Figure 70-1 The baroreflex arc. Baroreceptor afferents (dark blue) synapse at the nucleus of the tractus solitarius (NTS). The vagal baroreflex pathway (green) runs from the NTS to the nucleus ambiguus (NA) and sends efferents to the sinoatrial node (SA). The adrenergic baroreflex pathway (red) runs from the NTS to the caudal ventrolateral medulla (CVLM) and from there to the rostral ventrolateral medulla (RVLM). The adrenergic pathway continues with sympathetic efferents from the RVLM to the interomediolateral thoracic spinal cord and from there to autonomic ganglia and to the heart, arterioles, and venules.
(Reprinted with permission from Low PA, Singer W. Management of neurogenic orthostatic hypotension: an update. Lancet Neurol 2008;7[5]:451–8.)
Chronic baroreflex failure, especially if sympathetic efferents are affected, results in the triad of orthostatic hypotension, supine hypertension, and a loss of homeostatic ability to vary blood pressure, while acute baroreflex failure often results in a limited blood pressure buffering capacity resulting in paroxysmal hypertension and tachycardia due to loss of tonic inhibitory influence of baroreceptors on sympathetic tone.1,2
Treatment of chronic baroreflex failure is symptomatic and similar to treatment of orthostatic hypotension in general. Clonidine, a centrally and peripherally acting α-adrenoreceptor and imidazoline agonist, has been shown to reduce both frequency and severity of paroxysmal hypertension due to uninhibited sympathetic activity.3,4
CASE REPORT
A 60-year-old man presented for evaluation of generalized weakness. He denied focal muscle weakness, muscle fatigability, or excessive daytime sleepiness. However, he did report the insidious onset of loss of stamina, a generalized sensation of weakness, and exercise intolerance over the course of 3 to 4 years. He described a sensation of his arms and legs feeling “like rubber,” and standing activities such as shoveling snow had become difficult. Also, he experienced frequent lightheadedness when assuming the upright position. He reported longstanding static hand and foot paresthesias.
His past medical history was complicated. He had a history of Hodgkin’s disease and had received neck irradiation 16 years earlier, a history of idiopathic asymmetric bilateral brachial plexitis 9 years ago with almost complete recovery, and a left ulnar neuropathy 3 years earlier treated with nerve transposition at the elbow.
On physical examination, we found weakness limited to the left ulnar-innervated hand muscles. Reflexes were decreased in the upper extremities, and normal in the lower extremities. Plantar responses were flexor. Sensory examination revealed decreased sensation to touch and pinprick in the left ulnar distribution, and decreased sensation to pinprick and vibration in both feet. Stance and gait examination was normal.
Extensive laboratory work was negative except for evidence of mild renal insufficiency. Genetic testing for hereditary neuropathy with pressure palsies (HNPP) was negative. Head magnetic resonance imaging (MRI) scan showed some pontine signal changes, which appeared nonspecific but consistent with radiation effects. MRI of the cervical spine was normal except for mild degenerative changes. Electromyography (EMG) showed no evidence of a myopathy or polyradiculopathy but did show evidence of a longstanding left ulnar neuropathy, residua of an old left upper trunk brachial plexopathy, and a long-standing length-dependent peripheral neuropathy.
Thermoregulatory sweat test showed an area of anhidrosis involving the neck and medial shoulder region in the area of prior radiation (Fig. 70-2). Autonomic reflex screen showed normal postganglionic sudomotor function and normal heart rate responses to deep breathing (Fig. 70-3). However, heart rate responses to the Valsalva maneuver were markedly reduced. Late phase II and phase IV of the blood pressure responses to the Valsalva maneuver were also reduced (Fig. 70-4), and there was evidence of symptomatic orthostatic hypotension with head-up tilt. Based on the results of autonomic testing, a diagnosis of radiation-induced baroreflex failure was made, which is supported by the following considerations:
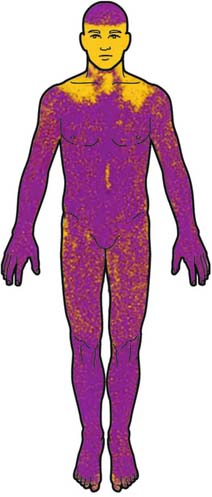
Figure 70-2 Thermoregulatory sweat test. The area of prior radiation is delineated by anhidrosis involving the neck and medial shoulder regions (local effects). Computerized drawing of sweat distribution. Note that indicator powder is not applied to the face because it may be irritating to mucous membranes and the delicate skin of the face.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








