12 Psychiatry of menstruation and pregnancy
Introduction
Psychiatric disorders are more common in women. Genetic, social and cultural theories have been put forward to explain these findings. Table 12.1 shows psychiatric disorders for which the prevalence is different between men and women. The lifetime risk of developing bipolar mood disorder or schizophrenia is, however, equal in males and females.
Table 12.1 Psychiatric disorders more common in men or women
| More common in men | More common in women |
|---|---|
| Alcoholism (eight times) | Senile dementia |
| Mental retardation | Dysthymia |
| Criminal behaviour, especially violence | Unipolar psychotic depression |
| Completed suicide | Anxiety and phobic disorders |
| Dissociative (conversion) disorders | |
| Anorexia nervosa (nine times) | |
| Bulimia nervosa | |
| Deliberate self-harm |
Premenstrual syndrome (PMS) (late luteal-phase dysphoric disorder)
Clinical features
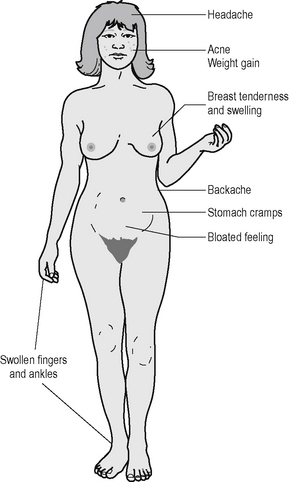
Over 150 symptoms of PMS have been described. Among the most common are psychological symptoms such as tension, irritability, depression, fatigue and poor concentration. Physical symptoms are shown in Figure 12.1.
Investigations and diagnosis
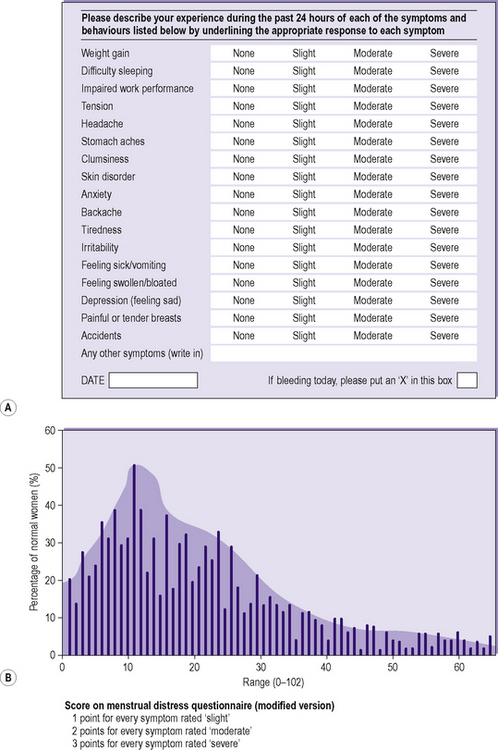
Diagnosis depends predominantly on confirming the timing of symptoms in relation to menstruation, i.e. symptoms begin in mid-cycle, they increase in number and severity to maximum intensity the day before the onset of menstruation, and this is followed by rapid and complete resolution of symptoms. The woman should be advised to keep a diary for at least two months of daily ratings of common menstrual cycle symptoms, using a standard symptom record chart (Figure 12.2) to help confirm the diagnosis.
Management
Pyridoxine (vitamin B6) may provide some benefit.
Pregnancy
Postpartum psychiatric disorders
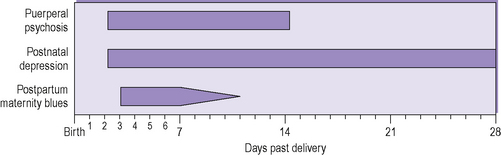
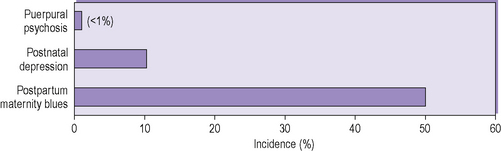
The postpartum period is a time of increased psychiatric disorder: in some studies an increase of up to 18 times has been found (Figures 12.3 and 12.4). Psychiatric disorders termed postpartum are usually taken to include those with an onset up to about 12 weeks following delivery, although other definitions vary from an onset of six weeks to up to one year post delivery. Psychoses are referred to as postpartum when onset is from six weeks up to one year post delivery. Psychoses in which onset is after six weeks have also been referred to as lactational psychoses. Clearly, the longer the period from delivery to onset, the less likely there is to be a direct relationship between the two. In the past, puerperal or lactational psychoses were seen as a specific, unitary psychiatric disorder. Nowadays, they are seen as a group of psychiatric illnesses, such as depressive disorder or schizophrenia, which can occur at other times. They are not classified separately in ICD-10 or DSM-IV-TR.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree