CHAPTER 24 Principles of Neurocritical Care
Medical care of a patient with an acutely deteriorating neurological or neurosurgical disorder is vastly different from that for patients with other medical or surgical disorders. Management is distinguished by recognition of the potential for further harmful injury to the central nervous system (CNS), identification of the causes of neurological deterioration, and recognition of the urgent need for neurosurgical procedures. Admission to a dedicated neurosciences intensive care unit (NICU) is preferred for any patient with severe traumatic head injury, aneurysmal subarachnoid hemorrhage, large ischemic stroke, expanding intracerebral hematoma, and CNS infections. Any “unstable” patient with an acute neurological or neurosurgical disorder, however, is better served in an NICU and, depending on the underlying cause, may require specific interventions. This chapter discusses the general principles of the initial assessment and care of critically ill neurological and neurosurgical patients. More detailed information on the complex care of these patients can be found in two monographs.1,2
Assessment of Impaired Consciousness
Neurologists and neurosurgeons have a singular aptitude for the assessment and correct interpretation of impaired consciousness. Because consciousness is often decreased in patients with acute CNS lesions,1 a brief review of the processes underlying abnormal consciousness is warranted. One of the critical anatomic elements that maintain or, more strictly speaking, activate consciousness has been defined under the term ascending reticular activating system. This neuronal system, located in the caudal brainstem, connects to the thalamus. These synapsing fibers extend from the entry of the trigeminal nerve in the midpons to the thalamus, which in turn loops fibers to the cortex and back, thereby creating a thalamic-cortical circuitry. Coma can be expected when destructive or compressive lesions interrupt these synapsing fibers. Therefore, a structural lesion in the pons or mesencephalon can interrupt cortical stimulation and generate an altered state of consciousness. Common lesions are occlusion of the basilar artery, which causes ischemia of major portions of the brainstem; pontine hemorrhage involving the tegmentum; and compression of the brainstem from acute, mostly hemorrhagic cerebellar lesions.
Thus, disturbances in arousal lead to diminished alertness. Altered arousal involves an altered state of awareness, and these two components are interrelated but sometimes dissociated. One can be awake and aware (normal vigilance), awake but not aware (persistent vegetative state), and not awake and not aware (coma or brain death).1
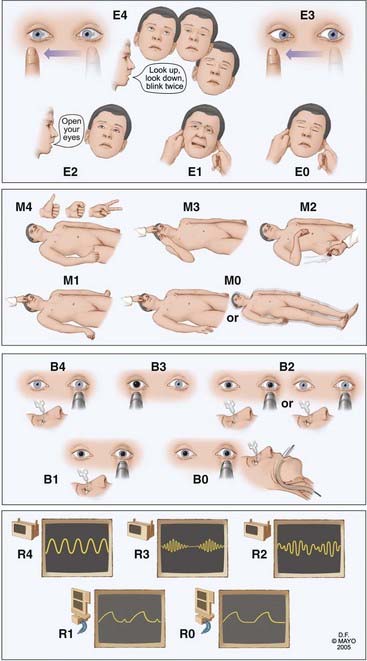
Neurological examination starts with assessment of responsiveness of the patient, and the simple reaction to painful stimuli is often one of the most important tests. Absent eye opening, vertical eye movements, or blinking (locked-in syndrome) and absent motor response to a voice command lead to the application of noxious stimuli. These stimuli should be limited to three known and reliable stimuli (compression of the supraorbital nerve, nail bed, and temporomandibular joints). The response of the patient to these stimuli is the first step in determining the depth of coma (Fig. 24-1).
We have developed and validated a new coma scale, the FOUR score, and tested it for accuracy when used by neurologists, emergency physicians, and medical intensivists.3–5 We compared ratings by residents and nursing staff specialists from all intensive care units (ICUs) and found a high degree of agreement. In this scale (Fig. 24-2) there is no assessment of verbal response, which at least in the GCS, is more a measure of orientation than alertness. The FOUR score is more useful in intubated, critically ill patients. This scale identifies different levels of coma but also locked-in syndrome, uncal herniation, and brain death. The FOUR score can be summed, and the summed scores reasonably correlate with certain degrees of impaired consciousness (alert, 16; drowsy, 12; stupor, 8; coma, 4; brain death, 0). However, it is better to describe the separate components when communicating (e.g., “this patient with traumatic brain injury has his eyes open but does not track a finger, has intact pupil and corneal reflexes, localizes to pain, is intubated, and triggers the ventilator”).
The FOUR score has been received well and is currently used or being piloted in ICUs. After initial assessment of the depth of coma, a more detailed examination follows, including a comprehensive assessment of brainstem reflexes, eye movements in particular. The eyes should be evaluated for spontaneous movement, position of the eyes with eyelid opening, and movement after turning the head or irrigation of the ear with cold water. Abnormal motor movements, pathologic reflexes, and tone are noted. With these neurological findings it should be possible to localize the lesion to three main parts of the brain—both hemispheres (or thalamus), the brainstem, or the cerebellum; key findings are shown in Table 24-1. These findings are then combined with findings on computed tomography (CT) and lead to a tailored differential diagnosis. Causes of impaired consciousness in patients in the NICU are mostly structural, secondary to postictal stupor, or, less commonly, due to acute metabolic derangements or the use of toxic substances, drugs, alcohol, or sedatives.
TABLE 24-1 Main Areas of Lesion Localization in Coma with Common Clinical Pointers
| LOCATION | CLINICAL POINTERS |
|---|---|
| Bihemispheric | |
| Intrinsic brainstem | |
| Brainstem displacement (from a hemispheric or cerebellar mass) |
Assessment of the Airway and Need for Mechanical Ventilation
Depression of the level of consciousness is not an absolute indication for mechanical ventilation. Intubated patients with acute CNS disease are generally able to maintain efficient gas exchange. However, patients with abnormal breathing patterns that result in inadequate oxygen delivery and hypercapnia need to be mechanically ventilated. Noninvasive mechanical ventilation (BiPAP) is a reasonable option in many postoperative patients with marginal oxygenation.6 In any patient on mechanical ventilation, a “ventilator bundle” is ordered (head elevation 30 degrees; peptic ulcer and venous thromboembolism prophylaxis).7 Intubation after a seizure is not usually necessary if the airway is not obstructed.
Assessment of Volume Status and Blood Pressure
Monitoring of volume status should include laboratory values (Table 24-2), with serial body weight and fluid balance being the most practical indicators. Patient with adequate fluid balance should have a hematocrit of less than 55%, an osmolality of less than 350 mOsm, and a serum sodium concentration of less than 150 mEq/L. Any higher values should signal dehydration.
TABLE 24-2 Indicators of Volume Status in Patients with Acute Neurologic Illness
| Basic principles | |
| Monitor |
From Wijdicks EFM. The Practice of Emergency and Critical Care Neurology. New York: Oxford University Press; 2010.
Hypertension has been arbitrarily defined as systolic blood pressure of 180 mm Hg or greater and mean arterial blood pressure of 120 mm Hg or greater. There are very few data on the need for blood pressure control and the best pharmaceutical agents in patients with acute neurological illness. In most patients in the NICU, acute hypertension is treated with a labetalol bolus of 20 to 40 mg and hydralazine, 20 mg (when patients have significant bradycardia). Recalcitrant hypertension may be treated with nicardipine by titrating up from a starting dose of 5 mg/hr while closely monitoring for hours via an arterial line. Recently, a study in China suggested that aggressive lowering of blood pressure with urapidil and furosemide to a systolic pressure of 140 mm Hg is safe and may possibly reduce expansion of intracerebral hemorrhage.8 It remains very uncertain whether outcome is affected by this measure, however.
How to best manage blood pressure in patients with aneurysmal subarachnoid hemorrhage is not known. Most neurosurgeons feel comfortable only if systolic blood pressure is maintained at less than 180 mm Hg, particularly in patients with an unsecured aneurysm. The relationship between blood pressure and rebleeding has not been established. A recent study suggested that systolic blood pressure above 160 mm Hg is associated with an increased risk for rebleeding, but many of these studies have poorly defined rebleeding.9
Postoperative hypertension is best managed by treatment of pain (mostly fentanyl), hypoxemia, and volume overload, if present.10
Assessment of Infection Potential
Fever is a key clinical sign that mostly signals infection. Fever is also associated with poor outcome after ischemic stroke,11 intracerebral hemorrhage,12 and aneurysmal subarachnoid hemorrhage,13 but the pathophysiologic effects of increased brain temperature on neuronal function are not well understood.
Fever develops in 25% to 50% of NICU patients. Fifty-two percent of fevers were explained by an infectious etiology, with pulmonary pathology being most predominant.14 Infectious causes should be aggressively sought (chest radiograph; blood, urine, and sputum cultures), but noninfectious causes of fever may occur and include reaction to blood products, deep venous thrombosis (DVT), drug fever, postsurgical local tissue injury, pulmonary embolism (PE), and central fever with its extreme autonomic storms (episodes of profuse sweating, tachycardia, tachypnea, and bronchial hypersecretion). Subarachnoid hemorrhage, intraventricular hemorrhage, and posterior fossa surgery can lead to a sterile inflammatory meningitis characterized by a progressive increase in cerebrospinal fluid (CSF) white blood cell counts and hypoglycorrhachia. Penicillins and phenytoin are the most common causes of drug-induced fever.15 DVT occurs in 9% of NICU patients and should be monitored with lower extremity ultrasonography.
The systemic inflammatory response syndrome may be diagnosed when fever is associated with tachypnea, tachycardia, or leukocytosis in the absence of detectable infection.16
Pneumonia is the most common nosocomial infection in critically ill neurological patients, and approximately half of all nosocomial infections are associated with mechanical ventilation. The rate of pneumonia increases 5- to 20-fold in intubated patients and with the duration of mechanical ventilation.17 Empirical antibiotic therapy is typically used at the first signs of infection. In general, early infections (<3 days) require coverage for Staphylococcus aureus, Haemophilus influenzae, Streptococcus pneumoniae, and nonpseudomonal gram-negative rods. Patients with late infections require double coverage for resistant Pseudomonas or Acinetobacter and treatment with vancomycin for methicillin-resistant S. aureus. Treatment should be modified after culture and sensitivity results are available. The duration of treatment with an effective agent should range from 7 to 14 days.
Urinary tract infections commonly develop after chronic indwelling bladder catheterization. After 10 days, nearly 50% of all catheterized patients have significant bacteriuria.18 Because asymptomatic bacterial colonization is extremely common, treatment should be reserved for patients with pyuria (>10 cells/mm3) and fever and leukocytosis. Early uncomplicated urinary tract infection can be treated with sulfamethoxazole/trimethoprim or fluoroquinolone for 7 days. Treatment should be guided by the results of culture and sensitivity testing. Changing the catheter before treatment of infection may reduce the rate of secondary infection.19
Ventriculostomy-related infection is rare, with the incidence of ventriculostomy-related meningitis or ventriculitis being approximately 8%.20 A combination of ceftazidime and vancomycin is the preferred regimen for empirical coverage. The infected catheter should be removed and treatment given for a minimum of 14 days.
Initial management of fever includes the administration of acetaminophen, but even high doses may not be effective. Currently, fever is aggressively treated with water-circulating cooling pads, and a feedback mechanism in the device secures a constant core temperature. A clinical trial comparing a simple cooling blanket with administration of acetaminophen for controlling fever found a 30% failure rate with both modes of treatment.21 The use of cooling pads with constant temperature control was shown to be superior to simple cooling blankets for the management of fever.22
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree