31 Proximal Neuropathies of the Shoulder and Arm
Suprascapular Neuropathy
Anatomy
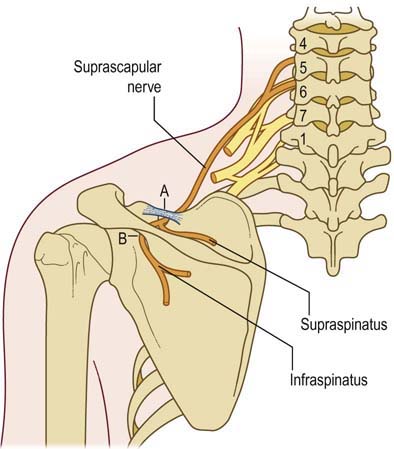
The suprascapular nerve comes off the upper trunk of the brachial plexus, receiving innervation from both the C5 and C6 roots. The nerve runs posteriorly under the trapezius, passing through the suprascapular notch of the scapula to enter the supraspinous fossa (Figure 31–1). The suprascapular notch is U shaped, located along the superior border of the scapula, and covered by the transverse scapular ligament. The suprascapular nerve first supplies motor fibers to the supraspinatus muscle, a shoulder abductor, before proceeding laterally to supply deep sensory fibers to the glenoacromial and acromioclavicular joints, and the coracoacromial ligament. It then wraps around the spinoglenoid notch of the scapular spine under the spinoglenoid ligament to enter the infraspinous fossa, where it supplies motor fibers to the infraspinatus muscle, an external rotator of the shoulder. The suprascapular nerve usually carries no cutaneous sensory fibers, although rare anomalous innervations have been reported. In these rare cases, the suprascapular nerve carries cutaneous sensation to the proximal lateral arm, the area usually supplied by the axillary nerve.
Clinical
Suprascapular entrapment most commonly occurs at the suprascapular notch, under the transverse scapular ligament. Less frequently, the nerve can also be entrapped distally at the spinoglenoid notch. The suprascapular nerve is relatively immobile both at its origin at the upper trunk and at the suprascapular notch. Because both the shoulder and scapula are quite mobile, movement, especially repetitive movement, results in stretch and nerve injury (Figure 31–2). Also, like most of the major proximal upper extremity nerves, the suprascapular nerve is often prominently involved in neuralgic amyotrophy (see Chapter 30).
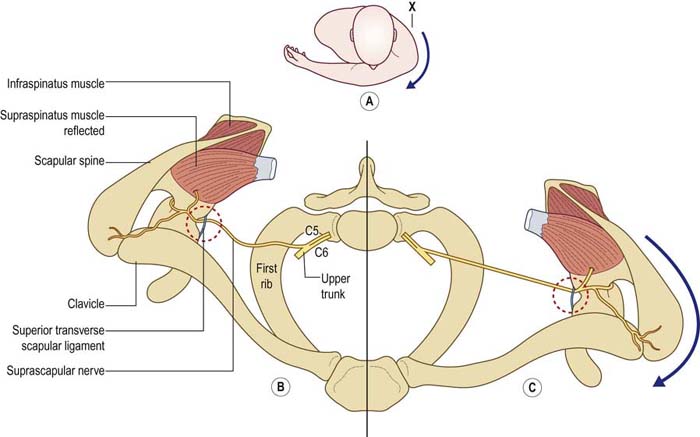
FIGURE 31–2 Suprascapular neuropathy.
(Reprinted from Kopell, H.P., Thompson, W.A.L., 1959. Pain and the frozen shoulder. Surg Gynecol Obstet 109, 92. By permission of Surgery, Gynecology & Obstetrics, now known as the Journal of the American College of Surgeons.)
In addition, suprascapular neuropathy, which is sometimes confused clinically with a rotator cuff injury, may also accompany a rotator cuff injury. One might initially assume that both have a common traumatic etiology. However, a suprascapular neuropathy may actually occur as a result of a rotator cuff tear, usually a large and full thickness tear. Following a rotator cuff tear, there may be medial retraction of the tendons to the supraspinatus and infraspinatus muscles. This may result in increased tension on the suprascapular nerve both at the suprascapular notch and the spinoglenoid notch (Figure 31–3).
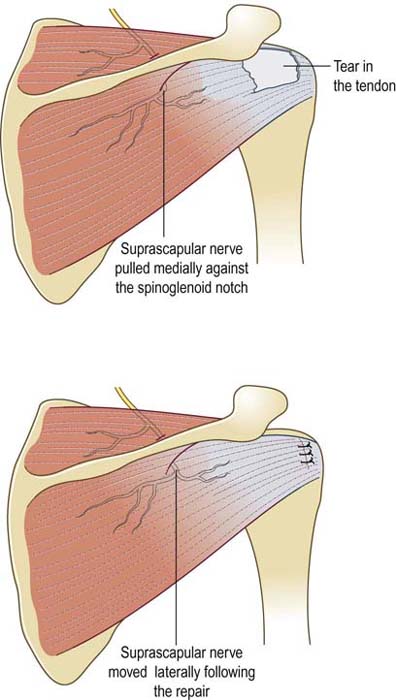
FIGURE 31–3 Suprascapular neuropathy and rotator cuff tear.
(Adapted with permission of Elsevier, from: Costouros, J.G., Porramatikul, M., Lie, D.T., Warner, J.J.P., 2007. Reversal of suprascapular neuropathy following arthroscopic repair of massive supraspinatus and infraspinatus rotator cuff tears. Arthroscopy 23, 1152–1161.)
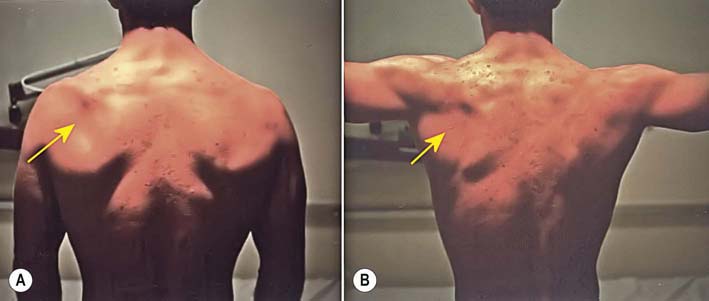
Symptoms and signs depend on the site of nerve entrapment. At the most common site of entrapment, the suprascapular notch, shoulder pain may be prominent. Indeed, there is anatomic and clinical evidence that the suprascapular nerve supplies the majority of deep sensory fibers (including pain fibers) to the shoulder joint. The pain typically is described as deep and boring, occurring along the superior aspect of the scapula and radiating to the shoulder, but usually not more distally. The pain may be exacerbated by shoulder movements, especially adduction of the extended arm. This movement results in protraction of the scapula, which increases the nerve tethering between the upper trunk and the suprascapular notch. Occasionally, the suprascapular notch may be tender to palpation. Weakness involves shoulder abduction (supraspinatus) and external rotation (infraspinatus). Impairment of these motions may or may not be noticed by the patient, because both functions are subserved by other muscles as well. Atrophy may be recognized, especially over the infraspinatus muscle, which is only partially covered by the trapezius muscle (Figure 31–4).
Lastly, neuralgic amyotrophy often presents with severe proximal arm and shoulder pain and later weakness (see Chapter 30). In some cases, the suprascapular nerve may be primarily involved. However, close clinical and electrophysiologic evaluation usually reveals evidence of more widespread involvement of other nerves.
Electrodiagnosis
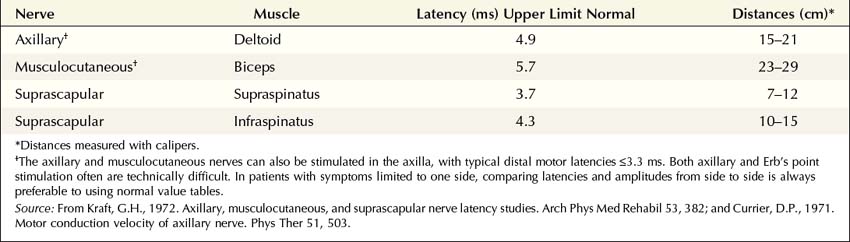
Motor conduction studies can be performed, stimulating Erb’s point and recording with a monopolar needle electrode in either the supraspinatus or infraspinatus muscle, or both, simultaneously (Table 31–1). A surface recording electrode should not be used to record from the spinati muscles, especially the supraspinatus, because they are covered by the trapezius. A surface reference electrode is placed distally over the shoulder joint. Compound muscle action potential (CMAP) amplitude and latency are measured. Comparing amplitude side to side can give an estimate of the amount of axonal loss present. However, these studies generally do not increase the yield over conventional EMG in terms of localizing the lesion. Typically, the pathophysiology of these entrapment neuropathies is axonal loss. Thus, although motor nerve conduction studies may show reduced amplitudes and slightly prolonged latencies, there really is no information gained over needle EMG, which more easily demonstrates axonal loss. When Erb’s point stimulation is performed, high stimulating currents often are required, and supramaximal stimulation can be difficult to ensure.
Axillary Neuropathy
Anatomy
Along with the radial nerve, the axillary nerve originates from the posterior cord of the brachial plexus (Figure 31–5). The axillary nerve is composed primarily of C5–C6 fibers, running through the upper trunk and posterior cord of the plexus. The nerve leaves the axilla through the quadrilateral space, which is formed by the humerus and the teres minor, teres major and long head of the triceps muscles (Figure 31–6). Posteriorly in the quadrilateral space, it often divides into two major trunks. The posterior trunk always supplies the teres minor before terminating as the superior lateral brachial cutaneous nerve (i.e., axillary sensory nerve). The teres minor aids in external rotation of the shoulder while the deltoid is principally a shoulder abductor. The axillary sensory nerve supplies an oval-shaped area over the lateral shoulder. The anterior trunk travels deep to the fascia of the deltoid and always supplies the middle and anterior heads of the deltoid as well as a deep sensory branch to the shoulder joint. The posterior head of the deltoid is most commonly supplied by the posterior trunk, but some variations exist wherein it is supplied by the anterior trunk alone, and in others by a combination of the anterior and posterior trunks.
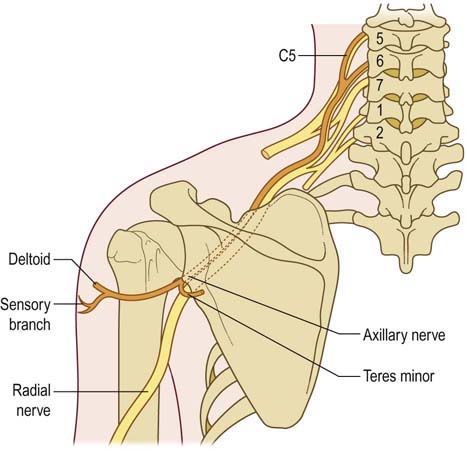
FIGURE 31–5 Anatomy of the axillary nerve.
(Adapted from Haymaker, W., Woodhall, B., 1953. Peripheral nerve injuries. WB Saunders, Philadelphia. With permission.)
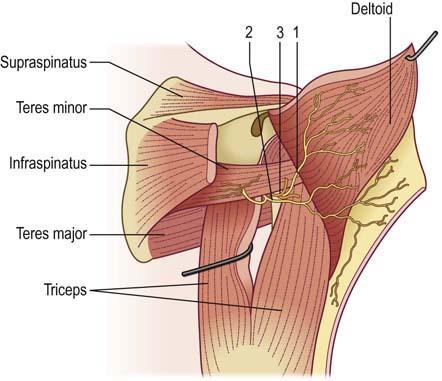
FIGURE 31–6 Posterior view of the quadrilateral space.
Anterior (1) and posterior (2) branches of the axillary nerve and circumflex artery (3).
(From Paladini, D., Dellantonio, R., Cinti, A., et al., 1996. Axillary neuropathy in volleyball players: report of two cases and literature review. J Neurol Neurosurg Psychiatry 60, 345–347. With permission.)
Clinical
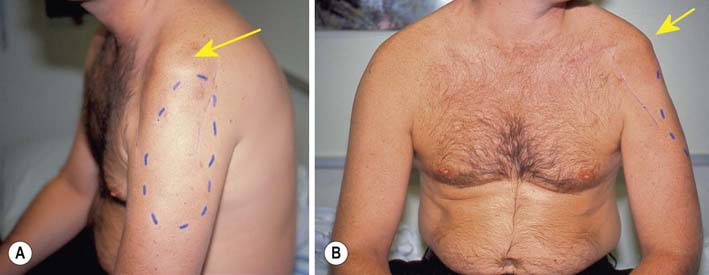
Patients with axillary neuropathies have a well-defined circular area of numbness over the lateral shoulder, along with partial weakness of shoulder abduction and external rotation (Figure 31–7). The degree of weakness varies from patient to patient. The weakness is only partial, because other muscles also contribute to shoulder abduction (i.e., the supraspinatus) and external rotation (i.e., the infraspinatus).
Electrodiagnosis
Axillary motor nerve conduction studies can be performed, stimulating the axilla and Erb’s point and recording with a monopolar needle or surface electrode over the deltoid (Table 31–1). A surface reference electrode is placed distally over the deltoid tendon. To calculate a conduction velocity, distances must be measured with calipers. CMAP amplitude can be compared both from side to side, to assess the amount of axonal loss, and between the axilla and Erb’s point on the symptomatic side, to look for conduction block. These studies can be technically difficult to perform, however, especially obtaining supramaximal stimulation, and are best used to assess axonal loss by comparing the symptomatic side to the asymptomatic side. Because these usually are axonal loss lesions, motor studies generally do not increase the yield of localizing the lesion beyond what is obtained from routine needle EMG.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree