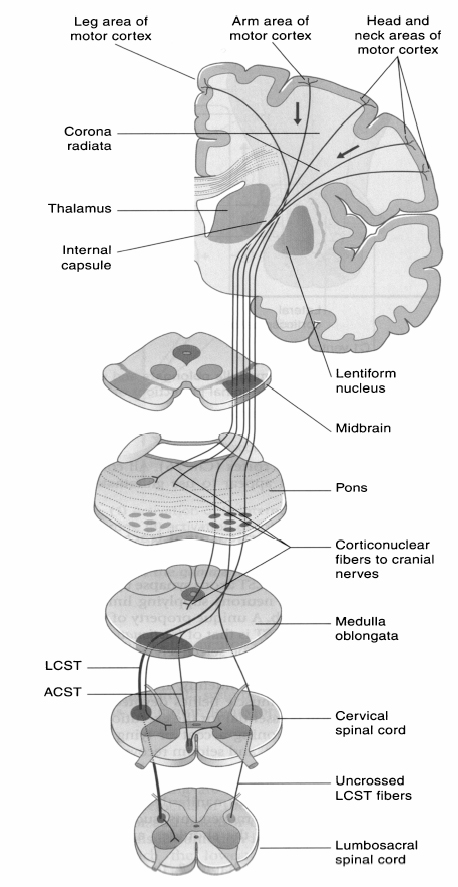
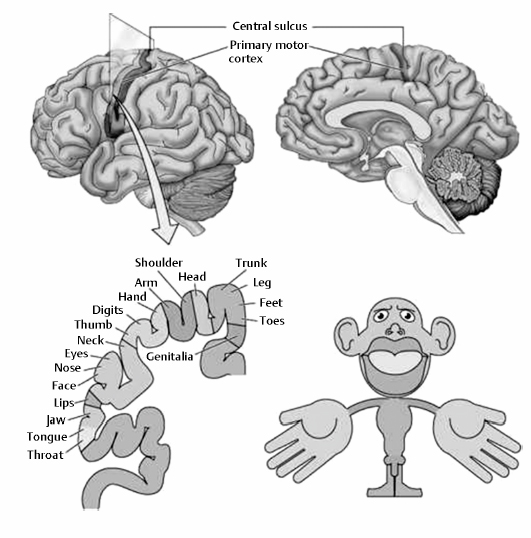
Chapter 19 Diseases of the larynx encompass a wide spectrum of problems including inflammation, cysts, benign and malignant tumors, and trauma. This chapter focuses on problems of pharyngolaryngeal function associated with pyramidal disease (i.e., stroke) and consequent dysphagia. It also discusses some new research in assessing the neuroanatomy of the pharyngolarynx and swallowing. Problems with speech (dysphonia) are briefly covered. As the name suggests, the pyramidal tracts, better known as the corticospinal tracts (CSTs) and corticobulbar tracts (CBTs), are a set of approximately one million nerve fibers that travel down from the motor cortex to the spinal cord and are predominantly involved in the regulation of all voluntary movements, in particular discrete, skilled movements. They are composed of cortical neurons, named pyramidal cells because their cell bodies resemble small pyramids, that collectively give rise to the single most important output tract of the motor cortex. They have an average conduction velocity of 60 m/s, indicating an average fiber diameter of 10 μm; however, fibers arising from the leg area of motor cortex can be up to 20 μm in diameter and account for approximately 3% of the total number of fibers. Approximately 80% of the tracts extend from upper motor neurons in the primary motor cortex to lower motor neurons in the anterior horn of the spinal cord as shown in Fig. 19.1 , with the remaining 20% of fibers originating in the premotor cortex and supplementary motor area. Upper motor neurons reside in the precentral gyrus of the frontal lobe, also known as the “motor strip,” and are arranged in a somatotopic fashion. Neurons controlling facial movements are located near the sylvian or lateral fissure, whereas neurons controlling limb muscles are located near the medial longitudinal fissure and within the central sulcus. The representations of the various body parts are often depicted graphically by a distorted human figure known as the motor homunculus as shown in Fig. 19.2 . Fig. 19.1 The corticospinal/pyramidal tracts. The pyramidal shape of the axons lead to the term pyramid. The corticobulbar tracts are also referred to as the corticonuclear tracts by some authors. (From FitzGerald MJT, Folan-Curran J. Spinal cord: descending pathways. In: FitzGerald MJT, Folan-Curran J, eds. Clinical Neuroanatomy and Related Neuroscience. 4th ed. Philadelphia: WB Saunders, an imprint of Elsevier Science; 2002:125. Reprinted with permission from Elsevier.) Fig. 19.2 The motor homunculus. The disproportionate anatomy of the homunculus arises from the number of neurons that innervate that area. The larger the body part the greater the number of innervating neurons.(From Purves D, Augustine GJ, Fitzpatrick D, Katz LC, LaMantia AS, McNamara JO. Descending control of spinal cord circuitry. In: Purves D, et al, eds. Neuroscience. Sunderland, MA: Sinauer Associates; 1997:316. Reprinted with permission from Sinauer Associates.) Axons extending from upper motor neurons in the motor strip traverse deep brain matter through the corona radiata and coalesce to form the internal capsule of the forebrain and then descend through the midbrain in the cerebral peduncle. Here axons of the CST condense and form the structure known as the pyramids; as in the motor strip, these axons are also arranged somatotopically. Axons innervating facial muscles are located medially and are collectively known as the CBT. These axons exit at their appropriate levels to synapse with their lower motor neurons in the cranial nerve nuclei. Axons innervating limbs are located laterally within the cerebral peduncle and are thus known as the lateral CST (LCST). These axons aggregate to form the pyramids in the medulla oblongata, hence the term pyramidal tract. In the distal medulla, approximately 80% of CST axons cross to the contralateral side in a very distinct area (on cross section) known as the pyramidal decussation. The pyramidal decussation separates the medulla, above, from the spinal cord, below. Injuries to upper motor neurons in the cortex or their axons prior to entering the pyramidal decussation result in contralateral spastic paralysis, whereas injuries below the decussation or to the lower motor neurons in the spinal cord usually cause ipsilateral flaccid paralysis. Approximately 10% of axons that do not cross over continue from here to join the lateral CST. The remaining 10% of axons that also do not cross over form the anterior CST (ACST) and supply motor neurons serving deep muscles in the neck. Beyond the pyramidal decussation, the upper motor neurons synapse on lower motor neurons in the anterior horn of the spinal cord, exiting via the ventral root. Damage to lower motor neurons can also cause flaccid paralysis. The ventral root then joins the dorsal root to form the spinal nerve, which finally innervates skeletal muscles. Pathologic processes that damage the pyramidal tracts (Table 19.1) are often associated with disability and suffering and are thus grouped together as pyramidal disease. Stroke is the main pathologic condition affecting the pyramidal tracts that will be discussed in this chapter.
Pyramidal Disease
Neuroanatomy of the Pyramidal Tracts
Definition of Pyramidal Disease
| Multiple sclerosis (MS) |
| Motor neuron disease (MND) |
| Space occupying lesions that affect the pyramidal tracts |
| Stroke |
A stroke, or cerebrovascular accident, is the temporary or permanent loss of functioning brain tissue due to an interruption in the blood supply. There are two classifications of stroke: (1) those resulting from full or partial blockage of an artery, which is called an infarct; and (2) those caused by hemorrhages or ruptures of intracranial blood vessels. Regardless of the type, stroke is a devastating affliction resulting in a catastrophic cerebral injury that removes both independence and dignity from many of its survivors. It is also the most common cause of pyramidal tract disease, and is recognized to affect pharyngolaryngeal function, resulting in conditions such as dysphagia,1 dysphonia,2 dysphasia,3 and dysarthria.4
Role of Pharyngolarynx in Swallowing
The three functions of the pharyngolarynx are (1) protective, (2) respiratory, and (3) phonatory. This chapter focuses on the protective role of the pharyngolarynx during swallowing.
Normal Swallowing Function
For most people, swallowing or deglutition is a normal and effortless task, but despite its effortlessness, it is a complex and dynamic sensorimotor activity involving 26 pairs of muscles and five cranial nerves. The complexity of the swallowing process is a consequence of the common shared pathway between the respiratory and gastrointestinal tracts that has arisen to avoid the threat of food or liquid entering the airway. Therefore, swallowing enables the safe delivery of ingested food, as a bolus, from the mouth to the stomach while ensuring protection of the airway. It is an integral component of feeding learned during gestation, organized at birth,5 and essential for the continuation of life.
Traditionally, swallowing is divided into three conventional phases: (1) oral, (2) pharyngeal, and (3) esophageal. Mastication and the oral phase refer to the volitional transfer of ingested material, as a bolus, from the mouth into the oropharynx and is controlled by the motor cortex and premotor areas of the brain.
During the oral phase food is taken into the mouth, manipulated, mixed with saliva, and formed into a bolus. This repetitive cycle of chewing is bolus dependent and regulated via sensory receptors in the tongue, alveolar ridge, and infrahyoid structures, which modify the activity of motor neurons in the trigeminal nucleus.6 A sophisticated peripheral feedback mechanism prevents injury to the oral structures and gives proprioceptive feedback about bolus position. Once prepared, the bolus is held in a central groove formed by the positioning of the tongue against the hard palate.7 It is prevented from moving backward by closure of the velum against the pharyngeal aspect of the posterior tongue, which acts as a gateway to the hypopharynx and allows continued respiration.
Once the bolus has been adequately prepared, the oral phase of the swallow commences. The velum elevates, the lips and buccal muscles contract, the posterior aspect of the tongue depresses, and the remainder of the tongue presses against the hard palate to propel the bolus to the hypopharynx.8 At the point where the bolus passes the anterior faucial arches, the oral stage of swallowing is complete, usually taking less than one second.
The pharyngeal phase is the first reflexive component triggered by activation of the central pattern generator in the brainstem, which subsequently controls muscles in the oropharynx to deliver the bolus from the oropharynx to the relaxed cricopharyngeal muscle (upper esophageal sphincter, UES). The oropharyngeal swallow has been described as a single pressure-driven event during which the mouth and pharynx form a continuous tube with four valves: the lips, velopharyngeal port, larynx, and UES.9
As the bolus is pushed backward by the tongue, there is a rise in intraoral pressure that marks the beginning of a series of pressure changes that occur during swallowing.10 A peristaltic-like wave activated by contraction of the constrictor muscles occludes the pharynx by squeezing together the pharyngeal walls behind the bolus.11
The nasopharynx is blocked off by the elevation of the soft palate and retraction of the tongue base. The palatopharyngeal folds are pulled together to form a cylindrical passage for the bolus, and the intrinsic muscles of the pharynx shorten, eliminating the pharyngeal recesses. Laryngeal closure is necessary to avoid aspiration and is achieved by a fixed sequence of motor events, which involves cessation of respiration, adduction of the vocal cords, approximation of the arytenoids, laryngeal ascent, and epiglottic descent.12 The elevation of the larynx also seats the epiglottis over the laryngeal vestibule as a secondary level of airway protection.
Upon closure of the UES, the esophageal phase of swallowing begins. This second reflexive component serves the primary function of transporting food from the UES to the stomach through the lower esophageal sphincter. The sequential contraction of muscles initiated in the pharynx continues down the esophagus and in combination with gravity pushes the bolus down the esophagus. Relaxation of the lower esophageal sphincter allows passage of the bolus into the stomach for digestion.
Sensation
Sensory input to the swallowing tract has three primary functions: (1) to assist in initiating swallowing, (2) to modify the threshold for a pharyngeal swallow, and (3) to alter the level of muscle recruitment during swallowing.
Appropriate preparation of food is reliant upon continuous sensory feedback from receptors in the tongue, soft palate, floor of mouth, and tooth pulp, which detect the size and texture of the bolus, thereby determining the chewing action required from masticatory muscles. The pharyngeal phase of swallowing relies on sensory input from the posterior oral region and pharynx to initiate the response.13 The intensity of pharyngeal muscle activity and overall duration of this phase are not constant, and in fact vary in response to sensory information relayed from afferent receptors about the unique characteristics of the bolus.14 Topical anesthesia of these mucosal regions increases the time to evoke repeated swallows and may disrupt swallowing modulation but does not eliminate swallowing completely.15
Sequential Swallowing
Much of what is known about swallowing physiology has been derived from studying single (discrete) swallows. However, the physiology of drinking, a more spontaneous activity composed of multiple swallows (known as sequential swallowing) is a prevalent behavior that warrants our further attention. Recent studies have suggested that two types of sequential swallowing can be observed that vary in their laryngeal closure patterns.16 In type 1 participants, the larynx rises and lowers for each separate bolus, whereas in type 2, the larynx stays elevated throughout a sequence of bolus ingestions. Both closure patterns are associated with laryngeal penetration, and older participants having significantly higher penetration-aspiration scores,17 something that has not been found in the study of discrete swallows. Sequential swallows have also been described as being “significantly shorter than discrete swallows in oral transit, pharyngeal response, UES opening, and total swallow durations, but significantly longer in pharyngeal transit and stage transition durations.”18
Innervation
Motor innervation of the pharynx and larynx is provided through several cranial nerves (CNs) including CN V (trigeminal), XI (glossopharyngeal), and X (vagus) and its branches. A detailed description of laryngeal sensory and motor innervation has been covered earlier in this book and so will not be discussed here.
All the muscles of the pharynx are innervated by the pharyngeal plexus of nerves, which run along its lateral aspect, except the stylopharyngeus, which receives its motor innervation from CN IX. The inferior constrictor is also supplied by additional branches from the external laryngeal and recurrent laryngeal nerves.
The pharyngeal plexus is formed by CNs IX and X and by sympathetic branches from the superior cervical ganglion. Motor fibers are derived from the cranial root of CN XI (the accessory nerve), and are carried by the vagus to all muscles of the pharynx and soft palate, except the stylopharyngeus (supplied by glossopharyngeal) and the tensor veli palatini (supplied by CN V3, the mandibular branch of the trigeminal). Pharyngeal sensory innervation is supplied by the CN IX and the superior laryngeal nerve (SLN) (part of CN X).
Swallowing Dysfunction
Difficulty swallowing, termed dysphagia, is identified as a major clinical problem and can occur during either oropharyngeal or esophageal phases of swallowing. The causes of dysphagia may be neurologic, mechanical, or obstructive in origin, but all have the same outcome: a disruption of bolus flow. This places patients at considerable risk of morbidity and mortality, and particularly at risk for aspiration pneumonia.19 For the purpose of this chapter, we discuss only oropharyngeal dysphagia, which can be subdivided into structural and neurogenic in origin.
Structural dysphagias (Table 19.2) refer to congenital malformations of the lip or palate and usually cause dysphagia from infancy. In adult life, structural resections of the tongue, mandible, pharynx, or neck due to carcinoma are associated with marked swallowing difficulty.
| Amyloidosis |
| Cervical spine osteophytes |
| Congenital anatomic abnormalities, e.g., cleft palate |
| Iron and B12 deficiency |
| Oral malignancies of the tongue and palate |
| Pharyngeal malignancy of the epiglottis, tongue base, or larynx |
| Salivary gland disease |
| Skull base tumors |
| Thyroid disease |
| Thyroid tumors |
| Zenker’s diverticulum |
Neurogenic dysphagias (Table 19.3) refer to those that have a neurologic basis. Some have a slow onset, associated with progressive neurologic conditions such as Parkinson disease, motor neuron disease, or myasthenia gravis.20 Others have a sudden onset associated with acute brain injury such as stroke and head trauma.21
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







