Rheumatoid Arthritis: Upper Cervical Spine
Dieter Grob
Takachika Shimizu
In spite of many years of research and treatment of rheumatoid arthritis (RA), there remains a relative inability to accurately predict the natural course of both RA (1) and rheumatoid cervical involvement (2).
In order to build up a strategic concept, a long-term follow-up is always necessary to evaluate the efficacy of the treatment. However, because of the dynamic changes associated with RA medications, there may be an undulating course following surgery. This may make the analysis of surgical results more complicated and reminds us to assess results from the literature with caution. According to Boyle (3) and Nakano (4), one-third to one-half of the patients, after serologic confirmation of the diagnosis, present with some degree of atlantoaxial subluxation, but only a few of them will eventually become myelopathic. The statistics do not yet take into account the change in medical treatment of the disease with new medications. Apparently, the frequency and severity of the aggressiveness of surgical treatment have been significantly reduced in recent years. However, surgery of the cervical spine for RA will always be a mainstay.
This chapter outlines the pathologic changes that may occur at the craniocervical junction in order to correlate them with symptoms and signs and to outline the indications for and types of operative intervention. It also reviews outcome criteria and the complications of treatment.
PATHOLOGY
The pathologic process of RA begins as an inflammatory synovitis, which in turn causes articular cartilage damage, subchondral damage with disorganization of the joint, damage to the capsule, and resultant strain on the associated ligaments. The inflammatory process also involves the ligaments, and the combined stresses result in tears and ruptures. Drugs, age, and instability combine to produce osteopenia, but in affected patients, there is no evidence of avascular necrosis or vasculitis.
Atlantoaxial instability may in fact be caused by damage to the ligamentous apparatus, the odontoid process (dens), or both. Damage to the transversal atlantal ligament alone causes as much as 4 to 5 mm of subluxation. A greater anterior atlantodental interval (AADI) in flexion films implies damage to the atlanto-occipital ligament complex or an incomplete or resorbed odontoid process (Fig. 61.1A,B). Vertical translocation (cranial settling) results from progressive destruction of the atlantoaxial and atlanto-occipital lateral masses and the lateral masses of the subaxial cervical spine.
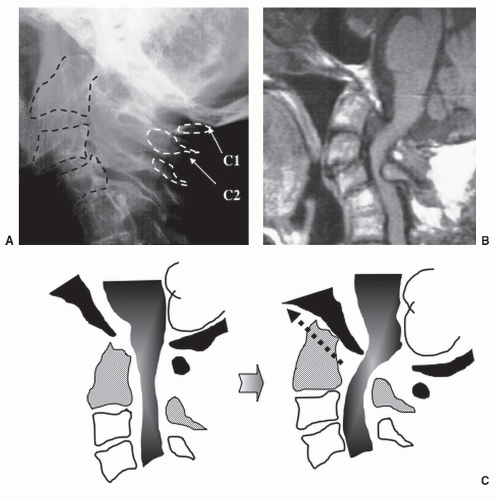
If the translocation continues, the atlantoaxial joints may lock and the impacted odontoid will eventually appear to be in a fixed in position (Fig. 61.2). This lends credence to the mistaken clinical impression that the joint that once had an increased AADI is now not involved because there is no longer evident movement. Translocation of more than 1 cm is usually associated with rupture of the ring of the atlas. Coupled with these changes is translation with the atlas moving forward. This dislocation causes compression on the dorsal aspect of the spinal cord, creating pincer, with the dens compromising the subarachnoidal space and the spinal cord ventrally. Dorsal dislocation occurs only in cases with dens destruction (Fig. 61.3A-C). Its prevalence in the literature is reported to be no more than 6.7% of all atlantoaxial dislocations (5). Each flare-up of the inflammatory process will cause an acute synovitis. The resulting pannus further compromises the spinal cord. Immobilization by operative stabilization results in resolution (6). Only in the presence of severe myelopathy should direct ventral decompression be considered.
Neuropathologic and neuroradiologic studies demonstrate the possible mechanism causing myelopathy (7,8). The spinal cord is thin and atrophic. In the white matter tracts, there are axonal retraction balls, the end result of torn axons. In the anterior horn cells, chromatolysis is often found. These findings are characteristic of repetitive trauma, as the cord is impacted at the level of the foramen magnum due to vertical migration or the atlantoaxial segment due to atlantoaxial instability.
CLINICAL FINDINGS
Most patients with RA of the cervical spine have neck pain. C2 nerve root pain or localized pain behind the auricle suggests pain arising from the atlantoaxial segment. Pain
originating from the atlanto-occipital joint has nonspecific referral pattern and varies significantly. In the presence of subaxial changes, diagnostic intra-articular injections might be useful to identify the origin of the pain (9). In some instances, atlantoaxial instability and joint crepitation may be felt on palpation of the C1/C2 segment during passive flexion and extension. The so-called clunk phenomenon may be associated with a positive Lhermitte sign during flexion of the head. Finally, it should be kept in mind that the neck pain in RA patients might not be predominant and is often disguised by other more obvious manifestations of the disease (10).
originating from the atlanto-occipital joint has nonspecific referral pattern and varies significantly. In the presence of subaxial changes, diagnostic intra-articular injections might be useful to identify the origin of the pain (9). In some instances, atlantoaxial instability and joint crepitation may be felt on palpation of the C1/C2 segment during passive flexion and extension. The so-called clunk phenomenon may be associated with a positive Lhermitte sign during flexion of the head. Finally, it should be kept in mind that the neck pain in RA patients might not be predominant and is often disguised by other more obvious manifestations of the disease (10).
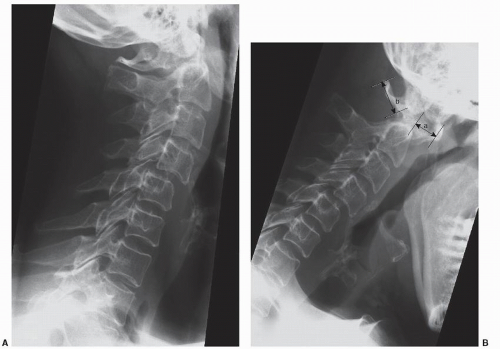 Figure 61.1. Extension (A) and flexion (B) radiographs of the upper cervical spine in RA. The changes between the two positions demonstrate mobile subluxation of C1/C2 (a, AADI; b, PADI). |
Cranial nerve palsies are extremely uncommon (11). Nevertheless, when corresponding symptoms are present, the patient might be on a life-threatening course. Downbeat nystagmus is an ominous sign of moderate to severe damage of the brainstem or high cervical spinal cord. The absence of a gag reflex may predict a high risk of postoperative aspiration pneumonia (12, 13, 14, 15, 16, 17 and 18). For the anesthetist, the pathoanatomical changes with instability, ankylosis, and soft tissue swelling represent a significant challenge for intubation and postoperative management (19). Specific neurologic signs, such as nystagmus, may be due to a coincidental Chiari malformation. Loss of position sense is evident when the spinal cord is compressed dorsally.
Typical signs of spinal cord compression are infrequent. Instead, patients report decreasing ambulation and dexterity, stiffness, and, occasionally, altered sensation. Care has to be taken to differentiate the consequences of joint destruction, prior surgery, and true neurologic symptoms. The scapulohumeral reflex (20) is a useful tool to detect upper motor neuron dysfunction of high cervical lesion even in RA patients. With this reflex testing, muscle activity of trapezius, which is innervated by the accessory nerve, is easily observed though the movement of scapula because scapula is floating on the rib cage. This may be present, even in patients with severe shoulder pathology.
CLINICAL ASSESSMENT
As with any progressive multisystem disease, the characterization of the extent of the condition and the effects of treatment must be standardized if there is to be any objective assessment of one’s center’s treatment effectiveness. A formal neurologic examination is not particularly useful due to multiple and individual anatomical changes and also the dynamic course of the disease. Different methods to assess function rather than neurologic deficits were used to overcome these difficulties (21,22). The Ranawat classification scheme (23), however, remained the internationally most widely used classification scheme. A more detailed subdivision of this group has been proposed (24,25) (Table 61.1). According to the latter modified Ranawat classification, results of surgery for the IIIBb patients with mutilating disease improved to IIIBa following occipitothoracic stabilization and fusion (10).
RADIOLOGY
Conventional anteroposterior and lateral radiographs remain the basis of radiologic investigations. The transoral radiographic view (“open-mouth view”) visualizes the atlantoaxial joints. However, in RA it is often impossible to obtain such because the patients cannot be positioned
correctly. Bone structure, posture and alignment, and calcifications should be examined. The degree of horizontal atlantoaxial subluxation and the upward migration of the dens may be detected and measured in the lateral view (26,27). Functional lateral radiographs in flexion and extension not only allow one to detect instabilities in the atlantoaxial segment and the subaxial spine but also provide information about the reducibility of the subluxation. (Fig. 61.1) Measurement of the posterior atlantodental interval (PADI) appears to be more accurate than the conventional AADI (28) since it indicates the true bony space available for the spinal cord. For an assessment of additional encroachment by pannus tissue, a magnetic resonance imaging (MRI) investigation is required (29). According to a recent multicenter study (30), 14 mm or less of space available for the spinal cord in lateral radiographs at C1 level (=PADI) was recommended as a cutoff point for the purpose to screen the patients with high risk for myelopathy.
correctly. Bone structure, posture and alignment, and calcifications should be examined. The degree of horizontal atlantoaxial subluxation and the upward migration of the dens may be detected and measured in the lateral view (26,27). Functional lateral radiographs in flexion and extension not only allow one to detect instabilities in the atlantoaxial segment and the subaxial spine but also provide information about the reducibility of the subluxation. (Fig. 61.1) Measurement of the posterior atlantodental interval (PADI) appears to be more accurate than the conventional AADI (28) since it indicates the true bony space available for the spinal cord. For an assessment of additional encroachment by pannus tissue, a magnetic resonance imaging (MRI) investigation is required (29). According to a recent multicenter study (30), 14 mm or less of space available for the spinal cord in lateral radiographs at C1 level (=PADI) was recommended as a cutoff point for the purpose to screen the patients with high risk for myelopathy.
TABLE 61.1 Modificed Ranawat Classification | |||||
|---|---|---|---|---|---|
|
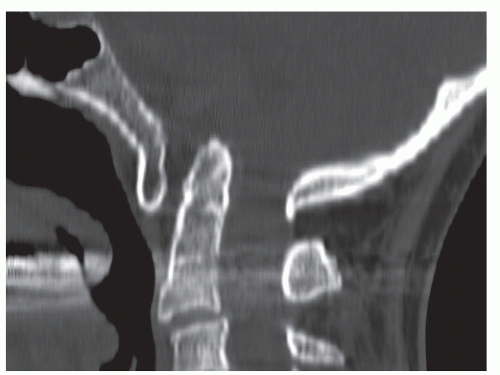 Figure 61.4. Due to the resorption of the lateral masses of the atlas, an upward migration of the odontoid occurs. It enters the foramen magnum with consecutive compression of the brainstem. |
In the majority of vertical instability cases at craniovertebral junction, the odontoid migrates upward into the foramen magnum (Fig. 61.4). But in rare cases with a long history of mutilating RA, the odontoid migrates upward and out of the foramen magnum (Fig. 61.3) (31,32). This atypical vertical instability was reported as a life-threatening neurologic high-risk instability. The management strategy must be crafted by taking into account this problem. In the less dramatic cases, the degree of upward migration of the dens may be determined with the Redlund-Johnell method, measuring from the base of C2 to the McGregor’s line (33).
COMPUTED TOMOGRAPHY AND MAGNETIC RESONANCE IMAGING
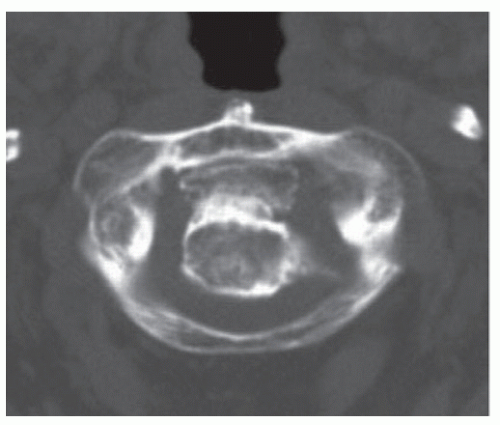
Computed tomography (CT) and MRI are indispensable in the diagnostic and surgical process. They can accurately locate bony (CT more than MRI) or soft tissue (MRI more than CT) compression or obstruction and allow precise interpretation of anatomical variations and consequently safe operative planning (Fig. 61.5). MRI in flexion and extension identifies by direct visualization the extent of compression of the retrodental inflammatory tissue in both positions and can provide information about the indication for ventral decompression. An absolute spinal cord diameter of less than 6 mm will leave the patient susceptible to myelopathy (29).
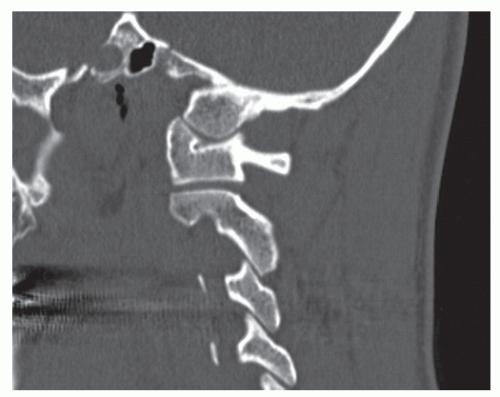 Figure 61.5. CT of the pars interarticularis of C2. Exact analysis allows to plan screw trajectory and to assess the suitability of the anatomy for the procedure. |
Several types of screws are placed to gain a stability also in rheumatoid cases (34, 35, 36 and 37). All have a potential risk to penetrate vertebral arteries, and preoperative examination of vertebral artery using MRI or CT angiogram has a significant role to prevent complications (38,39) (Fig. 61.6).
MANAGEMENT DECISIONS
Due to the individual course of the systemic disease, it is difficult to establish general rules for surgical management decisions; however, some broad principles are emerging (Tables 61.2 and 61.3)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree