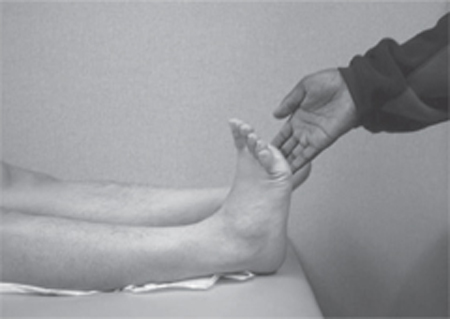
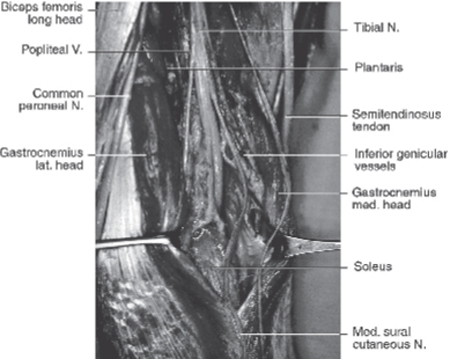
46 Posterior Tibial Nerve Injury A 28-year-old man presented to the emergency department after sustaining a gunshot wound (GSW) to his abdomen and a through-and-through GSW to his right lower extremity at the popliteal fossa. There was no noted injury to the vascular structures of his leg, but due to his abdominal injuries he was taken to the operating room where he underwent an exploratory laparotomy. The wounds to his right lower extremity were closed primarily. Postoperatively, he was discharged to an inpatient rehabilitation center after a hospital stay of approximately 2 weeks. At the time of his discharge, he complained of pain in his right foot and was experiencing plantar flexion weakness, but it was felt that this was merely a lingering effect of his injury and postoperative recovery, and that it would improve with time and physical therapy. Figure 46–1 Evaluation of tibial nerve motor function. During physical examination, the patient attempts to plantar flex the foot against the examiner’s hand, which offers resistance. In patients with proximal tibial nerve injuries that interrupt nerve conduction to the gastrocnemius and soleus muscles, plantar flexion is weakened or absent. Figure 46–2 Evaluation of tibial nerve motor function. During physical examination, the patient attempts to invert the foot against resistance. In patients with injury to the tibial nerve near or above the level of the midcalf, the posterior tibialis muscle may be affected and patients exhibit weakness or absence of foot inversion. Three months after his hospital discharge, he was still experiencing right foot weakness and pain in the bottom of his foot, and his right calf was noticeably atrophied, despite physical therapy. He was referred to a neurologist, who evaluated him and obtained electromyographic (EMG) and nerve conduction tests of his right lower extremity. Following these tests, the patient was referred to a neurosurgeon for evaluation. The patient presented to the neurosurgeon’s office approximately 5 months after his original injury. He was a healthy-appearing man with a fairly muscular build. On visual examination, there was marked atrophy of his right calf compared with his left. Motor examination demonstrated 5/5 strength in all muscle groups of his upper extremities bilaterally and of his left lower extremity. With his right lower extremity, however, the patient had 0/5 strength of plantar flexion (Fig. 46–1), and total inability (0/5) to invert the foot (Fig. 46–2), or flex or curl his toes. In addition, he demonstrated a complete lack of sensation to pinprick, light touch, pressure, and vibration on the sole of his right foot. Proprioception of the toes was intact. He was tender to palpation in his right popliteal fossa. He had 2+ reflexes of his biceps and patellar tendons bilaterally. His left Achilles tendon reflex was 2+, but absent on the right. There was no Babinski reflex and no clonus. Heel-to-shin testing was normal bilaterally, as were finger-nose-finger and rapid alternating movements, demonstrating normal cerebellar function. Examination of the patient’s gait showed that he walked with a limp on the right and was unable to walk on the toes of his right foot. He was, however, able to walk on his heels with relative ease. Review of the EMG and nerve conduction tests performed by the referring neurologist demonstrated the patient to have a severe posterior tibial nerve injury on the right. These results, taken into account along with the physical exam findings, led the neurosurgeon to diagnose the patient with a right-sided proximal tibial nerve palsy secondary to trauma (GSW). The patient was scheduled for exploration of the right tibial nerve with possible graft repair. Surgery was performed with the patient placed in a prone position and the proximal tibial nerve being accessed through a longitudinal incision in the popliteal fossa carried into the proximal calf. The patient was found to have sustained contusion injury of the tibial nerve in the popliteal fossa, with extensive surrounding scar/neuroma formation. A small branch was noted to leave the tibial nerve just proximal to the level of injury. Intraoperative nerve action potential (NAP) recordings showed no recordable action potentials across the injury site. Proximal and distal neuroma resection was performed until healthy nerve tissue was reached in the proximal and distal stumps, and fascicular graft repair was undertaken using the patient’s right sural nerve. There were no unexpected complications from the surgery itself, and the patient was discharged home on postoperative day 2. The patient was evaluated postoperatively with follow-up visits every 3 months for the first year. At the first two follow-up visits, at 3 and 6 months postop, the patient had achieved no appreciable improvement in functional status compared with his preoperative evaluation. At 9 months, however, the patient demonstrated improvement in his ability to plantar flex the foot, and associated improvement in gait. At his 1-year follow-up visit, there was a notable increase in the size of his right calf compared with its preoperative appearance, and the patient’s functional improvement continued, with 3+/5 strength to plantar flexion appreciated on physical examination and 2/5 foot inversion. He continued to have hyperesthesia on the sole of his foot, but the patient was overall very satisfied with the results of his surgery to that point. Tibial nerve injury from gunshot wound The sciatic nerve originates from the L4 through S3 spinal roots in the form of two nerve trunks: the tibial and the common peroneal nerves. These two major nerves are encompassed by a single epineurial sheath and divide in the popliteal fossa. The tibial nerve, the largest branch of the sciatic nerve, is a continuation of the medial trunk of the sciatic nerve. It begins at the bifurcation of the sciatic nerve, at the level of the middle to distal third of the thigh. After a relatively short course through the popliteal fossa, where it is close but posterior to the popliteal artery and vein, it branches a variable number of times to enter and supply the gastrocnemius, soleus, and more distal tibial-innervated muscles. It then travels distally between the bellies of the posterior tibial and soleus muscles. On reaching the gastrocnemius and soleus muscles, the tibial nerve tends to run underneath, providing a “pes-like” profusion of branches to these muscles. These branches provide input to the plantaris, popliteus, and tibialis posterior muscles, as well as to the gastrocnemius and soleus (Fig. 46–3). The tibial nerve accompanies the tibial artery and vein, running through the leg medial and posterior to the tibia and the intermuscular septum, separating anterior from posterior compartments. This nerve carries fibers destined for the foot but also produces branches in the more proximal leg to supply the flexor digitorum and flexor hallucis longus. At the junction of the upper and middle thirds of the leg, a branch to the posterior tibialis arises; slightly more distally, branches to the flexors of the big toe and other toes originate. As the tibial nerve approaches the ankle, it courses inferior to the medial malleolus and becomes superficial, lying on the medial side of the ankle and then passing into the foot beneath the tarsal tunnel. At this level, it passes beneath the medial collateral ligaments and branches into the medial and lateral plantar nerves. These nerves can also arise and be well defined before the tibial nerve reaches the malleolus. The tarsal tunnel is a fibro-osseous space located behind the medial malleolus. It has a bony floor formed by the medial talar surface, the sustentaculum tali, and the medial calcaneal wall. The flexor retinaculum, a thin, fibrous tissue originating from the medial inferior aspect of the medial malleolus and inserting into the periosteum of the medial tuberosity of the calcaneus, forms the tarsal tunnel roof. The base of the flexor retinaculum corresponds to the superior border of the abductor hallucis muscle. The posterior tibial, flexor digitorum longus, and flexor hallucis longus tendons are located within the tarsal tunnel. Each has its own synovial sheath. The tendons are contained within a separate fibro-osseous compartment formed by fibrous projections from the undersurface of the flexor retinaculum. The tibial nerve enters the tarsal tunnel between the overlying flexor retinaculum and the underlying tendon sheaths of the posterior tibial, flexor digitorum longus, and flexor hallucis longus. The tibial nerve and artery are often attached to these sheaths through surrounding areolar tissues. The tarsal tunnel is narrowest at its distal portion, where it is conjoined with the fascia of the abductor hallucis longus muscle. The tibial nerve divides into three branches at the ankle: the medial calcaneal, medial plantar, and lateral plantar nerves. The first branch, the medial calcaneal nerve, has numerous anatomical variations. The calcaneal branch leaves the tibial nerve posteriorly, supplying sensation to the heel of the foot. Just below the calcaneal branch, the main tibial nerve divides into the lateral and medial plantar nerves. Each is found within its own fibrous tunnel, separated by a partition originating from the medial calcaneus and attached to the deep fascia of the abductor hallucis muscle. The larger division, the medial plantar nerve, passes distally and laterally through the fibromuscular tunnel formed by the abductor hallucis muscle and the navicular tarsal bone. The medial plantar nerve innervates four medially located muscles: the abductor hallucis, flexor hallucis brevis, flexor digitorum brevis, and first lumbrical muscles. The distal cutaneous branches that originate from the medial plantar nerve innervate the medial two thirds of the plantar aspect of the foot. The lateral plantar nerve passes obliquely and laterally through the fibromuscular tunnel formed by the fascia of the abductor hallucis muscle inferiorly and the fascia of the flexor digitorum longus and the quadratus plantae muscles superiorly. This nerve supplies motor branches to the remaining muscles of the plantar lateral aspect of the foot and the second to fourth lumbrical muscles. The distal cutaneous branches that derive from the lateral plantar nerve innervate the lateral one third of the plantar aspect of the foot. Figure 46–3 Exploration of the left popliteal fossa/tibial nerve; anatomical relationships. The presentation of tibial nerve injury is a direct reflection of the function supplied by the tibial nerve interrupted at the level of the offending lesion. Injury to the tibial nerve just distal to its division from the common peroneal nerve in the popliteal fossa leads to dysfunction of all of the muscles supplied by this nerve, as well as decreased sensation or paresthesias over the nerve’s sensory distribution (essentially the plantar surface of the foot). Apparent motor deficits would include inability to plantar flex the foot (gastrocnemius and soleus muscles) (Figs. 46–1 and 46–4), invert the foot (tibialis posterior muscle) (Fig. 46–2), flex the toes (flexor digitorum longus and flexor hallucis longus muscles), and cup or curl the sole of the foot (small muscles of the foot supplied by the distal branches of the tibial nerve, the lateral and medial plantar nerves). Because the motor branches to the gastrocnemius and soleus muscles tend to leave the nerve fairly proximal along its course, injuries to the tibial nerve distal to the level of the knee and through the leg may manifest with varying deficits of ability to plantar flex the foot, or no apparent deficit in plantar flexion whatsoever. Injuries to the tibial nerve just proximal to the level of the midcalf may show inability to invert the foot as well as curl or flex the toes, and sensory changes on the sole of the foot with varying degrees of deficit in foot plantar flexion (at the level of the leg, deficits in plantar flexion could likely be from muscle injury rather than nerve injury). Injuries to the tibial nerve at the ankle level may manifest with relatively little motor deficit, but patients may complain of various degrees of paresthesias or sensory changes in the sole of the foot. Injuries beyond the ankle level may demonstrate no appreciable motor deficits, although patients may complain of sensory changes to areas of the sole of the foot. Due to lack of sensation to these areas, patients may develop problems with ulcers that lead to infection or other chronic injuries to the sole of the foot that go unnoticed over time.
 Case Presentation
Case Presentation

 Diagnosis
Diagnosis
 Anatomy
Anatomy
 Characteristic Clinical Presentation
Characteristic Clinical Presentation

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


