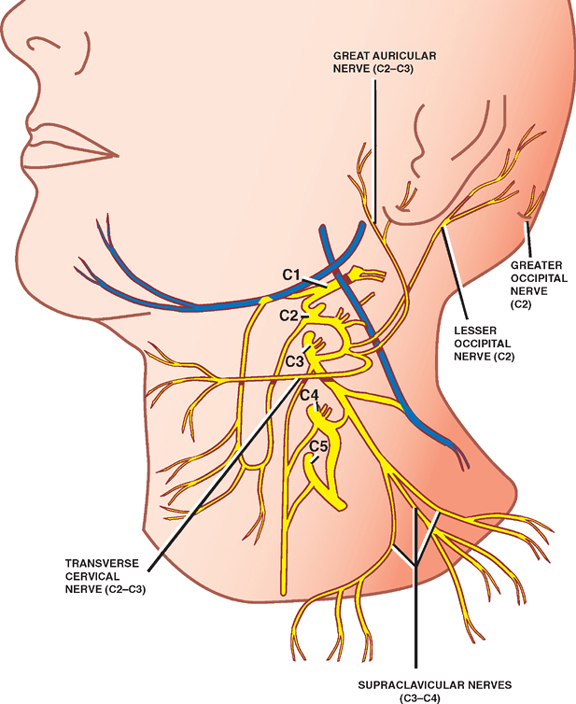
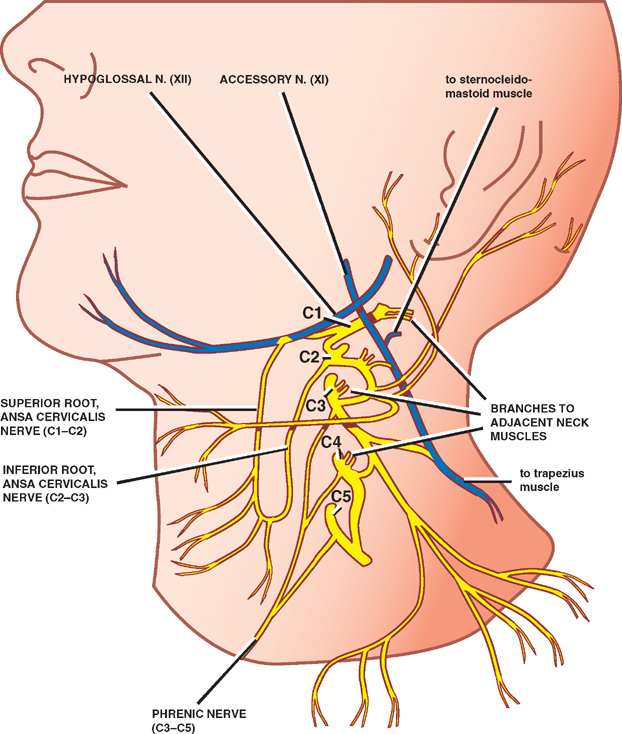
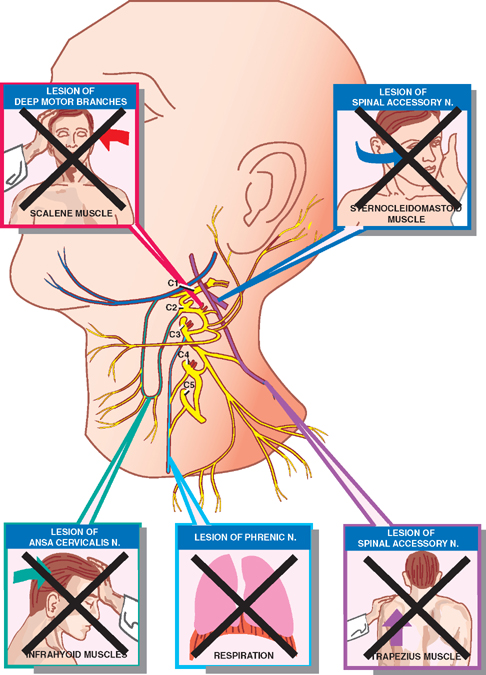
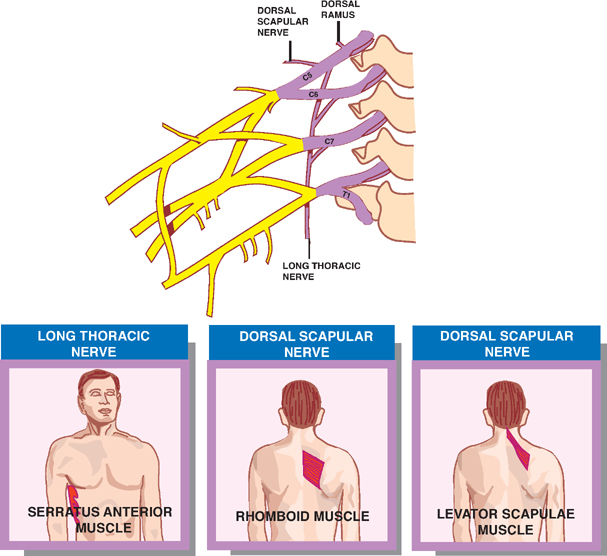
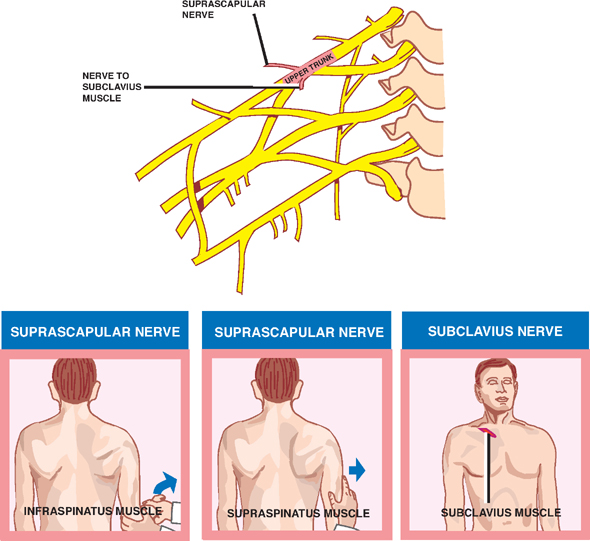
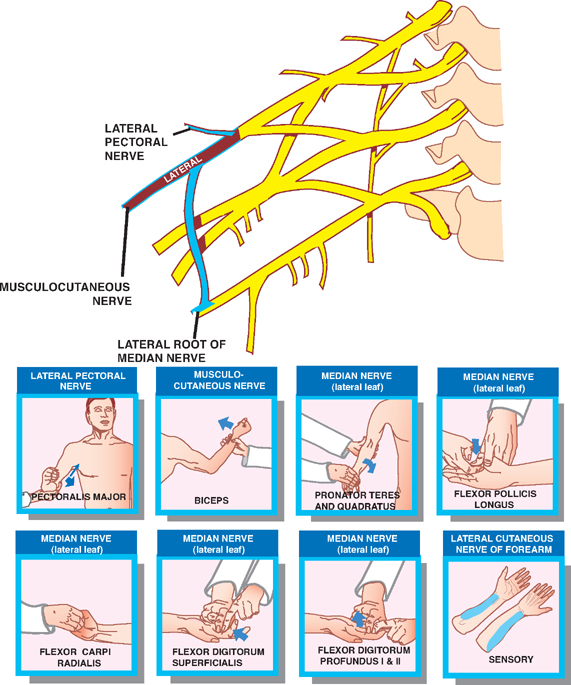
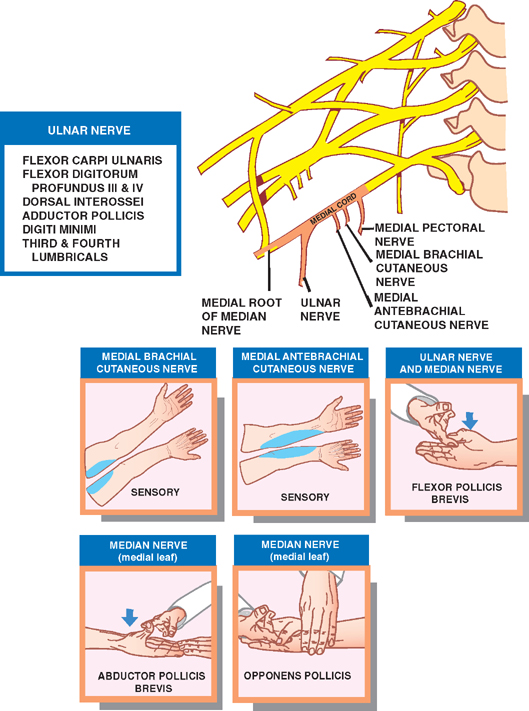
3 Plexuses The cervical plexus is composed of a collection of sensory and motor branches derived from the C1–C4 spinal nerves. It comprises a series of anastomotic loops that are located behind the sternocleidomastoid muscle, where they are closely related to the spinal accessory and hypoglossal nerves. The plexus may be divided into superficial sensory branches and deep motor branches as follows. See Fig. 3.1. The superficial sensory branches of the cervical plexus comprise the following nerves. (Note that the C1 segment, which does not possess a dorsal root, provides no sensory branches.) The greater occipital nerve is derived from the C2 spinal root. It supplies the skin of the posterior scalp. The lesser occipital nerve is derived from the C2 spinal root. It supplies the skin overlying the mastoid process, extending just above and below the mastoid process, to include part of the lateral head and part of the lateral neck. The great auricular nerve is derived from the C2–C3 spinal roots. It supplies the skin overlying the external ear, the parotid gland, and the angle of the mandible. The transverse cervical nerve is derived from the C2–C3 spinal roots. It supplies the skin overlying the anterior and lateral aspects of the neck from the body of the mandible to the sternum. The supraclavicular nerves are derived from the C3–C4 spinal roots. They supply the skin just above and below the clavicle. Fig. 3.1 Superficial sensory branches of cervical plexus. The deep motor branches of the cervical plexus comprise the following branches and nerves. See Fig. 3.2. The branches to the accessory nerve travel with the accessory nerve proper (cranial nerve XI) to supply the ster-nocleidomastoid (C2–C3) and trapezius (C3–C4) muscles. The ansa cervicalis (also known as the ansa hypoglossi) comprises a loop formed by a superior (C1–C2) and inferior root (C2–C3). The superior root fibers run for a short distance with the hypoglossal nerve. The ansa cervicalis supplies the infrahyoid muscles (flexors of the head), including the sternohyoid, omohyoid, sternothyroid, thyrothyroid, and geniohyoid muscles. Small muscular branches of the cervical plexus innervate adjacent muscles of the neck, which are flexors and rotators of the neck and head. These muscles include the lon-gus muscles anteriorly, the middle scalene more laterally, and the levator scapulae posteriorly. The phrenic nerve, which innervates the diaphragm, is derived from fibers of the C3–C5 spinal roots that join either low in the neck or in the thorax. Fig. 3.2 Deep motor branches of cervical plexus. See Fig. 3.3. Injuries of the cervical plexus produce a variety of clinical deficits, depending on the location of the lesion. Interruption of the superficial sensory branches may result in partial numbness of the head or neck. Interruption of the deep motor branches may result in weakness of forward or lateral neck flexion (infrahyoid and scalenes), rotation of the head (sternocleidomastoid), elevation of the shoulder (trapezius), or rotation of the scapula (levator scapulae). Typical causes of cervical plexus lesions include penetrating wounds, surgical injury (e.g., carotid endarterectomy), and various mass lesions. Injuries to the phrenic nerve most commonly occur distal to the cervical plexus in or around the mediastinum. Unilateral lesions result in paralysis of the diaphragm on the affected side. Frequently this is tolerated while the patient is at rest but may result in dyspnea on exertion. On the other hand, bilateral lesions are usually associated with severe ventilatory compromise at rest, unless the phrenic nerve receives an anastomotic branch from the subclavian nerve. Typical causes of phrenic nerve lesions include penetrating injury, surgical injury, and intratho-racic masses. Fig. 3.3 Lesions of cervical plexus. Functions or responses marked with an “X” are impaired or absent. See Fig. 3.4. The brachial plexus comprises an intermingling of fibers derived from the ventral rami of the C5-T1 spinal nerves. In proximal to distal order, the brachial plexus may be divided into five components: (1) roots, (2) trunks, (3) divisions, (4) cords, and (5) branches. In the posterior triangle of the neck, the C5 and C6 spinal roots join to form the upper trunk, the C7 spinal root continues as the middle trunk, and the C8 and T1 spinal roots join to form the lower trunk. The posttriangle is defined anteriorly by the sternocleiodomastoid muscle, posteriorly by the trapezius, and inferiorly by the middle third of the clavicle. More distally in the neck, in the supraclavicular fossa, each of the three trunks gives rise to an anterior and a posterior division. Behind the axillary artery, the three posterior divisions are united to form the posterior cord. The anterior divisions of the upper and middle trunk unite to form the lateral cord. And the anterior division of the lower trunk continues as the medial cord. The cords of the plexus leave the posterior triangle of the neck and enter the axilla through the outlet between the first rib and the clavicle (thoracic outlet). In the axilla, the cords give rise to the terminal branches of the plexus, the peripheral nerves. Along its ∼15 cm course, the major components of the plexus give rise to many other important branches (peripheral nerves). Fig. 3.4 Brachial plexus. See Fig. 3.5. The dorsal scapular nerve arises from C5. It supplies the levator scapulae and the rhomboid muscles. The long thoracic nerve arises from C5–C7. It supplies the serratus anterior muscle. Fig. 3.5 Branches from the roots of brachial plexus. See Fig. 3.6. The nerve to the subclavius arises from the upper trunk of the brachial plexus. It supplies the subclavius muscle. Of clinical importance, this nerve may contain accessory nerve fibers that join the phrenic nerve in the superior mediastinum. The suprascapular nerve arises from the upper trunk of the brachial plexus. It supplies the supraspinatus and in-fraspinatus muscles. Fig. 3.6 Branches from the trunks of brachial plexus. There are no branches that arise from the divisions of the brachial plexus. See Fig. 3.7. There are three branches that arise from the lateral cord, namely, the lateral pectoral nerve, the musculocutaneous nerve, and the lateral root of the median nerve. Fig. 3.7 Branches from lateral cord of brachial plexus. See Fig. 3.8. There are five branches of the medial cord, namely, the medial pectoral nerve, the medial brachial cutaneous nerve, the medial antebrachial cutaneous nerve, the ulnar nerve, and the medial root of the median nerve. Fig. 3.8 Branches from medial cord of brachial plexus. See Fig. 3.9. There are three branches of the posterior cord that are given off before its two terminal branches, namely, the upper subscapular nerve, the thoracodorsal nerve, and the lower subscapular nerve. The terminal branches of the posterior cord are the axillary nerve and the radial nerve. Fig. 3.9 Branches from posterior cord of brachial plexus. Partial lesions of the brachial plexus are far more common than complete lesions. The two most commonly described partial lesions are traumatic lesions involving the upper and lower trunks. These are known as the Erb-Duchenne type and the Dejerine-Klumpke type, respectively. Other traumatic lesions of the brachial plexus may involve the entire plexus or may be isolated to the lateral, medial, or posterior cords. Several nontraumatic lesions have also been described. These include the thoracic outlet syndrome, the apical lung tumor syndrome, radiation brachial plexopathy, and neuralgic amyotrophy. See Fig. 3.10. Lesions of the upper brachial plexus typically comprise traction injuries of the C5 and C6 nerve roots. They are frequently associated with excessive lateral displacement of the head to the opposite side or downward displacement of the ipsilateral shoulder, such as may occur during a difficult delivery or a fall or blow on the shoulder. Isolated lesions of the upper plexus primarily affect function of the shoulder and the elbow. The cardinal features of this syndrome are as follows: The posture of the extremity in upper plexus injuries is characteristic: the upper arm is internally rotated and adducted; the forearm is extended and pronated. The palm in this position faces out and backward, presenting the limb in the so-called policeman’s tip or waiter’s tip posture.
Cervical Plexus
Superficial Sensory Branches
Greater Occipital Nerve (C2)
Lesser Occipital Nerve (C2)
Great Auricular Nerve (C2–C3)
Transverse Cervical Nerve (C2–C3)
Supraclavicular Nerves (C3–C4)
Deep Motor Branches
Branches to the Accessory Nerve
Ansa Cervicalis (Ansa Hypoglossi)
Branches to Adjacent Neck Muscles
Phrenic Nerve (C3–C5)
Lesions of the Cervical Plexus
Brachial Plexus
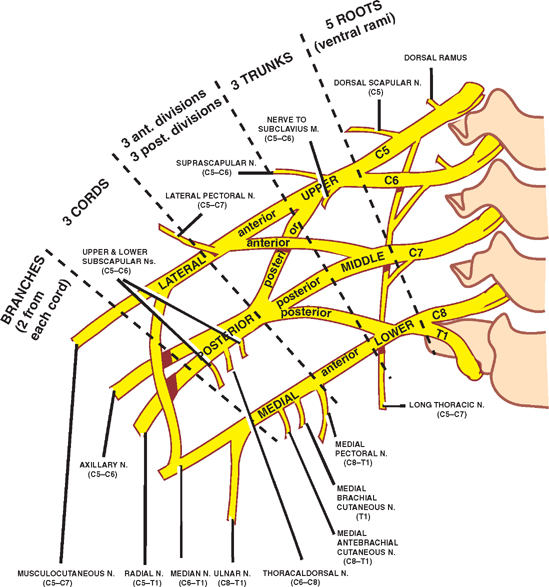
Branches from the Roots
Dorsal Scapular Nerve
Long Thoracic Nerve
Branches from the Trunks
Nerve to the Subclavius
Suprascapular Nerve
Branches from the Divisions
Branches from the Cords
Lateral Cord
Medial Cord
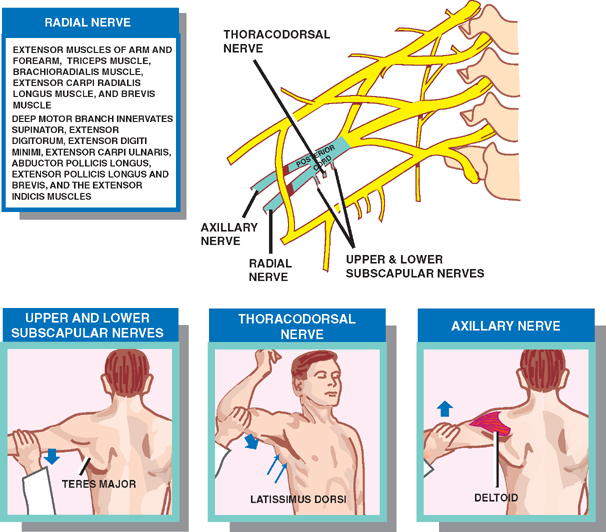
Posterior Cord
Lesions of the Brachial Plexus
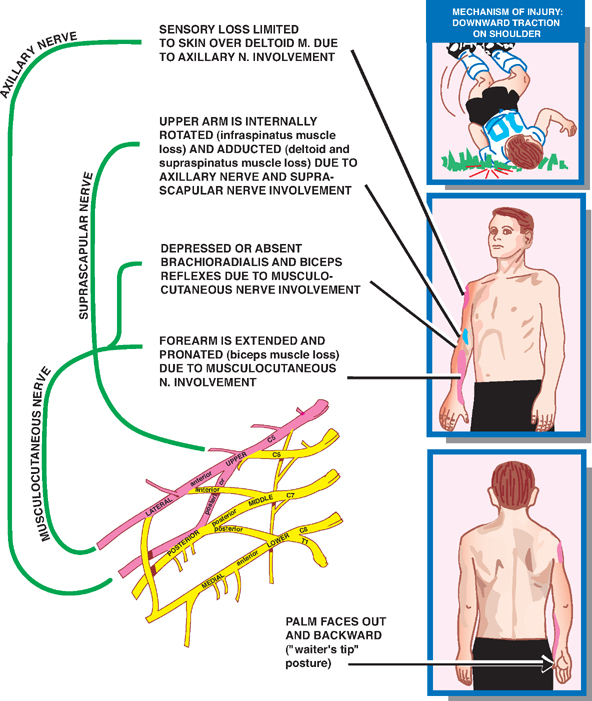
Lesions of the Upper Brachial Plexus (Erb-Duchenne Type)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








