29 Radiculopathy
Clinical
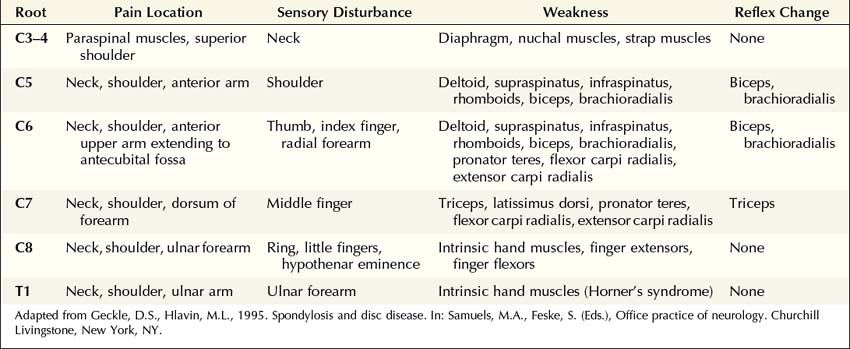
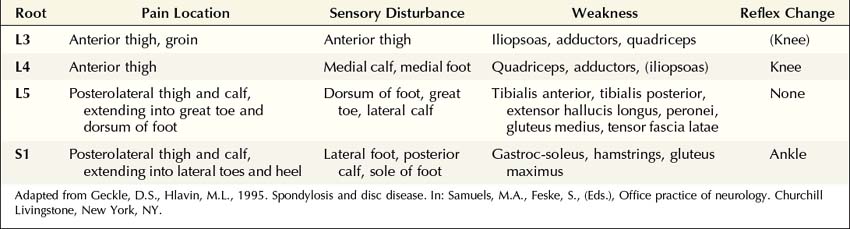
The clinical hallmark of radiculopathy includes pain and paresthesias radiating in the distribution of a nerve root, often associated with sensory loss and paraspinal muscle spasm. Motor dysfunction may also be present. Radiculopathy caused by degenerative bone and disc disease most often affects the cervical (C3–C8) and lower lumbosacral (L3–S1) segments, resulting in well-recognized clinical syndromes (Tables 29–1 and 29–2). Associated paraspinal muscle spasm commonly limits the range of motion, and movement of the neck or back may exacerbate symptoms.
The particular sensory and motor symptoms associated with a radiculopathy depend on which nerve root or roots are involved. Each nerve root supplies cutaneous sensation to a specific area of skin, known as a dermatome (Figures 29–1 and 29–2), and motor innervation to certain muscles, known as a myotome (Tables 29–3 and 29–4). Each dermatome overlaps widely with adjacent dermatomes. Consequently, it is very unusual for a patient with an isolated radiculopathy to develop a severe or dense sensory disturbance. Dense numbness usually is more indicative of a peripheral nerve lesion than a radiculopathy. In a patient with radiculopathy, sensory loss more often is vague, poorly defined, or absent, despite the presence of paresthesias.
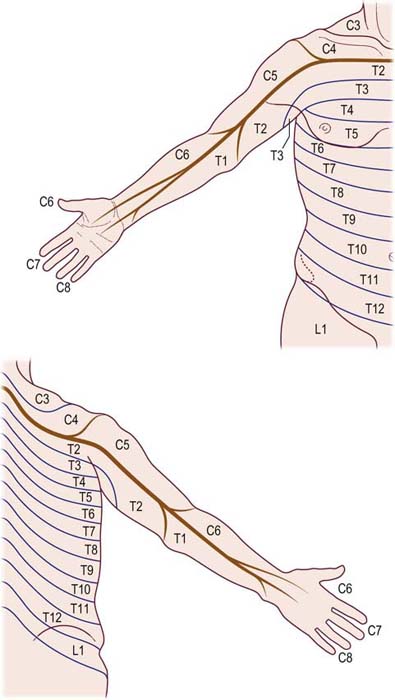
FIGURE 29–1 Cervical and thoracic dermatomes.
(From Aids to the examination of the peripheral nervous system. London: Baillière Tindall. With permission, 1986.)
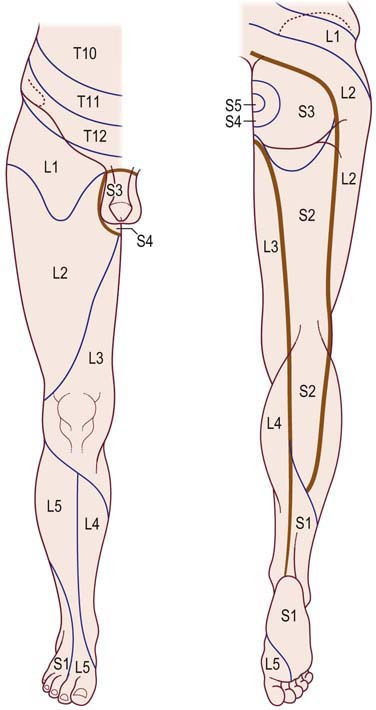
FIGURE 29–2 Lower thoracic and lumbosacral dermatomes.
(From Aids to the examination of the peripheral nervous system. London: Baillière Tindall. With permission, 1986.)
Table 29–3 Root Innervation of Major Upper Extremity Muscles
| Root | Muscle | Nerve |
|---|---|---|
| C4 5 | Rhomboids | Dorsal scapular |
| C5 6 | Supraspinatus | Suprascapular |
| C5 6 | Infraspinatus | Suprascapular |
| C5 6 | Deltoid | Axillary |
| C5 6 | Biceps brachii | Musculocutaneous |
| C5 6 | Brachioradialis | Radial |
| C5 6 7 | Serratus anterior | Long thoracic |
| C5 6 7 | Pectoralis major: Clavicular | Lateral pectoral |
| C6 7 8 T1 | Pectoralis major: Sternal | Medial pectoral |
| C6 7 | Flexor carpi radialis | Median |
| C6 7 | Pronator teres | Median |
| C6 7 | Extensor carpi radialis longus | Radial |
| C6 7 8 | Latissimus dorsi | Thoracodorsal |
| C6 7 8 | Triceps brachii | Radial |
| C6 7 8 | Anconeus | Radial |
| C7 8 | Extensor digitorum communis | Radial |
| C7 8 | Flexor digitorum sublimis | Median |
| C7 8 | Extensor indicis proprius | Radial |
| C7 8 | Extensor carpi ulnaris | Radial |
| C7 8 T1 | Flexor pollicis longus | Median |
| C7 8 T1 | Flexor digitorum profundus | Median/Ulnar |
| C8 T1 | Flexor carpi ulnaris* | Ulnar |
| C8 T1 | First dorsal interosseus | Ulnar |
| C8 T1 | Abductor digiti minimi | Ulnar |
| C8 T1 | Abductor pollicis brevis | Median |
Note: Underlining indicates predominant root innervation.
* In some individuals, the flexor carpi ulnaris may have a C7 contribution.
Table 29–4 Root Innervation of Major Lower Extremity Muscles
| Root | Muscle | Nerve |
|---|---|---|
| L2 3 4 | Iliacus | Femoral |
| L2 3 4 | Rectus femoris | Femoral |
| L2 3 4 | Vastus lateralis and medialis | Femoral |
| L2 3 4 | Adductors | Obturator |
| L4 5 | Tibialis anterior | Deep peroneal |
| L4 5 | Extensor digitorum longus | Deep peroneal |
| L4 5 S1 | Extensor hallucis longus | Deep peroneal |
| L4 5 S1 | Extensor digitorum brevis | Deep peroneal |
| L4 5 S1 | Medial hamstrings | Sciatic |
| L4 5 S1 | Gluteus medius | Superior gluteal |
| L4 5 S1 | Tensor fascia latae | Superior gluteal |
| L5 S1 | Tibialis posterior | Tibial |
| L5 S1 | Flexor digitorum longus | Tibial |
| L5 S1 | Peronei | Superficial peroneal |
| L5 S1 | Lateral hamstrings (biceps femoris) | Sciatic |
| L5 S1 2 | Gastrocnemius – lateral | Tibial |
| L5 S1 2 | Gluteus maximus | Inferior gluteal |
| L5 S1 2 | Abductor hallucis brevis | Tibial–medial plantar |
| S1 2 | Abductor digiti quinti pedis | Tibial–lateral plantar |
| S1 2 | Gastrocnemius – medial | Tibial |
| S1 2 | Soleus | Tibial |
Note: Underlining indicates predominant root innervation.
Electrophysiologic Evaluation
Nerve Conduction Studies
In patients with radiculopathy, nerve conduction studies typically are normal, and the electrodiagnosis is established with needle EMG (Box 29–1). Although some motor abnormalities are occasionally seen in radiculopathy, the more important reason to perform nerve conduction studies is to exclude other conditions that may mimic radiculopathy, especially entrapment neuropathy and plexopathy. In cases of upper extremity lesions, ulnar neuropathy at the elbow and CTS must be excluded. Ulnar neuropathy and C8 radiculopathy both can present with pain in the arm associated with numbness of the little and ring fingers. Likewise, pain in the arm with paresthesias involving the thumb, index, and middle fingers may be seen in C6–C7 radiculopathy and CTS. In the case of lower extremity symptoms, one must exclude peroneal neuropathy at the fibular neck. Both peroneal palsy and L5 radiculopathy may present with pain in the leg, accompanied by footdrop and paresthesias over the dorsum of the foot and lateral calf. In more severe cases, the clinical differentiation between a radiculopathy and a common entrapment usually is straightforward. In mild or early cases, however, the distinction often is more difficult, and nerve conduction studies are useful to either demonstrate or exclude an entrapment neuropathy.
Box 29–1
Recommended Nerve Conduction Study Protocol for Radiculopathy
Upper Extremity
• Perform median and ulnar motor conduction studies, recording abductor pollicis brevis and abductor digiti minimi, respectively. Be sure to exclude carpal tunnel syndrome in suspected C6–C7 radiculopathy and ulnar neuropathy at the elbow in suspected C8 radiculopathy. Ideally, studies should be performed bilaterally if CMAP distal latency, amplitude, or conduction velocity is abnormal or borderline.
• Perform at least one sensory study, ideally in the distribution of the suspected radiculopathy (see Table 29–6). It is best to perform the sensory studies bilaterally if the amplitude on the symptomatic side is low or borderline.
• In suspected C6–C7 radiculopathy (paresthesias into thumb, index, and middle fingers), perform at least one median versus ulnar internal comparison study (e.g., median versus ulnar palm-to-wrist mixed studies), as a sensitive internal control, to definitely exclude electrophysiologic evidence of median neuropathy across the wrist.
Lower extremity
• Perform peroneal and tibial motor conduction studies, recording extensor digitorum brevis and abductor hallucis brevis, respectively. Be sure to exclude peroneal palsy at the fibular neck, especially in suspected L5 radiculopathy. Ideally, studies should be performed bilaterally if CMAP distal latency, amplitude or conduction velocity is abnormal or borderline.
• Perform at least one sensory study, ideally in the distribution of the suspected radiculopathy (see Table 29–6). It is best to perform these studies bilaterally if the amplitude on the symptomatic side is low or borderline.
• Perform tibial and peroneal F responses. It is best to perform these studies bilaterally if the results are abnormal or borderline on the symptomatic side.
• Perform H reflexes to soleus bilaterally, especially when considering S1 radiculopathy.
Sensory studies are the most important part of the nerve conduction studies in the assessment of radiculopathy. The sensory nerve action potential (SNAP) remains normal in lesions proximal to the dorsal root ganglion (Figure 29–3). Nearly all radiculopathies, including those caused by compression from herniated discs and spondylosis, damage the root proximal to the dorsal root ganglion (Figure 29–4). Conversely, lesions at or distal to the dorsal root ganglion result in decreased SNAP amplitudes if they are associated with axonal loss. Thus, lesions of the plexus and peripheral nerve (proximal and distal nerve) are associated with abnormal SNAPs, whereas lesions of the nerve root result in normal SNAPs.
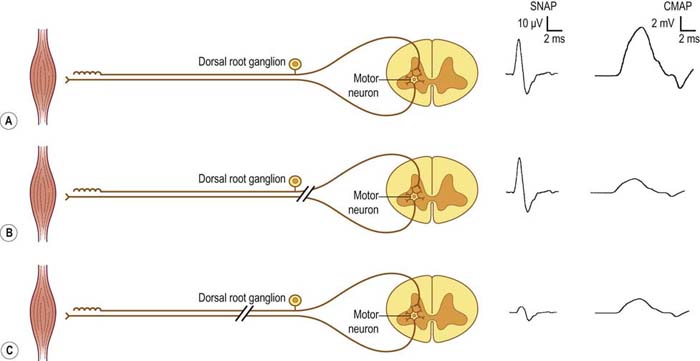
FIGURE 29–3 Sensory and motor potentials in axonal loss lesions distal and proximal to the dorsal root ganglion.
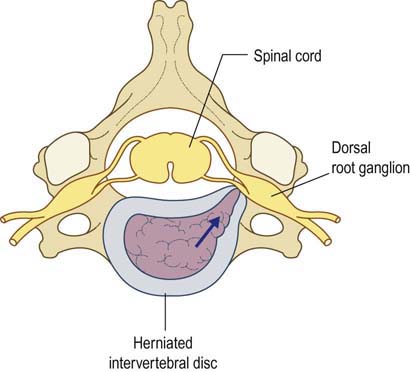
FIGURE 29–4 Radiculopathy and sparing of the dorsal root ganglion.
(From Wilbourn, A.J., 1993 Radiculopathies. In: Brown, W.F., Bolton, C.F. (Eds.), Clinical electromyography, 2nd ed. Butterworth, Boston. With permission.)
It is always imperative to check the SNAP that is in the distribution of the sensory symptoms (Table 29–5). For instance, if a patient has pain down the arm with tingling and paresthesias of the middle finger, the median sensory response to the middle finger should be checked. In such a case, if the lesion is at or distal to the dorsal root ganglion (e.g., in the brachial plexus or median nerve) and there is axonal loss, the SNAP amplitude will be abnormal, if enough time has passed that wallerian degeneration has taken place. On the other hand, if the lesion is proximal to the dorsal root ganglion (e.g., C7 radiculopathy), the SNAP amplitude will be normal. The presence of a normal SNAP yields important diagnostic information. A normal SNAP in the same distribution as sensory symptoms and signs should always suggest a lesion proximal to the dorsal root ganglion (although a proximal demyelinating or acute peripheral nerve lesion also can result in a normal SNAP). One important rare exception to his rule is discussed below.
Table 29–5 Sensory Potentials to Check in Radiculopathy
| SNAP | Root |
|---|---|
| Lateral antebrachial cutaneous | C5–C6 |
| Radial to the thumb | C6 |
| Median to the thumb | C6 |
| Radial to the snuffbox | C6–C7 |
| Median to the index finger | C6–C7 |
| Median to the middle finger | C7 |
| Median to the ring finger | C7–C8 |
| Ulnar to the ring finger | C7–C8 |
| Ulnar to the little finger | C8 |
| Dorsal ulnar cutaneous | C8 |
| Medial antebrachial cutaneous | T1 |
| Saphenous | L4 |
| Superficial peroneal sensory | L5 |
| Sural | S1 |
SNAP, sensory nerve action potential.
Note: SNAPs are normal in lesions proximal to the dorsal root ganglion, including lesions resulting in radiculopathies. When evaluating a possible radiculopathy, one should examine at least one SNAP in the distribution of the suspected radiculopathy. For example, the ulnar SNAP to the little finger should be normal in a C8 radiculopathy. If it is abnormal, the lesion likely is not at the root, unless there is another reason for the SNAP to be abnormal, such as a superimposed ulnar neuropathy at the elbow.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree