for the deep peroneal nerve lie more medial (adjacent to the fibula) whereas the fibers destined for the superficial peroneal nerve are more lateral (Figure 22–3). The common peroneal nerve then divides into superficial and deep branches. The deep peroneal nerve (Figure 22–4) innervates the peroneus tertius and the dorsiflexors of the ankle and toes, including the tibialis anterior (TA), extensor digitorum longus, extensor hallucis longus (EHL), and extensor digitorum brevis (EDB). It continues on to supply sensation to the web space between the first and second toes. The superficial peroneal nerve (Figure 22–5) innervates the ankle everters (peroneus longus and peroneus brevis) and then supplies sensation to the mid and lower lateral calf. As it passes over the dorsum of the foot, it divides into the medial and intermediate dorsal cutaneous nerves of the foot, supplying sensation to the dorsum of the foot and to the dorsal medial three or four toes up to the level of the interphalangeal joints. In 15 to 20% of patients, an accessory peroneal nerve leaves the main superficial peroneal nerve and runs posterior to the lateral malleolus to ultimately supply the lateral EDB muscle. This is an important normal variant often encountered during routine nerve conduction studies.
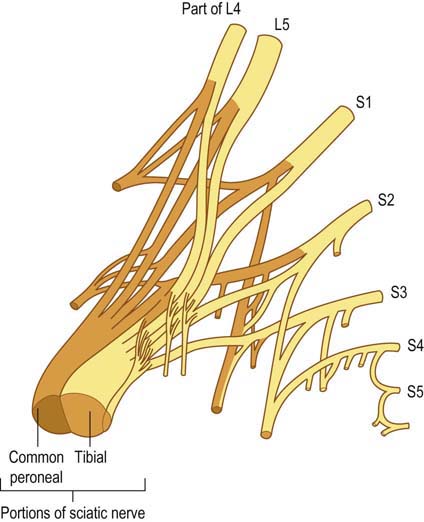
FIGURE 22–1 Common peroneal and tibial fibers within the sciatic nerve.
(Adapted with permission from Hollinshead, W.H., 1969. Anatomy for surgeons, volume 2: the back and limbs. Harper & Row, New York.)
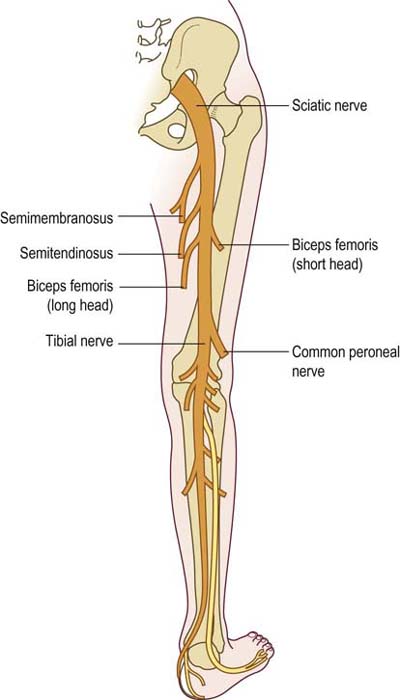
FIGURE 22–2 Sciatic-innervated muscles in the thigh.
(Adapted with permission from Haymaker, W., Woodhall, B., 1953. Peripheral nerve injuries. WB Saunders, Philadelphia.)
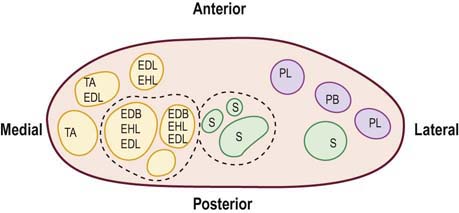
FIGURE 22–3 Internal fascicular anatomy of the common peroneal nerve at the fibular neck.
(Adapted with permission from Sunderland, S., 1973. Nerves and nerve injuries, second ed. Churchill-Livingstone, London.)
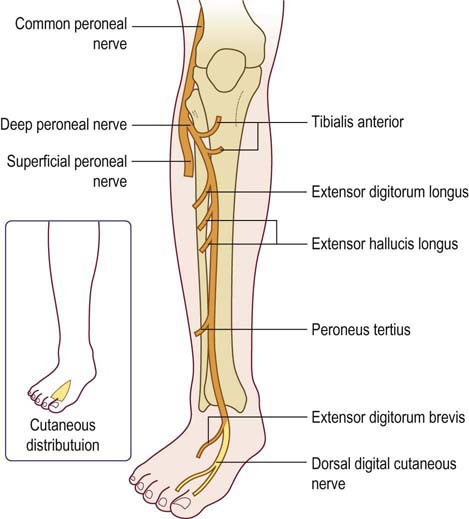
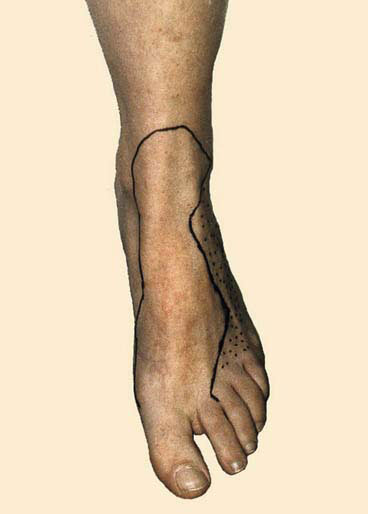
FIGURE 22–4 Deep peroneal nerve anatomy.
(Reprinted with permission from Haymaker, W., Woodhall, B., 1953. Peripheral nerve injuries. WB Saunders, Philadelphia.)
Clinical
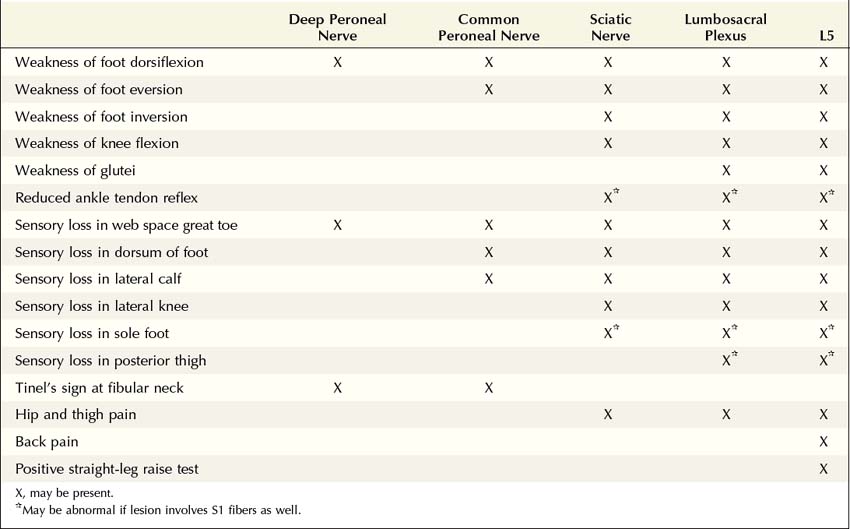
Peroneal Neuropathy at the Fibular Neck
As already noted, lesions of the sciatic nerve, lesions of the lumbosacral plexus, and L5 radiculopathy may present with a foot drop and numbness over the lateral calf and dorsum of the foot. Indeed, these lesions, especially early on, occasionally mimic a peroneal palsy almost exactly, including abnormalities of sensation (Table 22–1). It is in these cases that electrodiagnostic studies are especially helpful. On the clinical examination, any of the following abnormalities in a patient with a foot drop should suggest a lesion more proximal to the peroneal nerve at the fibular neck:
• Weakness of ankle inversion (tibialis posterior – innervated by the tibial nerve)
• Preferential weakness of the EHL (L5–S1) out of proportion to the TA (L4–L5) when the two are compared. In a peroneal neuropathy, these two muscles usually are equally affected; in an L5 radiculopathy, the EHL usually is weaker than the TA because of its predominant L5 innervation
• Sensory loss over the lateral knee (distribution of the lateral cutaneous nerve of the knee)
• Sensory loss over the sole of the foot, lateral foot, or medial calf (distribution of the plantar, sural, or saphenous nerves, respectively)
• Any weakness of hip abduction, extension, or internal rotation (gluteus medius, tensor fascia latae, gluteus maximus – innervated by the superior and inferior gluteal nerves). Because these muscles are quite strong, they must be tested at mechanical disadvantage to demonstrate subtle weakness
Etiology
Peroneal neuropathy at the fibular neck can be seen as a result of a variety of conditions (Box 22–1). Acute peroneal neuropathy often follows trauma, forcible stretch injury, or compression from prolonged immobilization. In the hospital, peroneal neuropathy at the fibular neck occurs most often postoperatively in patients who have received anesthesia or heavy sedation. Slowly progressive lesions often suggest a mass lesion, such as a ganglion or nerve sheath tumor. Entrapment of the peroneal nerve at the fibular tunnel, although quite uncommon, also may present in a progressive manner.
Box 22–1
Etiology of Peroneal Neuropathy at the Fibular Neck
Isolated neuropathy of the superficial peroneal sensory nerve is rarely reported. However, this nerve can be compressed externally, especially by tight-fitting boots. Most often, this is seen from ski boots (Figure 22–6).
Electrophysiologic Evaluation
Nerve Conduction Studies
In a patient with a foot drop and suspected peroneal neuropathy, peroneal motor, F response, and superficial peroneal sensory studies should be performed first (Box 22–2). The findings will depend on the location and severity of the lesion and on whether the underlying pathophysiology is demyelination, axonal loss, or a combination of both (Figure 22–7). In demyelinating lesions, if focal slowing or conduction block is seen across the fibular neck in the peroneal motor study, this can be used to localize the lesion. Usually, any slowing of more than 10 m/s is considered significant. Any drop in amplitude or area of more than 20%, especially over a very short segment, suggests focal conduction block (Figure 22–8). The amount of conduction block can be approximated by comparing the compound muscle action potential (CMAP) amplitude at the lateral popliteal fossa with that below the fibular head. In purely demyelinating lesions at the fibular neck, the distal superficial peroneal sensory response remains normal.
Box 22–2
Recommended Nerve Conduction Study Protocol for Peroneal Neuropathy
1. Peroneal motor study, recording extensor digitorum brevis, stimulating ankle, below fibular head and lateral popliteal fossa. If there is no focal slowing or conduction block at the fibular neck, perform a peroneal motor study, recording tibialis anterior and stimulating below the fibular head and lateral popliteal fossa.
2. Tibial motor study, recording abductor hallucis brevis, stimulating medial ankle and popliteal fossa
3. Superficial peroneal sensory study, stimulating lateral calf, recording lateral ankle
4. Sural sensory study, stimulating calf, recording posterior ankle
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree