7 Psychoactive substance use disorders
Introduction
The administration of a psychoactive substance can lead to relatively rapid central nervous system (CNS) effects, including a change in the level of consciousness or the state of mind. This chapter considers the effects of alcohol and other psychoactive drugs, both illicit (such as cocaine and heroin) and licit (such as caffeine). Table 7.1 gives the ICD-10 classification of these disorders. First, however, it is necessary to define some of the terms used.
Table 7.1 ICD-10 classification: F10–F19 mental and behavioural disorders due to psychoactive substance use
| F10 Mental and behavioural disorders due to use of alcohol |
| F11 Mental and behavioural disorders due to use of opioids |
| F12 Mental and behavioural disorders due to use of cannabinoids |
| F13 Mental and behavioural disorders due to use of sedatives or hypnotics |
| F14 Mental and behavioural disorders due to use of cocaine |
| F15 Mental and behavioural disorders due to use of other stimulants, including caffeine |
| F16 Mental and behavioural disorders due to use of hallucinogens |
| F17 Mental and behavioural disorders due to use of tobacco |
| F18 Mental and behavioural disorders due to use of volatile solvents |
| F19 Mental and behavioural disorders due to multiple drug use and use of other psychoactive substances |
| Four- and five-character codes may be used to specify the clinical conditions: |
| F1x.0 Acute intoxication |
| F1x.1 Harmful use |
| F1x.2 Dependence syndrome |
| F1x.3 Withdrawal state |
| F1x.4 Withdrawal state with delirium |
| F1x.5 Psychotic disorder |
| F1x.6 Amnesic syndrome |
| F1x.7 Residual and late-onset psychotic disorder |
| F1x.8 Other mental and behavioural disorders |
| F1x.9 Unspecified mental and behavioural disorder |
Definitions
Withdrawal state. This is a group of physical and psychological symptoms occurring on absolute or relative withdrawal of a psychoactive substance after repeated, and usually prolonged and/or high-dose, use of that substance. The onset and course of the withdrawal state are time-limited and are related to the type of substance and the dose being administered immediately prior to abstinence. The withdrawal state may be complicated by delirium (see Chapter 6) and/or convulsions.
Alcohol problems
Excessive consumption
Units of alcohol
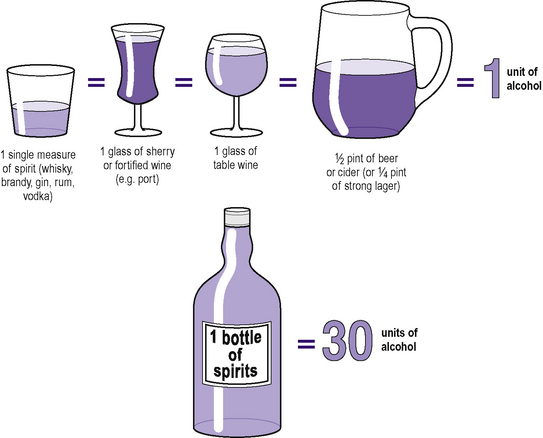
In the assessment of alcohol consumption it is useful to have a standardized measure of alcohol. It has been found that the amount (mass) of alcohol contained in a standard measure of spirits, in a standard glass of sherry or fortified wine, a standard glass of table wine, and in one half-pint of beer or lager of standard strength (3–3.5% by volume) is approximately the same, at 8–10 g. This amount is known as a unit of alcohol (Figure 7.1). Note that some (European continental) lagers can be as strong as 5–6% by volume, and some wines can be as strong as 17% (or even higher) by volume; the figures given in Figure 7.1 have to be adjusted accordingly in such cases. Also, although Figure 7.1 considers 25 mL to be a standard measure for spirits, some public houses and bars now use larger ‘standard’ measures for spirits, so that the number of units of alcohol is correspondingly higher.
Levels of consumption
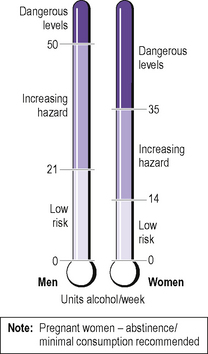
The Royal College of Physicians has defined low-risk levels of alcohol consumption as being up to 21 units per week for men and up to 14 units per week for women (Figure 7.2). This amount of alcohol should not be consumed in one go, and alcohol should not be consumed every day, for these levels to apply.
Alcohol consumption in greater amounts constitutes excessive consumption and carries a much greater risk of developing alcohol-related disabilities and alcohol dependence. The definitions of increasing hazard and dangerous levels of alcohol consumption are also shown in Figure 7.2.
Alcohol-related disabilities
Excessive alcohol consumption can lead to physical, psychiatric and social morbidity.
Physical (medical) morbidity
Hepatic damage takes place chronologically in the following order:
Haematological complications include:
Cancer of the oropharynx, oesophagus, pancreas, liver and lungs is increased in incidence.
Excessive alcohol consumption in pregnancy can lead to permanent fetal damage. The clinical features of the consequent presentation of the fetal alcohol syndrome following birth are shown in Figure 7.3.
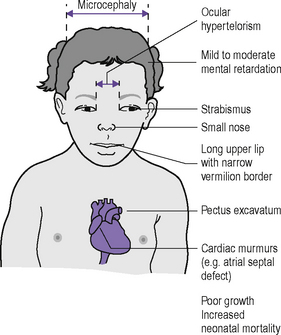
Figure 7.3 • Fetal alcohol syndrome in a child whose mother consumed excess alcohol during pregnancy.
Accidents and trauma may result from alcohol consumption. These include:
Psychiatric morbidity
Alcohol also affects the personality of the drinker, who may initially drink to achieve such superficial effects as appearing more sociable and sexually desirable. However, the effects of chronic heavy drinking on personality are often negative, causing boastfulness, embarrassing speech and actions and offensiveness. With persistent heavy drinking personality deterioration occurs, which may simulate a personality disorder (see Chapter 15).
In chronic heavy drinkers, a fall in the blood alcohol concentration leads to withdrawal symptoms (see below). These include delirium tremens or DTs. The features of delirium have been described in Chapter 6. Another important withdrawal symptom is withdrawal fits, which may occur within 48 hours of stopping drinking.
Chronic heavy drinking is one cause of pathological (delusional) jealousy (see Chapter 8). Alcohol is also a cause of fugue states (see Chapter 11).
Heavy drinking is often associated with gambling and the use of other psychoactive substances. It can also be a cause of dementia (see Chapter 6).
Social morbidity
The social costs of excessive alcohol consumption are very high, and include the following:
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree