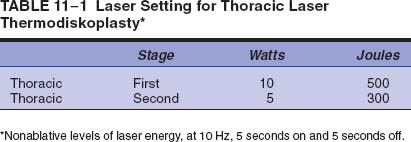
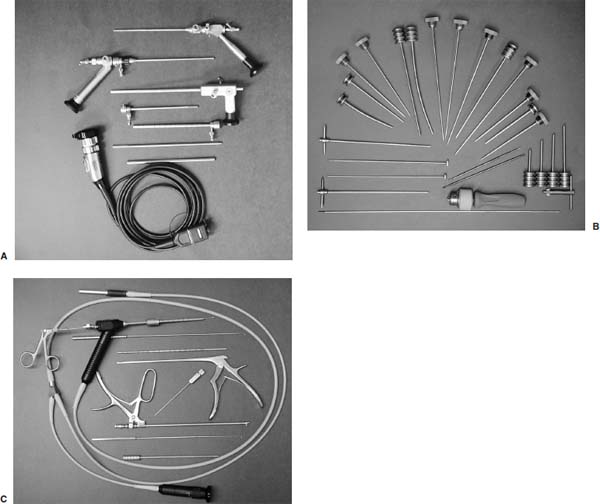
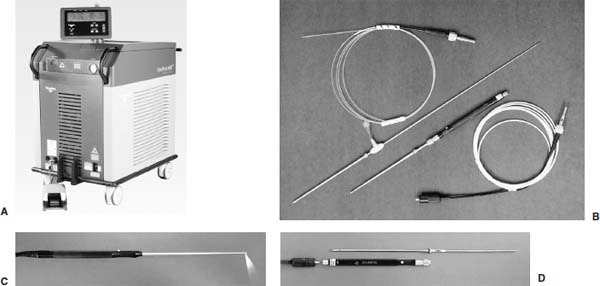
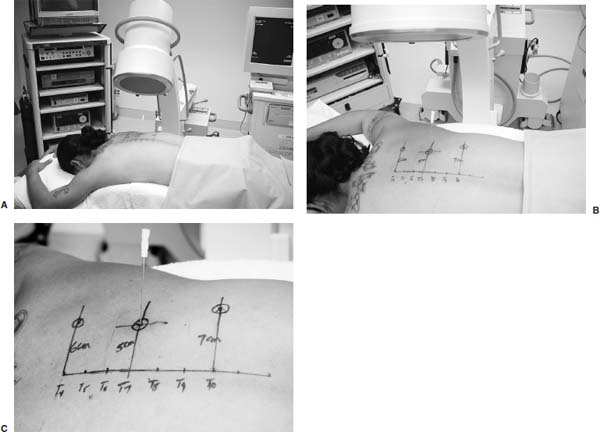
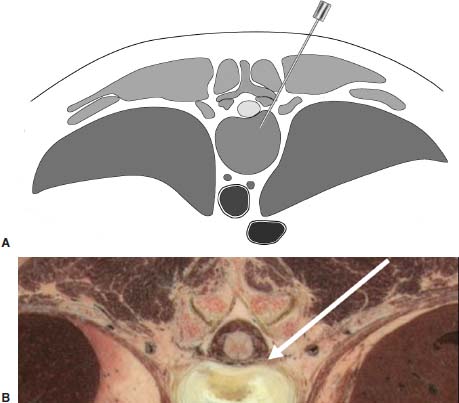
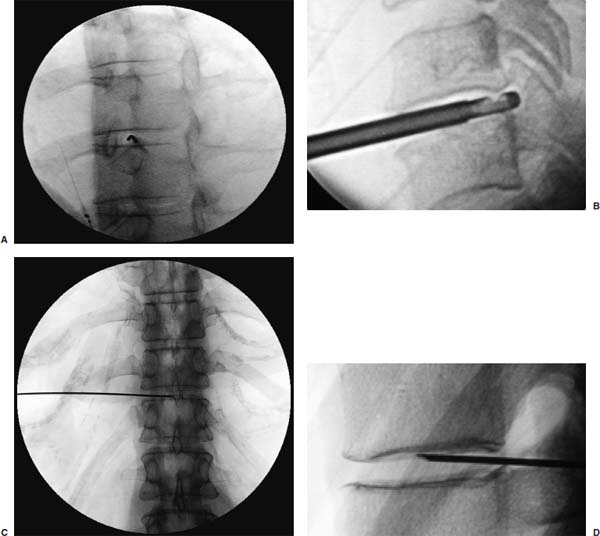
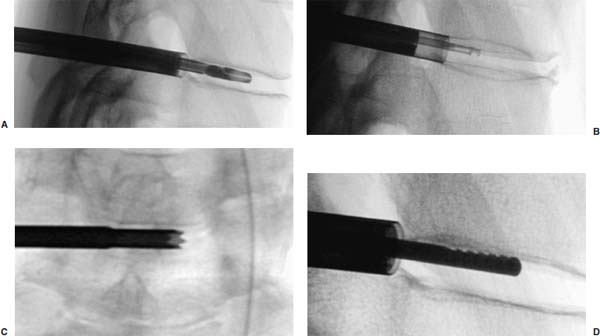
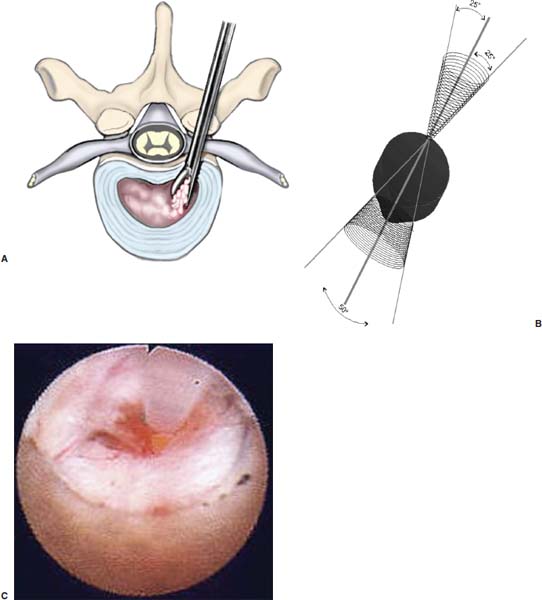
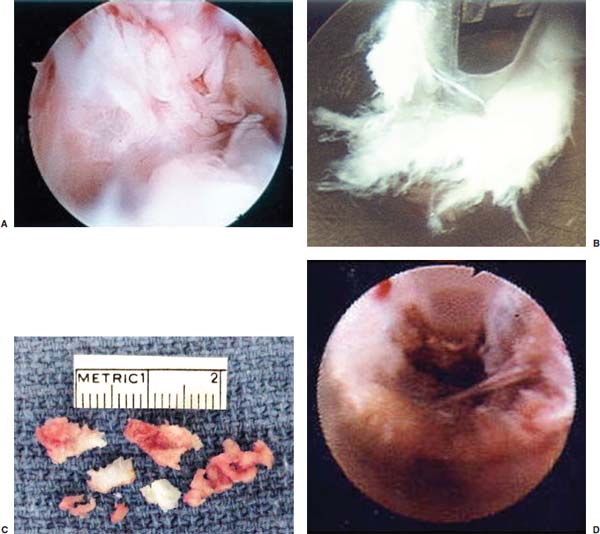
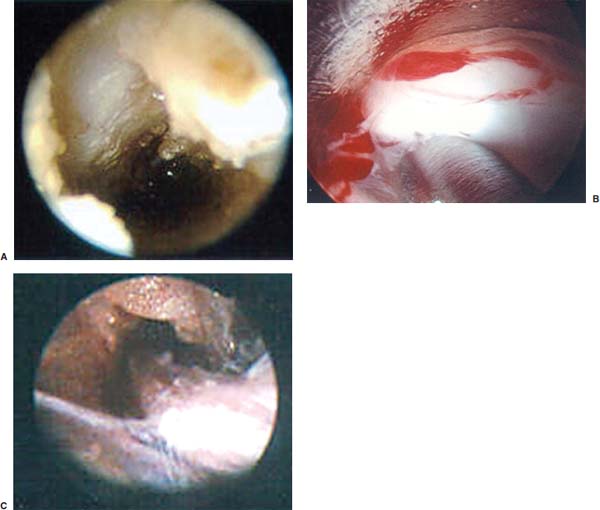
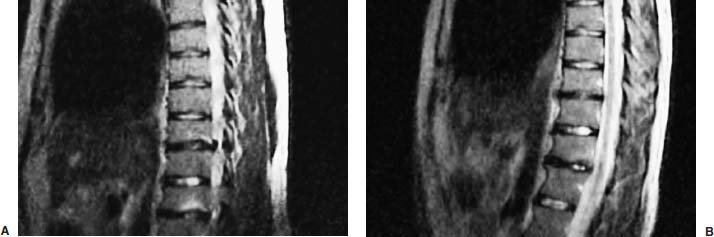
Posterolateral endoscopic thoracic diskectomy (PETD) is an alternative procedure for treating symptomatic herniated thoracic disks through an endoscope to achieve less tissue trauma than is caused by current conventional thoracic disk surgery and thoracoscopic procedures. The purpose of this chapter is to demonstrate the indications, instrumentation, surgical technique, safety, and efficacy of this less-traumatic outpatient endoscopic procedure. In addition, lower-energy nonablative laser is applied for shrinkage and tightening of the disk (laser thermodiskoplasty). This minimally invasive spinal surgery has numerous advantages, but it requires thorough knowledge of the PETD procedure, the surgical anatomy, specific surgical training, and hands-on experience in a laboratory and working closely with an experienced endoscopic surgeon through its steep surgical learning curve. The rationale and technique of this minimally invasive percutaneous endoscopic operation to relieve symptoms of protruded thoracic disks are presented. Spinal surgeons have long sought to find a procedure of choice by which to treat thoracic disk herniations.1–12 The threat of spinal cord, neural, vascular, and pulmonary injury has stimulated many attempted approaches, including posterior laminectomy (seldom performed because it is too likely to result in neurologic injury), costotransversectomy, and transthoracic, transpleural, posterolateral, transfacet pedicle-sparing, transpedicular, and, more recently, transthoracic endoscopic and posterolateral endoscopic procedures.1–6,11–13 Many clever, minimally invasive surgical endoscopic thoracic procedures have been developed, including video-assisted thoracic surgery (VATS),1 thoracic sympathectomy, and others attempting to reduce operative trauma. In the past, surgery was not contemplated unless considerable cord compression and neurologic deficit were present.5,6,11,12 A significant number of patients complain of thoracic spinal and paraspinal pain, intercostal or chest wall pain, upper abdominal pain, and occasionally low back pain due to thoracic disk protrusions without severe neurologic deficit or dramatic radiological abnormalities. With such improved diagnostic methods as MRI scans8 (the method of choice), CT myelograms, and CT scans, the diagnosis of these thoracic disk protrusions is now far more common. Such patients usually receive some period of physical therapy, injection therapy, and analgesics, and, if not cured, are expected to live with their discomfort because potential severe postoperative complications are feared if usual surgical treatment is attempted. PETD with laser thermodiskoplasty11–13 evolved from minimally invasive techniques used in the lumbar and cervical areas,10–16 and from the basic approach for performing thoracic diskography.9 We also have utilized pre- or intraoperative diskograms and pain provocation tests on almost all cases to confirm the diagnosis and the appropriate levels to treat. This chapter will describe the technique, safety, and efficacy of a method for treating thoracic disk protrusions by outpatient PETD. Indications The PETD approach is indicated12 in the following clinical situations: Contraindications The PETD approach is contraindicated in the following clinical situations: Instruments and Preparation This surgical equipment and these instruments11–13 are necessary to perform PETD (similar to anterior endoscopic cervical microdiskectomy): FIGURE 11–1 Posterolateral endoscopic thoracic diskectomy instruments. (A) Thoracic endoscopes (0-, 6-, and 30-degree) and trichip digital camera. (B) Endoscopic working cannula systems, trephines, rasp, and burrs. (C) Various types of forceps and rongeurs. FIGURE 11–2 Holmium:YAG laser equipment for laser thermodiskoplasty. (A) An 85 W double-pulse holmium:YAG laser generator. (B) A 550 µm holmium bare fiber with flat tip, and right-angle (side-firing) probe. (C) Single-use side-firing probes. (D) Reusable short side-firing probes. Anesthesia The patient is treated in an operating room under local anesthesia and monitored for conscious sedation. The anesthesiologist maintains mild sedation, but the patient is able to respond. Two grams of Ancef and 8.0 mg of dexamethasone are given intravenously at the start of anesthesia. Surface EEG (SNAP; Nicolet Biomedical, Madison, WI, USA) provides added precision of anesthesia. Patient Positioning The patient is prone on the table with a radiolucent 20-degree angled sponge under the symptomatic side of the chest, angling it into an obliquely up position (Fig. 11–3A). The arms are supported on arm boards over the head. Because only local anesthesia and mild sedation are used, the extremities, buttocks, and shoulders are restrained from sudden motion with adhesive tape. Localization Levels are identified by counting under C-arm fluoroscopy from the twelfth rib up, and from C7 of the cervical spine down for upper level thoracic diskectomies. Radiopaque markers are placed on the skin at appropriate sites.11–13 The midline, the levels, and the point of entry (operating portal) for surgery are marked on the skin with a marking pen (Fig. 11–3B). Using sterile technique, the level of the disk can be accurately identified by inserting an 18-gauge needle into a disk (Figs. 11–3C, 11–4, 11–5). The portal of entry is to be marked at 4 to 5 cm away from the midline at the midthoracic area (T5–T8 inclusive) at the respective thoracic disk level, 6 to 7 cm from the midline at the lower thoracic area (T9–T12 inclusive), and at the upper thoracic area (T1–T4 inclusive). Positioning of the instruments is checked throughout the procedure by C-arm fluoroscopy in two planes as needed. After the involved levels are identified, sterile needle electrodes are placed in the intercostal muscles innervated from those levels for continuous neurophysiological EMG monitoring,22 with a ground electrode having been previously placed. FIGURE 11–3 Patient positioning and localization. (A) Patient positioning. (B) Localization—skin marking. (C) Placement of needle (portal). FIGURE 11–5 Fluorosopic views for placement of needle/ stylette. (A,B) Needle placement into “safety zone” at the neural foramen between the interpedicular line and the rib head. (C,D) Incremental advance of stylette placement into center of the disk. Surgical Technique Under local anesthesia a beveled 20-gauge, 3.5-inch spinal needle is inserted into the portal of entry, as described under localization and fluoroscopic guidance (Fig. 11–5). The needle is incrementally advanced under C-arm fluoroscopic guidance at a 35- to 45-degree angle from the sagittal plane, targeting toward the center of the disk, into the “safety zone,” between the interpedicular line medially and the rib head at the costovertebral articulation laterally,11,12 and medial to the costotransverse junction (Fig. 11–5). During the needle insertion, one must keep the needle tip immediately along the medial aspect of the rib head to avoid entering the spinal canal medially, and medial to the costovertebral junction to avoid pleural puncture. After the anulus is punctured, the needle is incrementally advanced to the center of the disk. The stylette of the spinal needle is removed. Isovue contrast (Bracco Diagnostics, Inc., Princeton, NJ) is injected, observing the ease and volume of injection, the fluoroscopic appearance in AP and lateral projections, and the patient’s description of the location, concordance, and intensity of any pain produced. Surgery is performed if the diskogram and pain provocation tests are confirmatory. FIGURE 11–6 Fluoroscopic view of posterolateral endoscopic thoracic diskectomy (PETD) instruments. (A) Micrograsper forceps. (B) Trephine. (C) Side fire laser probe. (D) Endoscopic rasp. A narrow 12-inch plain wire guide is passed into the center of the disk through the spinal needle placed for the diskogram. The needle is then removed. A 3 to 4 mm skin incision is made at the site. The diskectomy cannula containing its dilator is passed over the guidewire and is advanced to the anulus. A trephine replaces the dilator and incises the anulus. The cannula then advances a short distance into the disk space. The disk is decompressed using curettes, trephine, microforceps, diskectome, and the laser (Figs. 11–6, 11–7, 11–8, 11–9). Disk removal is aided by a rocking excursion of the cannula in a 25-degree arc, a “fan sweep” motion from side to side, that creates an oval cone-shaped area of removed disk totaling up to 50 degrees (Fig. 11–7). During the procedure the endoscope is utilized for visualization, and under magnification additional disk material and osteophytes are removed with microcurettes, rasps, forceps, and diskectomes (Figs. 11–8, 11–9). Large spurs or a rib head obstructing entry to the disk space can be removed or can be perforated by a set of more aggressive-toothed trephines (Fig. 11–6). A holmium:YAG laser (Fig. 11–2) is used to ablate additional disk (500 J at 10 W, 10 Hz, 5 sec on and 5 sec off), then at a lower power setting (300 J at 5 W) (Table. 11–1) to shrink and contract the disk, further reducing the profile of the protrusion and hardening the disk tissue, laser thermodiskoplasty9 (Fig. 11–7). This may also cause sinovertebral neurolysis or denervation. The diskectome is again used briefly to remove charred debris. The disk space can be directly visualized by endoscopy for confirmation of disk decompression (Fig. 11–9). The probe and cannula are removed. Marcaine (0.25%) is infiltrated subcutaneously about the wound. A Band-aid is applied over the tiny wound. Postoperative Care The patient is checked neurologically prior to leaving the operating room. An upright portable chest x-ray done in the recovery room rules out a pneumothorax. Ambulation begins immediately after recovery, and the patient is usually discharged 1 hour after surgery. The patient may shower the following day. An ice pack is helpful. Mild analgesics and muscle relaxants are required at times. A progressive exercise program begins the second postoperative day. Patients are usually allowed to return to work in 1 to 2 weeks, as long as heavy labor and prolonged sitting are not involved. Most patients found this procedure extremely gratifying. FIGURE 11–7 Surgical technique of thoracic diskectomy “fan sweep” maneuver and endoscopic view of laser thermodiskoplasty. (A) Thoracic diskectomy. (B) “Fan sweep” maneuver. (C) Holmium bare laser flat-tip fiber in action. Outcome Ninety-six percent of 150 consecutive patients with a total of 197 herniated thoracic disks demonstrated good to excellent relief of symptoms. Six patients (4%) had persistent thoracic pain, although overall their pain improved. The patients postoperatively resumed usual activity in a few days, and full active lives in 3 to 7 weeks.13 Discussion PETD is a minimally invasive surgical procedure for treating symptomatic herniated thoracic disks through an operating endoscope with much less tissue trauma and zero mortality. It has numerous advantages, but it requires thorough knowledge of the surgical anatomy, the PETD procedure, specific surgical training, and hands-on experience in a laboratory and working closely with an experienced endoscopic surgeon through its steep surgical learning curve in order for a surgeon to become competent and avoid possible complications. FIGURE 11–8 Endoscopic view of thoracic diskectomy. (A) Intradiscal endoscopic view. (B) Endoscopic disk removal with cutter forceps. (C) Disk fragments removed. (D) Laser application for disk decompression. Complications and Avoidance A thorough knowledge of the procedure and surgical anatomy of the thorax and thoracic spine, careful selection of patients, and preoperative surgical planning with appropriate diagnostic evaluations facilitate the PETD and prevent potential complications.2,3,11,13 All potential complications of open approaches for thoracic disk surgery are possible but are rare or much less frequent3,7,10,11,21,23 in PETD, with no rib resection or deliberate collapse of the lung required. FIGURE 11–9 Endoscopic view after PETD. (A) After PETD, hollow disk defect and end plates are seen. (B) Grasper forcep for disk removal below the intercostal nerve. (C) Intercostal nerve after microdiskectomy. Advantages The advantages7,10–12,14,21 of PETD are numerous. They include: Disadvantages This technique is useful in select patients and is not appropriate for patients with severe thoracic disk extrusions causing cord compression with severe neurologic deficit (parparesis) and patients with severe congenital or acquired stenosis of the spinal canal. In patients with severe spondylosis and foraminal stenosis, this technique may not be suitable because insertion of the endoscope may not be feasible. FIGURE 11–10 Large herniated T10 and T12 disks, pre- and postoperative MRI scans. Case Illustration A 24-year-old man had complained for 2 months of intractable midback pain and muscle spasm. Past history was noncontributory. Parathoracic muscle spasm was palpable adjacent to the painful level. Neurologic examination showed hypalgesia in T10 and T12 dermatomes. MRI demonstrated two protruded thoracic disks (at T10 and T12 levels). Physical therapy, analgesics, and epidural steroid injections did not alleviate his discomfort. Chest x-ray demonstrated 13 thoracic vertebrae with 13 ribs, with seven cervical and five lumbar vertebrae. The patient was treated by PETD at T10–T11 and T12–L1. He had total relief of his symptoms postoperatively. Comparative preoperative and postoperative MRI scans showed the disappearance of the protruded disks (Fig. 11–10). Posterior endoscopic thoracic diskectomy performed for symptomatic herniated thoracic disk with added laser “tightening” of the disk (thermodiskoplasty) is an easier, safe, and efficacious procedure. This minimally invasive, less-traumatic outpatient procedure results in less morbidity, more rapid recovery, and significant economic savings. The mortality rate was zero in a multicenter study23 of percutaneous endoscopic spinal diskectomy (26,860 cases), and the morbidity rate was less than 1%, with patient satisfaction of more than 92% for thoracic disks. There are no reported spinal cord injuries, intercostal neuralgia, or dural tears, and no significant infection, vascular injury, or pulmonary complications. PETD requires a knowledgeable and competent surgeon with a thorough appreciation of the surgical anatomy of the thorax and thoracic spine intercostal nerves and vessels, the relationship of the rib heads, pedicles, disk spaces, and spinal cord. To perform the procedure, the spine surgeon must have specific surgical training with hands-on experience in the laboratory, and, most importantly, must spend time working through the steep surgical learning curve with an endoscopic spinal surgeon expert at this procedure. REFERENCES 8. Simpson J. Thoracic disc herniation. Spine. 1993;18:872–877. 17. Boriani S, Biagini R, Delure F. Two level thoracic disc herniations. Spine. 1994;21:2461–2466.
11

Posterolateral Endoscopic Thoracic Diskectomy

< div class='tao-gold-member'>
Posterolateral Endoscopic Thoracic Diskectomy
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree