8 Schizophrenia and delusional (paranoid) disorders
Introduction
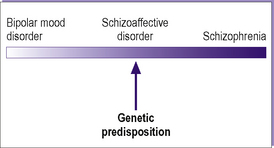
Schizophrenia is one of the most debilitating psychiatric disorders. It is a major psychosis that can manifest itself in a variety of ways, described below. This is followed by a discussion of less severe related psychotic disorders known as delusional or paranoid disorders. The chapter ends with a consideration of schizoaffective disorders, which combine elements of both schizophrenia and mood disorders (see Chapter 9). Table 8.1 gives the ICD-10 classification of these disorders.
Table 8.1 ICD-10 classification of schizophrenia and delusional disorders
| F20 Schizophrenia |
| F20.0 Paranoid schizophrenia |
| F20.1 Hebephrenic schizophrenia |
| F20.2 Catatonic schizophrenia |
| F20.3 Undifferentiated schizophrenia |
| F20.4 Post-schizophrenic depression |
| F20.5 Residual schizophrenia |
| F20.6 Simple schizophrenia |
| F20.8 Other schizophrenia |
| F20.9 Schizophrenia, unspecified |
| F22 Persistent delusional disorders |
| F22.0 Delusional disorder |
| F22.8 Other persistent delusional disorders |
| F22.9 Persistent delusional disorder, unspecified |
| F23 Acute and transient psychotic disorders |
| F23.0 Acute polymorphic psychotic disorder without symptoms of schizophrenia |
| F23.1 Acute polymorphic psychotic disorder with symptoms of schizophrenia |
| F23.2 Acute schizophrenia-like psychotic disorder |
| F23.3 Other acute predominantly delusional psychotic disorders |
| F23.8 Other acute and transient psychotic disorders |
| F23.9 Acute and transient psychotic disorder, unspecified |
| F24 Induced delusional disorder |
| F25 Schizoaffective disorders |
| F25.0 Schizoaffective disorder, manic type |
| F25.1 Schizoaffective disorder, depressive type |
| F25.2 Schizoaffective disorder, mixed type |
| F25.8 Other schizoaffective disorders |
| F25.9 Schizoaffective disorder, unspecified |
| F28 Other non-organic psychotic disorders |
| F29 Unspecified non-organic psychosis |
Schizophrenia
Clinical features
The clinical features of schizophrenia characteristically include one or more of the following:
Cognitive functions are usually intact in the early stages.
Schneiderian first-rank symptoms
One important set of features that can be used in diagnosing schizophrenia is the presence of any of a number of symptoms brought together by Kurt Schneider and known as Schneider’s first-rank symptoms (Table 8.2). In the absence of organic cerebral pathology, the presence of any of these is indicative of, though not pathognomonic of, schizophrenia.
Table 8.2 Schneider’s first-rank symptoms of schizophrenia
| Auditory hallucinations: voices repeating thoughts out loud |
| Auditory hallucinations: discussing the subject in the third person |
| Auditory hallucinations: running commentary |
| Thought insertion |
| Thought withdrawal |
| Thought broadcasting |
| Made feelings |
| Made impulses |
| Made actions |
| Somatic passivity |
| Delusional perception |
Three types of thought alienation (see Figure 5.5; p. 68), in which the patient believes his thoughts are under the control of an external agency or that others are participating in this thinking, are included as first-rank symptoms. He may believe that external (alien) thoughts are being inserted into his mind by an external agency (thought insertion), or that his own thoughts are being withdrawn from his mind by an external agency (thought withdrawal). The third type of thought alienation is thought broadcasting, in which the patient believes that his thoughts are being ‘read’ by others, as if they were being broadcast.
Other ICD-10 symptoms
Subtypes
ICD-10 distinguishes the following major types of schizophrenia.
Paranoid schizophrenia
The clinical picture is dominated by the presence of paranoid symptoms, such as:
Hebephrenic schizophrenia
The following features are typical of this form of schizophrenia:
Other classifications
Syndromal classifications
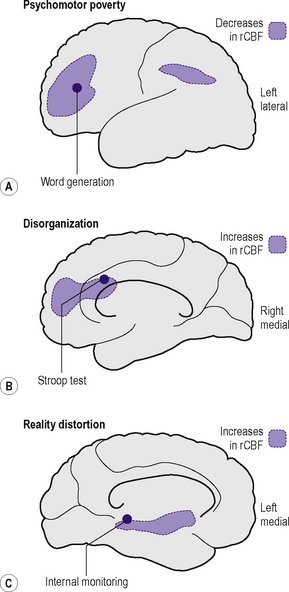
These syndromes can coexist in the same individual. Positron emission tomography (PET) regional cerebral blood flow (rCBF) studies have shown that each of these is associated with a specific pattern of perfusion in paralimbic and associated cerebral cortex and in related subcortical nuclei (Figure 8.1).
A neurodevelopmental classification
Clinical features and classification
visual impairment. It is sometimes related to a paranoid personality or to a mood disorder. Organic brain dysfunction is often found to be present.
Investigations
The investigations carried out in a patient presenting for the first time with schizophrenic symptomatology are those described in Chapter 5, and include:
In the case of first presentation in the elderly, i.e. when the diagnosis being considered is paraphrenia (see Chapter 20), tests of hearing and vision should be carried out at an early stage, as sensory deprivation is an important cause in this age group.
Differential diagnosis
Organic disorders and psychoactive substance use disorders, described in Chapters 6 and 7, should be excluded before making a diagnosis of schizophrenia. A full physical examination and appropriate further investigations (see below) should be carried out, particularly with a first presentation, in order to do this.
Mood disorders (see Chapter 9) may present with symptoms similar to schizophrenia. Negative symptoms and the early stages of simple schizophrenia may be difficult to distinguish from depression. In such cases care should be taken to look for other symptoms of depression. Moreover, depression may itself be a symptom of schizophrenia, both in the acute phase and following an episode of schizophrenic illness (post-schizophrenic depression). Schneider’s first-rank symptoms can occur in mania. Therefore, one should look for other features of mania, particularly if there is no previous history of schizophrenia.
The onset of schizophrenia can lead to personality deterioration, which may simulate a personality disorder (see Chapter 15).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree