Chapter 102 Radiation Therapy and Radiosurgery in the Management of Craniopharyngiomas
Craniopharyngiomas are benign extra-axial epithelial tumors that arise from squamous epithelial remnants of Rathke’s pouch, near the pituitary gland.1 These cells may extend from the nasopharynx to the tuber cinereum and may arise within the sphenoid bone, the sella, or the suprasellar region. Although craniopharyngiomas are rare, they are the most common suprasellar tumor in the pediatric age group, accounting for as many as 5% of all intracranial tumors or up to 10% of pediatric brain tumors.2 Its incidence has been estimated to be about 1.5 per million persons per year,3,4 but may be considerably higher in specific ethnic groups, such as Japanese children (5.25 per million).5 Craniopharyngiomas have a bimodal age distribution, generally appearing in young patients between the ages of 5 and 14 years and in adults between 50 and 74 years.
Despite being histologically benign, craniopharyngiomas can cause severe and often permanent damage to nearby hypothalamic, visual, and endocrine apparatus. The presentation of these tumors may include symptoms related to endocrine derangement of the hypothalamic–pituitary axis, with severity dependent upon location, size, and rate of growth. Mass effect from the tumor may result in increased intracranial pressure presenting as headache, nausea, and vomiting. Cases with larger mass lesions may also present with hydrocephalus (seen more commonly in children than in adults), as a result of the obstruction of the cerebral aqueduct or the interventricular foramina.6,7 Compression of the nearby optic apparatus typically results in visual field defects, such as chiasmal syndrome and papilledema. Endocrine disruption often manifest as amenorrhea, hypothyroidism, and diabetes insipidus.8,9
Current treatment strategies include cystic drainage, intracavity chemotherapy, limited or gross total resection, and radiation therapy. These strategies are often combined in a patient-specific treatment plan based on age at presentation, tumor size, relation to optic chiasm and third ventricle, presence of hydrocephalus, and degree of pituitary endocrinopathy. If total excision can be safely performed with minimal risk to these structures, then surgery remains the treatment of choice as this allows rapid decompression, minimizes recurrence, and provides a histologic diagnosis. However, judgment of minimal risk is often unclear as some favor subtotal resection coupled with adjunctive therapy to achieve similar outcomes.10–18 Although surgical approaches are often curative, they harbor high treatment-related morbidity and mortality due to the close proximity of crucial neurovascular structures. Recurrent craniopharyngiomas must be considered separately, as secondary surgery is associated with higher risk of complications and a lower cure rate.16,19–23 More recently, stereotactic radiosurgery techniques have become increasingly utilized as either a primary or secondary treatment for craniopharyngioma patients.
Surgical Outcomes
Complete surgical resection is a primary objective and has curative potential. In a recent series by Shi et al., 284 patients (58 children) were treated surgically, without adjunctive therapy, between 1996 and 2006. Total, subtotal, and partial removal of the tumors were achieved in 237 (83.5%), 34 (12.0%), and 13 (4.5%) patients, respectively.24,25 Upon follow-up, 23 (14.1%) patients experienced recurrence 1 to 3.5 years after total resection, and 24 (64.9%) recurred after 0.25 to 1.5 years after subtotal or partial resection. In this series, the early mortality rate was 4.2%. In another 25-year retrospective study by Van Effenterre and Boch, 122 patients underwent gross total (59%), subtotal (29%), or partial (12%) surgical resection. During the follow-up period, 29 patients (24%) experienced one or more recurrences. The delay to recurrence was 1 to 180 months (mean 42 months, median 12 months). Patients that underwent total, subtotal, or partial removal experienced 13%, 33%, and 69% recurrence, respectively. Radiotherapy was reserved only for cases of recurrence. The surgical mortality rate was 2.5% and overall survival was 95% at two years, 91% at 5 years, and 83% at 10 years.26
The comparison of surgical complications across various series produces a variable picture. Most of the recent large series report a total resection rate of 59% to 90%.16,26–28 The 10-year recurrence-free survival rates have been reported as 74% to 81% for gross total resection,23,29,30 41% to 42% after partial removal,31,32 and 83% to 90% after combined surgery and radiotherapy.18,42 Surgical mortality rates vary between 1.1% and 4.2%.16,26,28,33 It is well documented that recurrent tumors are associated with significantly higher risk and poorer outcome, with overall mortality rates reported between 10.5% to 40.6%.16, 28 Pituitary dysfunction may occur in 50% to 100% of patients, the most common being diabetes insipidus. Visual deterioration may occur in up to 50% of patients undergoing gross total resection.34
Radiation Therapy for Craniopharyngiomas
Endocavitary Radiation Therapy
Endocavitary/intracavitary irradiation with a beta-emitter (186Re, 32P, 198Au, 90Y) or an antitumoral antibiotic (bleomycin) can be used to treat purely cystic or cystic components of craniopharyngiomas.35 This treatment modality requires the use of stereotactic technique to achieve intracystic instillation of radioactive agents. In a recent retrospective study of endocavitary irradiation (186Re) treatment by Derrey et al., of 48 patients treated, complete cystic resolution was achieved in 17 patients (44%) and partial resolution in another 17 patients (44%). Visual function improved in 12 patients, while baseline endocrine function was preserved.35 Similarly, Julow and colleagues observed an 80% reduction in 47 patients and complete disappearance of cyst in 27 patients within 1 year after treatment with intracystic colloidal yttrium-90.36 Across several studies, the response rate of tumors to endocavitary/intracavitary irradiation is 71% to 88%.37,38 However, because intracavitary irradiation is limited to cystic tumors, recurrence, and survival rates with this type of therapy alone are considered inferior to surgery or external radiotherapy.24,38 Additionally, the risk of visual deterioration is considerable, possibly due to unpredictable radiation dose to the optic pathway and radiation damage from leakage. In a review by Caceres, no change or improvement in visual acuity after intra-cavitary irradiation ranged from 42% to 99% while 31% to 58% experienced deterioration in visual function.39
External Beam Radiation Therapy
Fractionated radiation therapy improves craniopharyngioma control and survival32,40–44 and is the standard treatment for residual or recurrent tumor. Most series demonstrate that when combined with subtotal resection, adjuvant radiotherapy allows for greater tumor control and survival than surgery alone.31, 45–49 In a study by Varlotto et al.,49 an 89% tumor control rate was seen in patients who received both subtotal resection and external beam irradiation.39 Stripp and colleagues48 compared 57 patients treated only with surgery to 18 treated with subtotal resection combined with radiation therapy, demonstrating a 10-year tumor control rate of 42% and 84%, respectively. The case for primary radiation therapy for recurrent craniopharyngioma is even stronger for lower risk and better outcome (30% vs. 90% 10-year progression-free survival).12,50–52 Finally, Karavitaki and colleagues examined the records of 121 patients and subdivided the patients into four treatment categories: gross total removal, gross total removal with radiotherapy, partial removal, and partial removal with radiotherapy. The recurrence-free survival rate was 100% at 10 years in the gross total removal and gross total removal with radiotherapy groups, 38% in the partial removal group, and 77% in the partial removal with radiotherapy group.34
With radiotherapy, the risk of neurotoxicity from radiation injury should be considered alongside gains in potential tumor control. Conventionally fractionated focal radiation therapy around the sellar–suprasellar region is also associated with risks similar to surgery. Disruption of the hypothalamic-pituitary axis (30% to 70%) may result in diabetes insipidus, panhypopituitarism, hypogonadism, hypothalamic obesity, or sleep disturbance.53–55 The normal optic apparatus is particularly sensitive to radiation, and optimized dose and fractionation regimes carry a 3% risk of optic neuropathy.56–58 There is also considerable discussion about the effect of radiation on cognitive function, an issue particularly pertinent in the pediatric population. Additionally, radiation itself carries the risk of secondary malignancies,59–61 radiation necrosis,61,62 and vasculopathy, which also have end-neurodegenerative effects.
Typically, craniopharyngiomas are treated with doses between 45 and 60 Gy in 1.8- to 2-Gy fractions to prevent growth of tumor and minimize injury to the visual pathways. Long-term (10 years) local control ranges from 31% to 42% with surgery alone compared with 57% to 89% with surgery and radiotherapy.31,32,45,47–49 However, there are limitations as the wide treatment field includes irradiating many structures, such as the optic apparatus, pituitary gland, hypothalamus, and medial temporal lobe. The risk may only manifest itself after a long delay, but this is particularly important since benign conditions such as craniopharyngiomas confer favorable long-term survival and its predilection for the pediatric population. Another limitation is when conventional radiotherapy fails, it almost inevitably precludes further radiotherapy treatment to the recurrent tumor. Finally, although of minor importance, conventional fractionated radiotherapy usually takes place over a 6-week course, which is less attractive to patients when compared to other shorter treatment courses. For these reasons, radiosurgery (particularly multisession radiosurgery) may present a more amenable option, especially to tumors surrounding the optic apparatus.
Stereotactic Radiosurgery
Stereotactic radiosurgery (SRS) is a relatively recent therapeutic option that has significantly improved the effectiveness of and morbidity associated with radiation therapy. With SRS, one to five sessions of radiation are utilized to treat residual or recurrent lesions. The application of stereotaxis for target localization, treatment planning, and daily treatment immobilization allows for a more precise delivery of radiation dose with a steeper dose gradient between tumor and parenchymal tissue to prevent further neurologic deficit. The irradiation dose can be delivered using either a multiple cobalt-60, gamma radiation-emitting source such as a gamma knife (GK) or a modified linear accelerator (LINAC, CyberKnife). Most stereotactic systems can deliver a radiation beam with no more than approximately 1 mm of error. Historically, SRS for craniopharyngiomas was limited to tumors 3 cm or less that are 3 to 5 mm away from the optic chiasm and nerves. In the case of single-session radiosurgery, the optic chiasm becomes a limiting anatomic structure capable of only receiving 8 to 10 Gy per session before the incidence of optic neuropathy increases.63,64 More recent multisession radiosurgery using image-guided radiosurgical techniques has allowed for treatment of craniopharyngiomas immediately adjacent to the anterior visual pathways.65
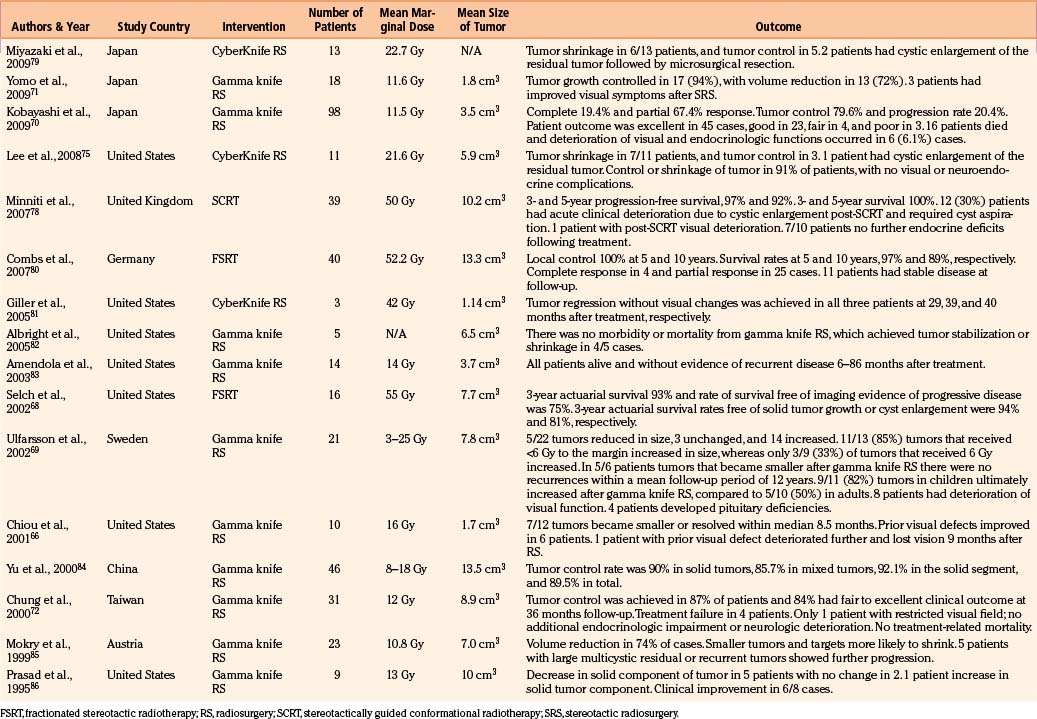
In the current literature, several studies have reported safe and effective long-term results with the application of SRS using a GK for the treatment of craniopharyngiomas.66–69 Kobayashi et al. published the largest treatment and outcomes series with 98 cases. At a mean marginal dose of 11.5 Gy and a mean tumor size of 3.5 cm3, Kobayashi and colleagues observed a tumor control rate of 79.6%, with a complete response in 19.4% and partial response in 67.4% of the cases.70 The actuarial 5- and 10-year survival rates were 94.1% and 91% with respective progression-free survival rates of 60.8% and 53.8%. Yomo and colleagues demonstrated the outcomes of 18 patients with residual or recurrent craniopharyngioma who were treated by the Leksell Gamma Knife Model C. Tumor growth (mean tumor volume of 1.8 cm3 and a mean marginal irradiation dose of 11.6 Gy) was controlled in 17 cases (94%), and volume reduction was attained in 13 cases (72%).71 No new endocrinopathy was observed and 3 patients experienced substantial improvement of visual functions following shrinkage of the neoplasm. In another study by Chung et al., tumor control was achieved in 87% of the 31 patients and 84% had fair to excellent clinical outcome.72 Finally, Minniti et al. completed a meta-analysis of eight published studies that includes 252 patients who underwent either unfractionated radiosurgery or GK therapy, demonstrating a tumor control rate of 69%. Taken together (Table 102-1), the published studies on GK therapy for craniopharyngiomas demonstrate an average control rate of 90% for solid tumors, 88% for cystic tumors, and 60% for mixed tumors.73 Tumor control was achieved with a mean marginal dose of 12 Gy and recurrence of tumor was observed in 85% of cases that received a marginal dose of less than 6 Gy.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree