11 Routine Lower Extremity Nerve Conduction Techniques
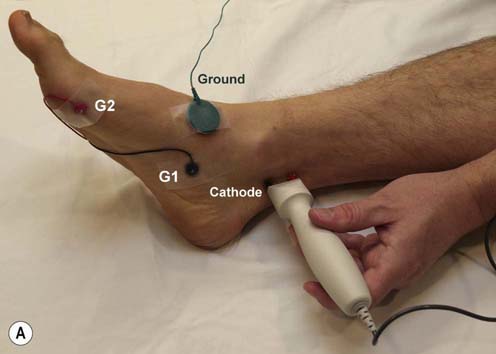
Tibial Motor Study (Figure 11–1)
Key Points:
• The tibial compound muscle action potential (CMAP) often has an initial positive deflection, indicating that G1 is not over the motor endplate. If this occurs, the position of G1 should be changed slightly.
• CMAP amplitude at the popliteal fossa stimulation site often is lower than at the medial ankle stimulation site (normal controls may drop up to 50%). Thus, caution must be used whenever interpreting a drop in amplitude between the ankle and popliteal fossa as a conduction block on tibial motor studies. Side-to-side comparisons often are useful in this situation.
• High stimulation intensities often are required at the popliteal fossa to ensure supramaximal stimulation.
• Recording also can be done to the flexor hallucis brevis (FHB) muscle.
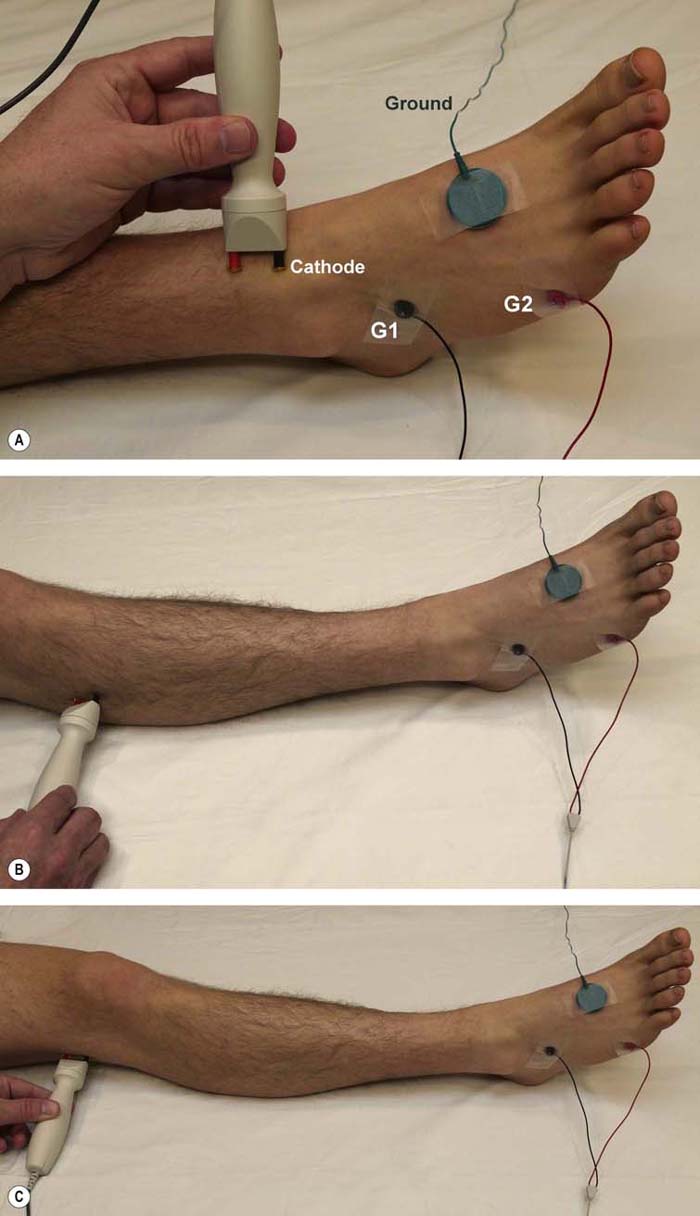
Peroneal Motor Study (Figure 11–2)
Stimulation Sites:
Ankle: Anterior ankle, slightly lateral to tibialis anterior tendon
Below fibular head: Lateral calf, one to two fingerbreadths inferior to fibular head (one can straddle the fibular neck with the stimulator)
Lateal popliteal fossa (above fibular neck): Lateral knee, adjacent to external hamstring tendons, at a distance of 10–12 cm from the below-fibular head site
Key Points:
• Higher stimulation currents are needed at the below-fibular head site because the nerve lies deep at that location.
• Always perform the ankle, below-fibular neck, and above-fibular neck stimulations. If only the ankle and above-fibular neck stimulations are done, one can miss peroneal slowing across the fibular neck.
• Avoid excessive stimulation at the lateral popliteal fossa site to prevent co-stimulation of the tibial nerve.
• If there is a higher CMAP amplitude at the below-fibular head and popliteal fossa sites than at the ankle, consider an accessory peroneal nerve.
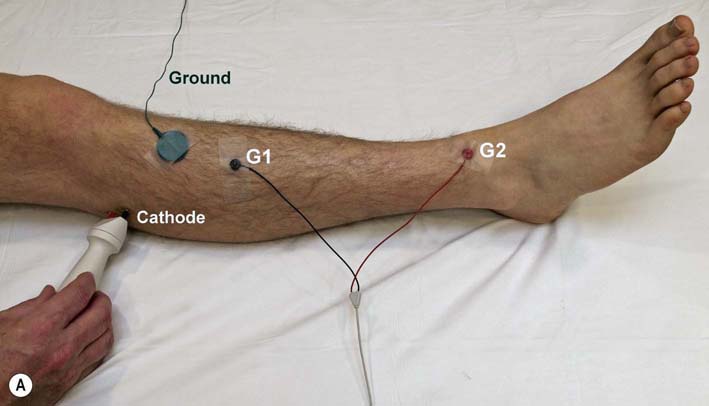
Peroneal Motor Study (Figure 11–3)
Key Points:
• Recording the TA is especially valuable in patients with suspected peroneal neuropathy at the fibular neck. Demonstrating a conduction block, focal slowing across the fibular neck or both may be easier when recording the TA than the EDB.
• Higher stimulation currents are needed at the below-fibular head site because the nerve lies deep at that location.
• Avoid excessive stimulation at the lateral popliteal fossa site to prevent co-stimulation of the tibial nerve.
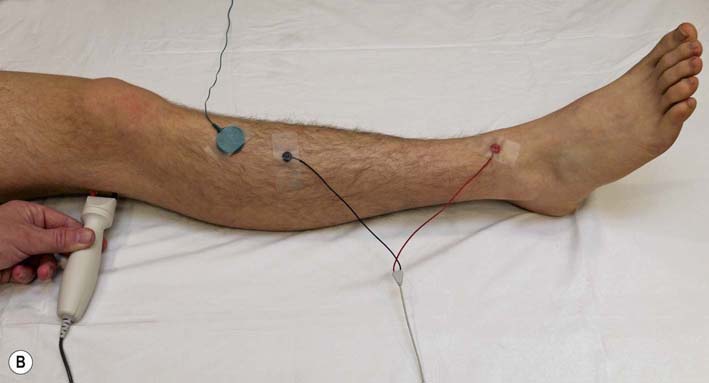
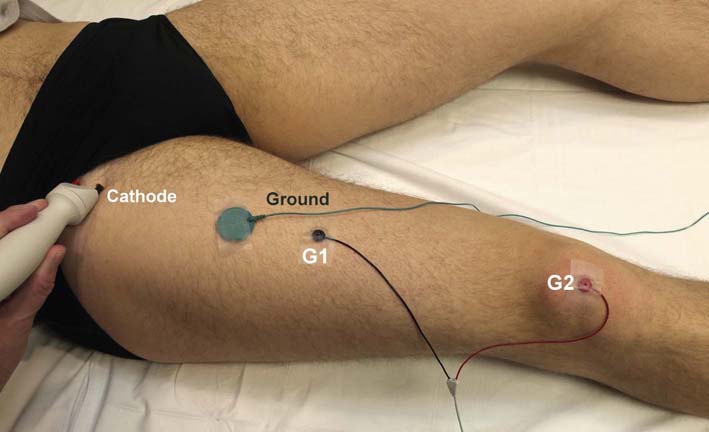
Femoral Motor Study (Figure 11–4)
Key Points:
• Firm pressure is needed when holding the stimulator.
• Difficult study to perform in obese individuals; high currents are typically needed (e.g., >50 mA).
• Limited indications; this study usually is used to compare motor amplitudes from side to side to quantitate the degree of axonal loss in femoral neuropathies, lumbar plexopathies, and severe L4 radiculopathies.
• Normal amplitude is >3 mV; however, side-to-side comparisons are most useful when symptoms are unilateral.
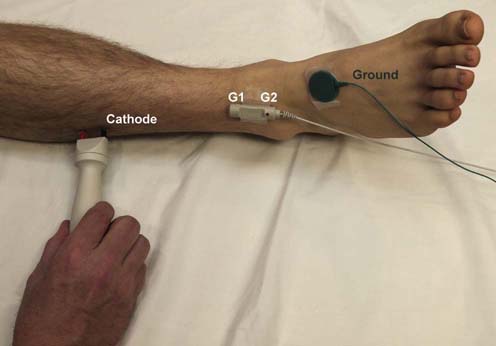
Superficial Peroneal Sensory Study (Figure 11–5)
Key Points:
• Although the normal value for peak latency is based on the standard distance of 14 cm, in many individuals, the nerve is much easier to stimulate at a shorter distance (typically 10–12 cm, and in some individuals as short as 7–9 cm). Supramaximal stimulation usually can be achieved with low stimulation intensities (e.g., 5–25 mA). Thus, if the response is not present stimulating at 14 cm or if high currents are needed, try a shorter distance of 10–12 cm, or 7–9 cm. If a good response is obtained at a shorter distance, do not use the peak latency to determine if the response is normal, but rather the calculated conduction velocity based on the onset latency and the distance used.
• May be abnormal in lesions of the peroneal nerve, sciatic nerve, or lumbosacral plexus.
• To maximize the response, the recording electrodes may have to be repositioned either slightly medially or laterally to the original position.
• Side-to-side comparisons of amplitude and latency often are helpful.
• Antidromic study described; for orthodromic study, recording and stimulation sites are reversed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree