CHAPTER 150 Pseudotumor Cerebri
Terminology
The syndrome known as pseudotumor cerebri (PTC) is generally thought of as a condition characterized by increased intracranial pressure (ICP) without evidence of dilated ventricles or a mass lesion by imaging, normal cerebrospinal fluid (CSF) content, and papilledema occurring in most cases (but not all—see later) in young, obese women without any clear explanation. The terminology used to describe this condition has changed dramatically over time and continues to change as new issues regarding its etiology are raised. The condition was probably first described by Quincke in 18971; however, the term pseudotumor cerebri appears to have first been used in 1914.2 Subsequently, Foley suggested calling the condition “benign intracranial hypertension” because it appeared to have a much more benign neurological prognosis than increased ICP caused by a central nervous system mass lesion or infection.3 Because significant visual morbidity may result from PTC, use of the adjective “benign” is no longer considered appropriate terminology. Instead, most physicians use the term idiopathic intracranial hypertension (IIH) for cases of PTC that occur in young, obese patients and the term secondary pseudotumor cerebri for the rare cases in which a cause (e.g., drug induced) is identified.4,5 The problem with this terminology is that a substantial percentage of patients with so-called IIH have been shown to have some degree of lateral sinus stenosis. At issue is whether the stenosis is the cause or the effect of the increased ICP. If one believes—as many do—that the stenosis is the cause of the condition, patients previously considered to have IIH but who exhibit lateral sinus stenosis may have to be put into the category of secondary PTC, even though they are otherwise identical in body habitus, age, and other features as patients without lateral sinus stenosis. This issue is discussed in more detail later. It suffices here simply to state that (1) one should not use the term pseudotumor cerebri synonymously with idiopathic intracranial hypertension, and (2) some patients previously thought to have IIH because no cause could be identified may now be considered to have a condition caused by stenosis of one or both lateral sinuses. In this chapter I use the terms pseudotumor cerebri to describe the general condition and idiopathic intracranial hypertension when discussing the condition formerly thought to have no identifiable cause but, in some cases, appears to be associated with lateral sinus stenosis. It should also be emphasized that some authors use the term pseudotumor syndrome for patients with increased ICP unassociated with ventricular dilation, evidence of cerebral edema, or an intracranial mass lesion but with abnormal CSF content. This condition occurs in some patients with aseptic, carcinomatous, or lymphomatous meningitis. This chapter deals only with patients who have true PTC, not this “pseudotumor syndrome.”
Epidemiology
PTC affects infants, children, and young adults. The idiopathic form (i.e., IIH), which represents about 90% of cases, is typically a disorder of obese females of childbearing age,5 but it may also occur in men and young children.6 The incidence of IIH varies throughout the world. Two studies in the United States estimated the incidence to be approximately 0.9 per 100,000 in the general population with a female-to-male ratio of 8 : 1.7,8 The incidence increases to 3.5 per 100,000 in women aged 20 to 44 years and further increases to 13 per 100,000 in women who are 10% over ideal weight and 19 per 100,000 in women who are 20% over ideal weight.7 A recent and rapid gain in weight is associated with an increased risk for IIH in both obese and nonobese patients.9,10 All races are affected, and there is evidence that African Americans have a worse prognosis than white individuals regardless of treatment.11 Secondary PTC, which accounts for about 10% of cases, may develop at any age and occurs with equal frequency in both sexes.
Symptoms and Signs
Primary PTC (i.e., IIH) and secondary PTC produce identical symptoms and signs. Occasionally, the condition is asymptomatic and discovered during a routine ophthalmic examination when papilledema is found12; however, the most common symptom, as well as most often the initial symptom, is headache, which occurs in approximately 90% of cases.4,5 The character of the headache is not specific, but it is generally different from previous headaches and is severe.13–15 It most frequently is bifrontal or generalized, pressure-like, and often associated with neck pain.13 The headache usually occurs daily but may be intermittent. Many patients have migrainous features, including unilateral pain, nausea, vomiting, photophobia, and phonophobia.15 It may awaken the patient from sleep or resemble a “brain tumor headache” that is worse in the morning and aggravated when cerebral venous pressure is increased by Valsalva maneuvers (e.g., coughing, sneezing).
The second most common symptom of PTC is transient visual loss. Typical transient obscurations of vision (TOVs) are reported by about 70% of patients.4,5 They may be unilateral or bilateral and generally last only a few seconds. They are thus quite different from the TOVs experienced by patients with carotid artery or cardiac valvular disease, which typically last at least 15 minutes. The TOVs occurring in patients with PTC are often precipitated by a change in posture (e.g., bending over, arising from a stooped position) or rolling the eyes. In some patients, TOVs occur 20 to 30 times a day. The visual loss may be partial or complete. TOVs indicate the presence of optic disc swelling, usually severe, but are not a sign of a poor prognosis. They probably reflect transient ischemia of the optic disc caused by the papilledema.
A small percentage of patients with PTC complain of visual loss that may be characterized as an enlarged dark spot in the temporal visual field. This is caused by enlargement of the physiologic blind spot as a result of severe papilledema. Tunnel vision and central visual loss may occur in more chronic cases13 or acutely from ischemic optic neuropathy.16 The visual loss in patients with PTC may also arise from local associated ocular causes, such as macular hemorrhage, exudates, or accumulation of subretinal fluid.17,18
Diplopia, reported by approximately 40% of patients, is usually horizontal and results from unilateral or bilateral abducens nerve paresis, a nonlocalizing feature of increased ICP.4,5 Rarely, there is vertical diplopia from trochlear nerve paresis, oculomotor nerve paresis, or skew deviation.19
Pulsatile tinnitus is not uncommon in patients with PTC, although such patients rarely mention this symptom unless asked directly about it. Frequently described as a whooshing sound, hearing a heartbeat in the head, or a high-pitched noise, pulsatile tinnitus is thought to reflect flow disturbances within the cerebral venous system.13,20 It may be unilateral or bilateral and is often more prominent at night or in quiet surroundings.
Focal neurological deficits in patients with PTC are extremely uncommon, and their occurrence should make one consider alternative diagnoses21; however, patients with chronic PTC are more likely to be anxious or depressed or feel that they have a worse quality of life than age-matched control subjects.9,10,22 Cognitive deficits are less well substantiated and may be a manifestation of headache-related concentration difficulties, depression, or anxiety.22
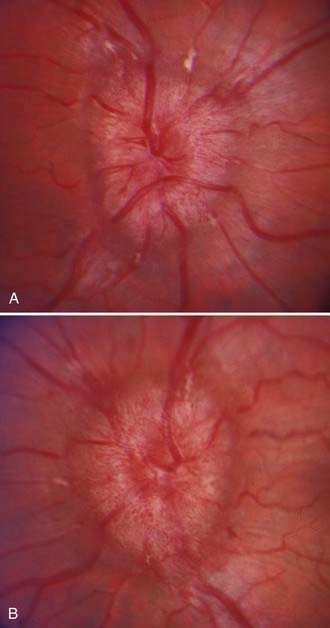
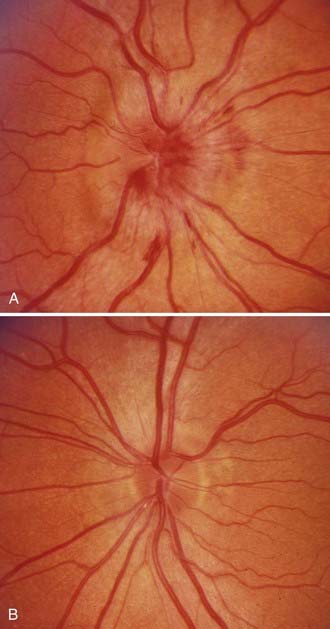
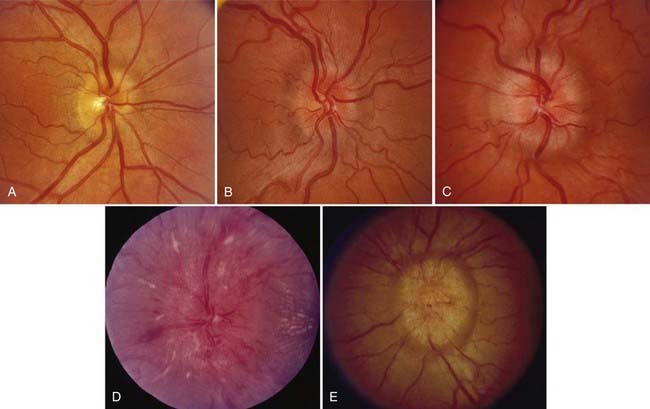
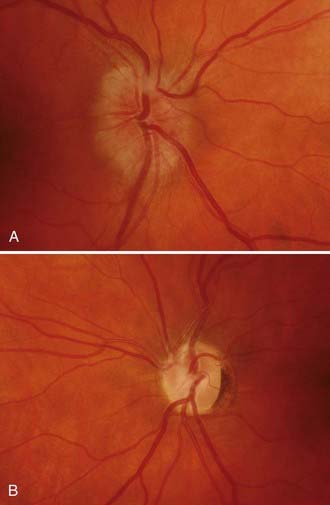
Papilledema is the diagnostic hallmark of PTC and is present in almost all patients.4,5 The papilledema of PTC is identical with that in patients with other causes of increased ICP. It is almost always bilateral and symmetrical (Fig. 150-1), but it may be asymmetric or, occasionally, unilateral (Fig. 150-2).23 Several grading systems for papilledema have been proposed over the years. The system most commonly used is the Frisén system, which separates the appearance of the optic disc into stages ranging from normal appearance (stage 0) to very severe papilledema (stage 5) (Table 150-1 and Fig. 150-3).24 The importance of this grading system cannot be overemphasized because it—along with color vision assessment and visual field testing—is crucial in determining the appropriate management of any patient with papilledema, particularly a patient with PTC. It should also be noted that PTC may occur without papilledema, but it is uncommon and the diagnosis should be made with caution in such a setting, preferably only after continuous CSF pressure monitoring.25
TABLE 150-1 Papilledema Grading System (Frisén Scale)
| Stage 0—Normal Optic Disc |
| Stage 1—Very Early Papilledema |
Disruption of the normal arrangement of radial nerve fiber layers with a grayish opacity accentuating the nerve fiber layer bundles |
| Stage 2—Early Papilledema |
| Stage 3—Moderate Papilledema |
| Stage 4—Marked Papilledema |
| Stage 5—Severe Papilledema |
From Frisén L. Swelling of the optic nerve head: a staging scheme. J Neurol Neurosurg Psychiatry. 1982;45:13-18.
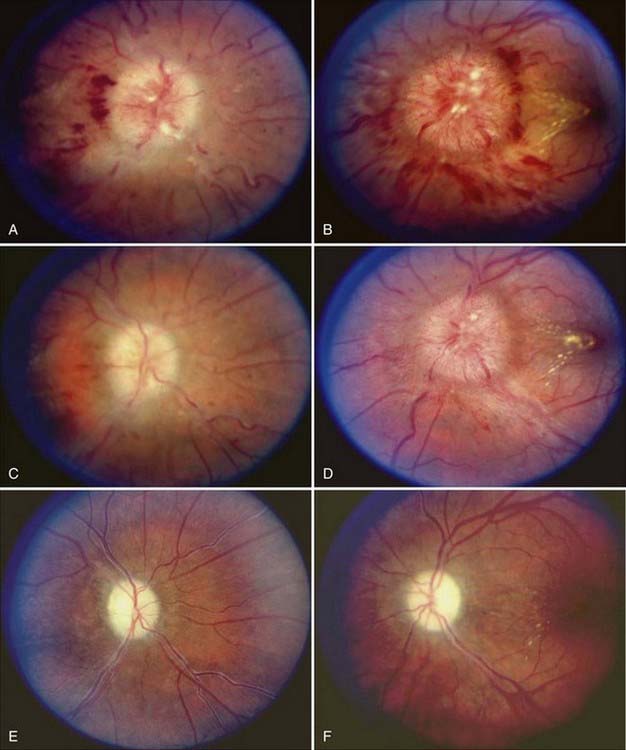
As with papilledema from other causes, loss of central visual acuity is uncommon in patients with PTC unless they have sustained severe damage to the optic nerves or there is an intraocular cause, such as macular hemorrhage or exudates, all of which should be easily visible with an ophthalmoscope. Instead, the visual dysfunction usually begins with visual field defects similar to those that occur in patients with glaucoma (Fig. 150-4). Thus, loss of central acuity in a patient with PTC who has severe papilledema and no evidence of an intraocular cause for the loss of vision indicates an advanced process, requires immediate and aggressive treatment, and confers a poor prognosis for recovery, even if urgent therapy is undertaken immediately.
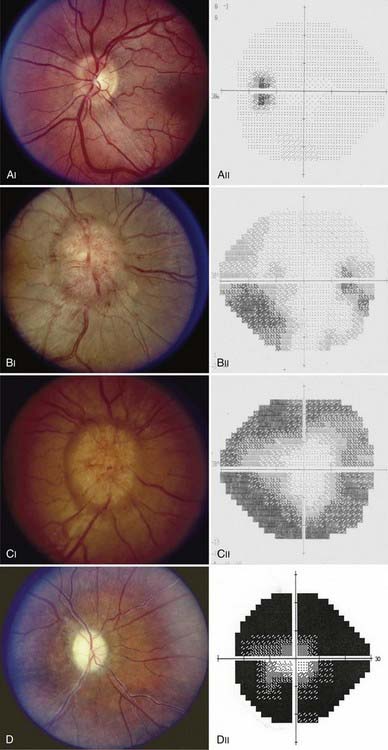
FIGURE 150-4 A-E, Progression of visual field defects in papilledema with corresponding appearance of the optic disc.
Postpapilledema optic atrophy occurs in untreated or inadequately treated patients after a variable period, usually several months, but occasionally within weeks of the onset of symptoms (Fig. 150-5). Some patients have persistent chronic papilledema without visual deterioration or optic atrophy. Postpapilledema optic atrophy in patients with PTC usually develops symmetrically, but just as papilledema may be asymmetric, so postpapilledema optic atrophy can be asymmetric. In some patients a pseudo–Foster Kennedy syndrome develops that is characterized by postpapilledema optic atrophy in one eye and papilledema in the other (Fig. 150-6).26
Diagnosis
The diagnosis of both IIH and secondary PTC requires that there be no intracranial or spinal mass, no evidence of hydrocephalus, documented increased ICP, and normal CSF contents.4,5 Thus, the diagnosis cannot and should not be made without neuroimaging and a lumbar puncture (LP).
Neuroimaging
The rationale for neuroimaging studies in patients with suspected PTC is twofold: first, to exclude a condition such as a tumor producing hydrocephalus or a mass effect that would put the patient at risk for herniation and, second, to ensure that there is no secondary cause of the increased ICP. Although computed tomography (CT) is generally adequate to ensure that the patient will not be at risk when undergoing LP, the resolution of this study is insufficient to exclude certain posterior fossa lesions, isodense lesions not associated with ventriculomegaly, gliomatosis cerebri, meningeal abnormalities, or venous sinus thrombosis.27 Thus, magnetic resonance imaging (MRI) is recommended for most patients.4,5 For children, men, and non-overweight women or patients with symptoms or signs that are atypical for PTC, MR or CT venography should be performed. Indeed, even patients who appear to have the typical clinical picture of IIH may show evidence of venous sinus thrombosis on MR venography.28 Catheter-based angiography with venous-phase sequences may also be needed in such patients if venous sinus thrombosis is suspected and the results of noninvasive venography are equivocal. In addition, I and others have seen patients with apparent IIH who initially had no evidence of venous sinus thrombosis but who then worsened and underwent repeat imaging that subsequently showed venous sinus thrombosis.29
The diagnosis of PTC should not be made in patients with an intracranial or spinal mass lesion; however, about 50% of patients with the condition have an empty sella as a result of the chronically increased ICP. In addition, a small percentage of patients with PTC have a Chiari type I malformation or cerebellar ectopia.30 In some cases, this results from downward pressure on the cerebellar tonsils; however, in other cases, it is thought that the Chiari malformation is the cause rather than the effect of the increased ICP, and in such cases, treatment is directed at the malformation (see later). Finally, as noted earlier, an increasing percentage of patients who in the past would be considered to have IIH are being shown to have unilateral or, occasionally, bilateral lateral sinus stenosis.
Examination of Cerebrospinal Fluid
Examination of CSF is required for the diagnosis of PTC to confirm an elevated opening pressure and to exclude a malignant, infectious, or inflammatory process that might simulate PTC. Normal lumbar CSF pressure in both obese and nonobese adults is 200 to 250 mm H2O, and thus values between 201 and 249 are nondiagnostic.31,32 Consequently, the diagnosis of PTC cannot be made unless the CSF opening pressure is 250 mm H2O or greater. In prepubertal children, a value higher than 200 mm H2O is probably abnormal. Because CSF pressure normally fluctuates, multiple CSF pressure measurements or prolonged CSF pressure monitoring is sometimes required, depending on the clinical circumstance.33 In obese patients, LP may be technically challenging to perform, in which case fluoroscopic guidance is extremely helpful. To ensure accuracy, lumbar CSF pressure must be measured with the patient in the lateral decubitus position, relaxed with the legs partially extended. The pressure may be artifactually elevated if the patient is crying, performing a Valsalva maneuver, or in severe pain.34 CSF should be analyzed for glucose and protein concentration, presence of cells, cytology, and atypical infections (e.g., syphilis, Cryptococcus, fungus). A diagnosis of PTC should not be made unless the CSF contents are completely normal.4,5
Secondary Pseudotumor Cerebri
IIH is a diagnosis of exclusion that occurs primarily in young obese women and, occasionally, in obese men with no evidence of any underlying disease4,5,35,36; however, about 10% of cases of PTC are associated with a number of different conditions. Suspicion of a secondary cause of PTC is heightened in prepubertal children, men, nonobese women, and otherwise typical patients with rapidly progressive visual loss that does not respond to treatment. Secondary causes of PTC include (1) impairment or obstruction of cerebral venous sinus drainage by intrinsic or extrinsic lesions, (2) endocrine and metabolic dysfunction, (3) exposure to exogenous drugs and other substances, (4) withdrawal of certain drugs, and (5) systemic illnesses.4,5,35,36 It is important to realize that although many conditions have been reported to be associated with PTC, relatively few are likely to be true associations. Tables 150-2 to 150-5 list the best substantiated and most frequently observed ones.
TABLE 150-2 Causes of Obstruction/Impairment of Cerebral Venous Drainage Associated with Secondary Pseudotumor Cerebri
| Obstruction of the Superior Sagittal Sinus |
| Obstruction of the Transverse Sinus |
| Occlusion of the Straight Sinus |
| Tumors (extravascular) |
| Occlusion of the Internal Jugular Vein |
TABLE 150-3 Endocrine and Metabolic Disturbances Associated with Pseudotumor Cerebri
TABLE 150-4 Exogenous Substances Whose Exposure, Ingestion, or Withdrawal Has Been Associated with Pseudotumor Cerebri
Get Clinical Tree app for offline access 
|