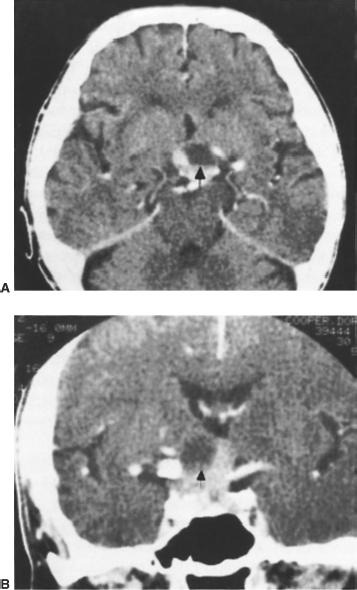
8 Pituitary Apoplexy Kalmon D. Post, John S. C. Shiau, and Jane Walsh Pituitary apoplexy is a neurosurgical emergency in which prompt intervention may halt and even reverse the neurologic deficits and life-threatening situation. The condition results from hemorrhage or necrosis of a pituitary tumor. However, Brougham et al in 19501 were the first to present a series of patients with a concomitant literature review. They described the clinical and pathologic findings of five patients who presented with changes in mental status, headaches, meningismus, and ocular disturbances. Since then, there has been extensive interest in the entity. Nevertheless, there has also been considerable debate on what the term pituitary apoplexy encompasses. In fact, there have been reports of silent pituitary apoplexy.2,3 However, defining the condition as merely a hemorrhagic or necrotic pituitary tumor is too broad. Mohr and Hardy4 estimated the incidence of asymptomatic hemorrhages in pituitary adenomas to be 9.9% as opposed to 0.6% (4 of 663) that presented with clinical findings. Other large studies cite similar numbers, with 41% to 86% of all hemorrhages remaining asymptomatic.5–8 Onesti et al9 described five patients with subclinical pituitary apoplexy, that is, a clinically silent yet extensive hemorrhage into a pituitary adenoma. Necrotic or cystic degeneration of pituitary adenomas may be asymptomatic. The diagnosis of pituitary apoplexy is made clinically by the sudden onset of headache, meningismus, visual impairment, and oculomotor abnormalities in varying combinations. Basic anatomy lends insight into the genesis of pituitary apoplexy. The pituitary gland is seated in the sella turcica of the sphenoid bone, attached to the hypothalamus by the infundibulum. The cavernous sinuses are laterally located; through these pass the internal carotid arteries (ICAs), the oculomotor (III), trochlear (IV), and abducens (VI) cranial nerves, as well as the ophthalmic divisions of the trigeminal (V) cranial nerve. Superiorly, the intercavernous and circular sinuses are enclosed in the diaphragma sellae. In the suprasellar region are the optic nerves, chiasm, and tracts. The pituitary gland receives its vascular supply from the ICAs. The inferior hypophyseal artery originates from the intracavernous carotid and supplies the posterior lobe. The superior hypophyseal artery arises just distal to the cavernous sinus to supply the stalk and adjacent parts of the anterior lobe. The majority of the anterior lobe of the pituitary derives its blood supply from the portal system. Brougham et al1 proposed that rapidly growing tumors outgrow their own blood supply, resulting in ischemic infarction. Rovit and Fein10 hypothesized that an expanding pituitary neoplasm would necessarily compress the superior hypophyseal artery against the diaphragmatic notch, rendering the pars distalis and its tumor ischemic, necrotic, and hemorrhagic. Mohanty et al11 believed that tumor size was directly related to vascularity and therefore prone to acute vascular events. Critics, however, have pointed out that even small adenomas will show evidence of hemorrhage.12,9 Furthermore, anatomic studies have shown that the predominant blood supply of pituitary tumors is derived via the meningohypophyseal trunk.13 Others suggest that “intrinsic” tumoral factors may cause the apoplectic event.6 A multifactorial explanation for pituitary apoplexy is probably more appropriate.14 Other predictive factors have been suggested. Although the majority of cases have no precipitating event, case reports of estrogen therapy, diabetic ketoacidosis, pregnancy, radiotherapy, bromocriptine, cabergoline, chlorpromazine stimulation, anticoagulation, angiography, and even cardiac surgery-induced apoplexy exist.3,4,15–31 Incidences of apoplexy following closed head trauma have also been reported.32 Explanations for these observations involve vascular compromise, attenuation, direct tumor necrosis, and systemic hypotension. However, whether there is a direct relationship between these conditions and pituitary apoplexy remains unproven and anecdotal. An overall review of the literature has shown that no particular type of tumor displays an increased incidence of hemorrhage, and the data actually reflect the relative frequency of each type of tumor.3,4,13,18,33 In 20 consecutive patients diagnosed with pituitary apoplexy, from a series of over 1000 patients treated surgically for pituitary tumors by the senior author, no contradictory trends are evident. Five patients had a history of a precipitating factor. These were bromocriptine (2 patients), radiotherapy, pregnancy, and head trauma. Hemorrhage was noted in all patients at the time of surgery and confirmed on histologic examination. In 3 cases, there was evidence of prior hemorrhage with the deposition of hemosiderin within the adenoma, and in 17 of 20 cases, necrosis was present. In 4 cases, the entire sample was necrotic, preventing identification of the cell type after immunohistochemical staining. Eleven adenomas were undifferentiated. There were 2 corticotroph cell adenomas. A Rathke’s cleft cyst with hemorrhage and inflammatory response to the ruptured cyst, and a reported case of metastatic adenocarcinoma were identified.9 As previously alluded to, not all patients who bleed into a pituitary adenoma necessarily develop the apoplectic syndrome. The authors are in agreement with several others1,9,10,13,18 who consider pituitary apoplexy a clinical entity supported with pathologic evidence of hemorrhage. Using this definition, the incidence of pituitary apoplexy ranges from 0.6% to 12.3%.6,7,13,34 The 2% incidence of pituitary apoplexy found in our patients is consistent with these studies. Semple et al had an incidence of close to 4% in a series of 62 patients with apoplexy from a group of 1605 patients.35 The distribution of sexes in pituitary apoplexy is roughly equal. The largest case series was published in 1981 by Wakai et al.34 In 51 patients with pituitary apoplexy out of 560 consecutive pituitary adenomas, 28 were males and 23 females. In Cardoso and Peterson’s 1984 review of the 241 patients reported in the literature, 141 (58%) were men.18 Males represented 60% of the authors’ personal series as well as in the Semple series.1 Cardoso and Peterson found that the average age of onset in 176 patients was 46.7 years (range, 6 to 88 years).18 The clinical progression of pituitary apoplexy can evolve rapidly in a few hours to days.1,9,18,36 Because of this variable presentation, it is prudent to include apoplexy in the differential diagnosis in any patient who presents with meningeal signs. In the authors’ series, only 4 of 20 patients were known to have pituitary adenomas. The others had their tumors diagnosed after the apoplectic event. In the Semple series, there was an average time of presentation of 14.2 days after the ictus. This delay was thought to be secondary to 81% not having a previous diagnosis of adenoma as well as the frequent misdiagnosis of subarachnoid hemorrhage.35 The presenting symptoms of pituitary apoplexy are consistent.1,3,4,6,7,9,10,13,18,33,34,38 An excruciating headache (almost ubiquitous) is characteristically retro-orbital or frontotemporal, and usually precedes other symptoms or signs. The mechanism underlying the headaches is postulated to be irritation or stretch of the basal meninges or the diaphragma sellae.3,18 Extravasation of blood into the subarachnoid space may mimic meningitis, characterized by neck stiffness, fever, and spinal pleocytosis.39,40 Mental status changes may be evident. In addition, the cerebrospinal fluid (CSF) may be frankly bloody or xanthochromic.33,41 Acute upward extension of the pituitary adenoma from a space-occupying hemorrhage, plus associated edema and necrosis, will cause compression of the optic pathways and diencephalons. Involvement of the optic pathways commonly will be manifested by deteriorating vision, ranging from mild to very severe. Visual field defects are also apparent, ranging from bitemporal hemianopsia to blindness. Optic discs usually appear normal, but optic atrophy and papilledema may be present. Often one eye is affected more than the other.41,42 Associated impaired consciousness may be related to compression of the diencephalon.18 Blood rupturing into the third ventricle has been reported in a large pituitary tumor with suprasellar extension.19 Lateral expansion of the tumor into the cavernous sinuses results in extraocular ophthalmoplegia, trigeminal dysfunction, and vascular compromise. Oculomotor (III) nerve palsy was evident in more than 50% of a series 39 and 45% of another presenting with ophthalmoplegia, diplopia, ptosis, and mydriasis.35,45 A sellar mass with extraocular ophthalmoplegia is highly suggestive of pituitary apoplexy. Abducens (VI) nerve involvement is rare, and if it occurs, usually follows the third nerve palsy.18,41 Impingement of the first division of the trigeminal (V) nerve may cause facial pain and impaired corneal reflex. Damage to the sympathetic fibers that accompany the first division may give rise to a central form of Horner’s syndrome.3 There have been reports of carotid artery occlusion resulting in mental status changes and hemiparesis or hemiplegia.44,45 Pituitary apoplexy has been considered an endocrine emergency.46 Hypopituitarism, either partial or complete, is a major manifestation.8,43,47 Low basal or stimulated levels of growth hormone, corticotrophin, thyrotropin, and gonadotropins have all been documented. Worsening of preexisting endocrine abnormalities in not unusual.3,8,47 Major morbidity and mortality can occur because of failure to treat an evolving Addisonian crisis. Conversely, spontaneous reversal of endocrine abnormalities, mostly in acromegalics, but also in prolactinomas and Cushing’s disease, have been reported following pituitary apoplexy.48 Clinically significant derangement of the neurohypophysis is rare.8 Veldhuis and Hammond calculated a 4% incidence of transient and a 2% incidence of permanent diabetes insipidus.8 Bacterial and viral meningitis, intracerebral hematoma, optic neuritis, brainstem infarction, temporal arteritis, encephalitis, transtentorial herniation, and migraine may all, in one form or another, mimic an acute pituitary vascular accident.18,33,37,39,42 However, the most important entity that must be considered and excluded is an aneurysmal subarachnoid hemorrhage, also a neurologic emergency. Both may present with an altered level of consciousness, sudden headache, ocular signs, and blood in the CSF.18,33 The mass effect of a large anterior communicating aneurysm may likewise mimic the ocular findings of a pituitary apoplectic event.49 It must also be kept in mind that intracranial aneurysms may be found in 7% of all pituitary tumors.50,51 Epidermoid cysts with extension into the sella may present like apoplexy.52 The diagnosis of pituitary apoplexy requires radiographic evidence of hemorrhage coupled with clinical correlation. Literature has demonstrated that computed tomography (CT) without contrast is most valuable the first 2 days after the hemorrhage.53,54 It will demonstrate a hyperdense lesion consistent with new blood within a pituitary tumor, which is usually hyperdense relative to brain54 (Fig. 8-1). After 48 hours, magnetic resonance imaging (MRI) is more sensitive, as it can better differentiate older blood from tumor and areas of necrosis from cystic changes17,38,54–56 (Fig. 8-2). The MRI is also helpful in estimating the age and time course of the hemorrhage. Hemorrhages of less than 7 days will appear hypointense or isointense on both T1- and T2-weighted images. A hyperintense signal will develop around the periphery of the hematoma during the second week, and increased signal intensity throughout the hematoma on T1-and T2-weighted images after 14 days.53 If clinically warranted, an angiogram or magnetic resonance angiogram (MRA) should be obtained if neither CT nor MRI is able to rule out a concomitant aneurysm. MRI will also best demonstrate the extension of the tumor or hemorrhage into the suprasellar space, as well as chiasmal compression and cavernous sinus extension. Earlier detection has also been reported with diffusion-weighted MRI.57
Etiology
Presentation
Differential and Diagnosis
Pituitary Apoplexy
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








