Radiation Physics and Safety
Neuroendovascular surgery involves an extensive list of equipment, devices, and techniques. However, one element is ever-present but intangible, colorless, odorless, and largely unnoticed—radiation, without which no neurointerventional procedure would be done. Knowledge of radiation, from the basic physical principles that govern its behavior to safety measures that can reduce exposure to not only the patient but also the interventionalist, is paramount.
Physics of Fluoroscopy
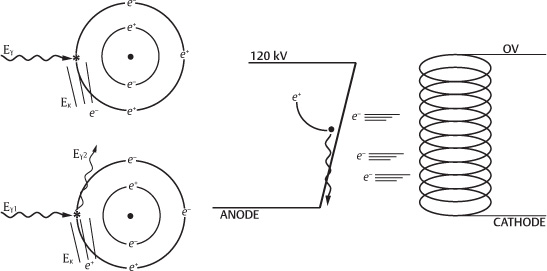
Fluoroscopy involves imaging the body using radiation, which is defined as the transfer of energy in the form of particles or waves. In most fluoroscopy units, a tungsten target is bombarded with energized electrons, where approximately 1% of their kinetic energy is transformed into waves of photons of electromagnetic radiation, called X-rays. X-rays, which contain more energy than other forms of electromagnetic radiation (e.g., ultraviolet, infrared, microwaves, or visible light), have sufficient energy (>30 eV) to cause ionization, where an outer shell electron is displaced (Fig. 5.1).1
To generate X-rays, a cathode, consisting of a heated filament, generates high-energy electrons, which are accelerated to the tungsten target by the aid of an anode, that is, a high-voltage terminal that attracts the electrons. The energy gained by the electron is equal to the potential difference between the anode and the cathode. As the electrons interact with the tungsten nucleus, they release energy in the form of X-rays, whose production is termed braking (deceleration) or bremsstrahlung radiation.
The distribution of X-ray energy levels is continuous, given the variable degree of interactions by the accelerated electrons with the tungsten target. Most low-energy X-rays are either absorbed within the fluoroscopy unit or filtered out using various techniques, which contribute to reducing X-ray exposure levels. Some X-rays are produced with a discrete level of energy and are termed characteristic X-rays. The resulting X-ray spectrum therefore consists of characteristic and bremsstrahlung radiation.1
Components of the Angiography Suite
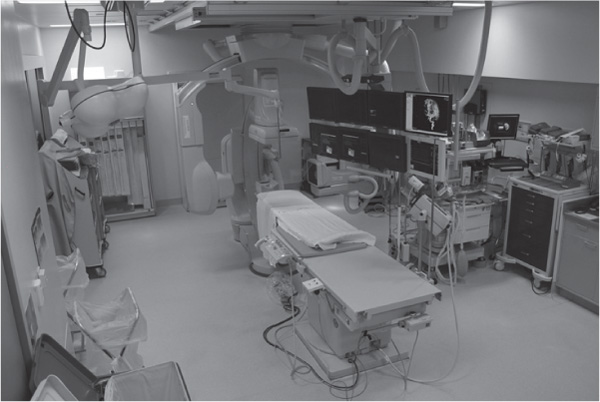
Most modern angiography suites consist of a biplane angiography unit, capable of simultaneous imaging of two image planes using two X-ray tubes (anteroposterior and lateral planes), and either two image intensifiers or flat-panel digital detectors (Fig. 5.2), the angiographic table, and a suspended rack of monitors, which display a variety of information, including but not limited to the current angiographic views, the patient’s vital signs and cardiac monitoring, and saved images for roadmapping or 3D volume-rendered images. The X-ray tube/intensifiers/detectors have the ability to rotate 360 degrees in the anteroposterior plane while the movement in the craniocaudal plane is limited due to the table. As a result, most angiographic views can be obtained.
Fig. 5.1 Production of X-rays through bremsstrahlung radiation.
Fig. 5.2 Standard interventional suite.
Dynamic Fluoroscopy
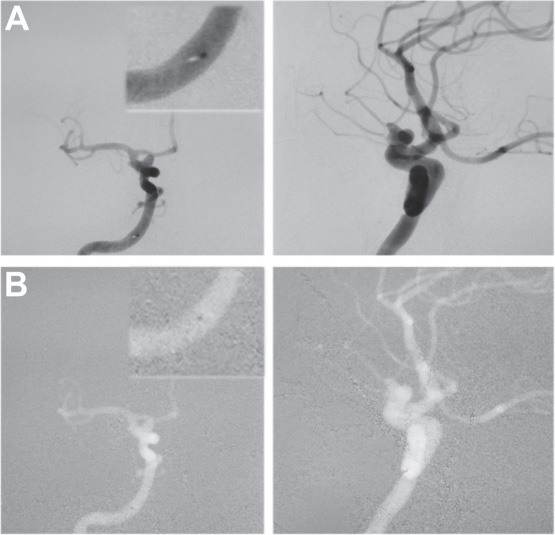
Dynamic fluoroscopy allows angiographic images to be displayed continuously in real time. This allows for dynamic radiographic imaging, which is important for examining the dynamic flow of contrast through vascular lesions, collateral circulation, or normal cerebral circulation. Fluoroscopy is now performed at relatively low radiation doses because of better filtering and detection, which requires fewer X-rays to produce a high-quality image.2 When image intensifiers are used, this low dose can result in high levels of image mottling (also known as quantum mottle or noise), which limits the ability to detect subtle and low-contrast lesions. However, modern fluoroscopy utilizes digital radiographic receptors, which have a much wider exposure range, thereby significantly reducing the amount of noise and increasing the ability to detect low levels of contrast. Digital fluoroscopic imaging also permits various forms of image overlay and subtraction, so that roadmapping strategies for catheterizing difficult vessels and progressive coil embolization monitoring can be performed (Fig. 5.3).
Fig. 5.3 Roadmap navigation. Images are acquired at the desired viewing angles. The microcatheter can be seen in the insert image. This image is then reversed and over-layed onto an active image, thus allowing the visualization of any radiopaque structure, such as a wire. The angio table must not be moved; otherwise, the images become offset, and either the roadmap has to be reset or the table must be placed back into the identical position.
Digital Subtraction Angiography (DSA)
In digital subtraction angiography (DSA), a digital image (or mask) of the native image (no contrast) is subtracted from subsequent images with contrast administration to show only the opacified structures (Fig. 5.4).2 DSA is very sensitive to artifacts created by patient motion, which can be corrected with re-masking or “pixel-shifting.” Most modern angiography systems use charge-coupled device (CCD) cameras, which record the images in digital format. If conventional TV cameras are used along with image intensifiers, the images for digital subtraction must first be digitized. An important property of DSA images is their ability to undergo post-processing, which may include changing windowing levels, filtering, or applying digital tools to measure distances and densities quantitatively. Other advantages of digital imaging include speed of acquisition, instant transfer to viewing stations, and easy archiving options.
Radiation Safety (Tables 5.1 and 5.2)
Now that we understand how X-rays are generated and what equipment is used to capture them, we must now focus on the negative effects of radiation exposure and ways to minimize both patient and operator exposure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree