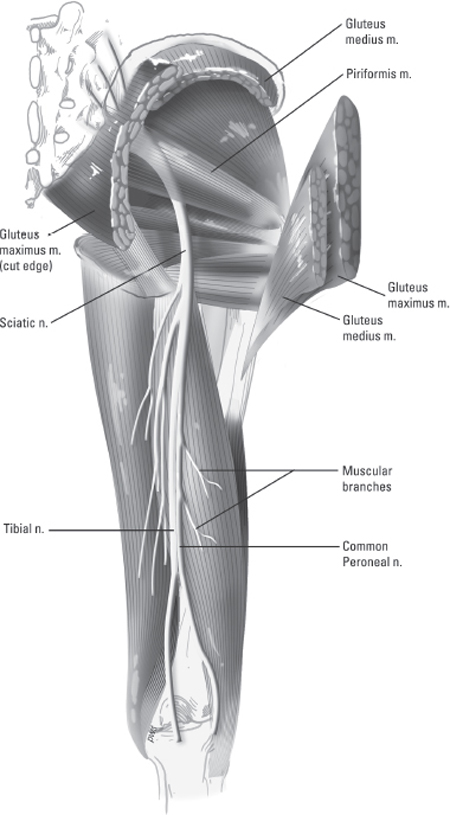
42 Sciatic Nerve Injury and Repair A 32-year-old male was seen in the emergency department after sustaining a through-and-through gunshot wound to the left thigh. The patient reported significant local thigh pain, foot weakness, and loss of sensation down the leg, including the foot. On examination the patient had strong distal pulses, preserved hip flexion and extension, and knee extension against pressure with the injured leg. His left leg below the knee was flaccid and he was limited in knee flexion by local pain. There was detectable hamstring contraction. He had dense but incomplete sensory loss along the lateral and posterior aspects of the lower leg and on all surfaces of the left foot. The left knee reflex was intact but the ankle reflex was absent. Plain radiographs of the left leg were negative for fracture or bullet fragments. A sciatic nerve injury was suspected and after appropriate local care for the gunshot wound and lower extremity bracing, the patient was discharged from hospital with an electrodiagnostic evaluation and neurosurgery consultation scheduled for 3 to 4 weeks from the injury. On follow-up examination the patient had recovered some additional posterior leg sensation and trace plantar flexion of the left foot. He continued to be unable to evert or dorsiflex the left foot or toes. The electromyogram (EMG) showed denervational changes in all lower leg and foot muscles in both the tibial and common peroneal nerve (CPN) distributions. No volitional units were detected in the CPN-innervated muscles, including the short head of the biceps femoris. The patient was prescribed physical therapy to maintain range of motion in the leg and ankle, and continued to use an ankle–foot orthosis for ambulation. At 3-month follow-up evaluation, there was further improvement in posterior leg sensation, knee flexion, and plantar flexion, but the complete deficit in the CPN distribution persisted. A follow-up electrodiagnostic study showed no signs of reinnervation in the CPN distribution. Surgical intervention was recommended at that point. Sciatic nerve injury, complete in the common peroneal nerve distribution As the largest single nerve of the body, the sciatic nerve supplies sensory innervation to the majority of the leg as well as motor innervation to the muscles of the posterior thigh, entire lower leg, and foot (Fig. 42–1). The sciatic nerve originates from the lumbosacral plexus emerging from the pelvis below the piriformis muscle through the greater sciatic foramen to enter the buttock and lower extremity. It receives input from L4 through S3 roots and near its origin often provides articular sensory branches to the posterior part of the hip capsule, if not already directly innervated from the sacral plexus. The nerve enters the dorsal thigh between the ischial tuberosity and greater trochanter. As it courses down into the lower extremity, the nerve hugs the posterior surface of the ischium, covered by the gluteus maximus and accompanied by the posterior femoral cutaneous nerve and inferior gluteal artery. Past the lower border of the gluteus maximus, the sciatic nerve enters the thigh lying on the surface of the adductor magnus muscle. The nerve is crossed obliquely by the long head of the biceps femoris muscle as it descends down the middle of the thigh into the popliteal space. The sciatic nerve most commonly separates into the tibial and common peroneal nerve branches at the upper portion of the popliteal space. However, the nerve may already separate into its two major branches anywhere along its course from its origin through to the lower thigh. The upper terminal branch of the tibial nerve swings superiorly to innervate the long head of the biceps femoris and the upper portion of the semitendinosus. The lower branch of the tibial nerve supplies the lower portion of the semitendinosus as well as the semimembranosus and adductor magnus. After providing a branch to the popliteus muscle, it then courses deep into the posterior compartment of the leg to supply the gastrocnemius, soleus, and plantaris muscles. The common peroneal nerve branch of the sciatic nerve provides innervation to the short head of the biceps femoris before it descends laterally around the fibular head into the lateral and anterior compartments of the leg to provide branches to the peroneus brevis, peroneus longus, tibialis anterior, extensor hallucis longus, and extensor digitorum longus. The long course of the sciatic nerve makes it susceptible to a large variety of injuries, differing in location and etiology. Due to its origin from the greater sciatic foramen and close relationship with the ischial tuberosity, the nerve is subject to injury from hip fractures and surgeries. It can also be compressed or contused against the tuberosity from falls or long periods of inactivity and improper positioning. In the thigh, it may be subject to traction and contusive injuries due to femur fractures as well as penetrating trauma. Figure 42–1 Illustration of the anatomy of the sciatic nerve. Due to variable locations of injuries as well as patient anatomical variations in the branch points of the sciatic nerve into the tibial and common peroneal divisions, the clinical presentation of a sciatic nerve injury is quite variable. Although nearly all injuries cause pain or paresthesias in the buttock or dorsal thigh, motor deficits may be in the common peroneal or tibial nerve distribution or both. Common signs of sciatic nerve injury could be any combination of lateral hamstring weakness, foot drop, or lack of strong toe flexion and plantar flexion. Common peroneal division injuries cause weakness in dorsiflexion and foot eversion and milder weakness of knee flexion due to its contribution to biceps femoris innervation. Sensory loss following CPN injury is confined to the lateral lower leg and lateral and dorsal surfaces of the foot. Tibial division injuries cause weakness of knee and plantar flexion and altered sensation on the plantar surface of the foot. The etiology of sciatic nerve injury varies according to the location of the injury. At the buttock level, the most common cause of injury is from misplaced intramuscular injections. Compression or contusion of the nerve can also occur at the buttock level secondary to pelvic fractures causing a change in the conformation of the sciatic notch or pressure against the ischial tuberosity from a fall. Gluteal muscle wasting or piriformis muscle hypertrophy can also cause a more slowly occurring sciatic nerve compression (see Chapter 41 for discussion of the controversial piriformis syndrome). In the thigh, traction injuries from femur fractures, total hip replacements, or leg lengthening may cause contusion or excessive tension on the nerve. More commonly, gunshot wounds or other penetrating trauma in the thigh may cause lacerations or contusion injuries of the sciatic nerve. Sciatic nerve injury must be differentiated from proximal nerve root injury, lumbosacral plexus injury, and local injury to distal nerve branches. Although pelvic plexus injuries may cause hamstring, dorsiflexion, or plantarflexion weakness, they also commonly have femoral, gluteal, and medial hamstring involvement. Acute proximal nerve root injury may mimic sciatic nerve injury and can be due to compressive spinal lesions, including vertebral fractures or disk herniation. These injuries can be differentiated clinically by their radicular pattern rather than their distal nerve distribution. Electrodiagnostic studies may also show paraspinal muscle denervation in cases of root injury; this feature is absent in plexus or sciatic nerve injury. A sciatic nerve injury should also be considered for all isolated tibial nerve or common peroneal nerve palsies until confirmatory diagnostic evaluation is completed. EMG is often helpful in determining whether sciatic nerve injury is the cause of the patient’ s symptomatology. More importantly, EMG may provide localizing information as to where and what divisions of the nerve are affected as well as the extent of injury. Apart from diagnostic evaluation EMG may also provide important data on the recovery from sciatic nerve injury. Computed tomography (CT) or magnetic resonance imaging (MRI) of the buttock and thigh is not immediately required for diagnosis but may aid in timing or operative planning in cases of pelvic fracture or penetrating trauma. In some cases compressive hematomas of the gluteal region or thigh may be detected on initial CT and provide an indication for evacuation and decompression of the nerve. Ultrasound is becoming a more common modality for imaging peripheral nerves; we have used it to help localize a deep sciatic nerve tumor in the operating room. Magnetic resonance neurography is a very promising modality that has been utilized more recently for evaluation of nerve compression and regeneration following injury. In the setting of acute blunt trauma, initial management of sciatic nerve injury is usually conservative; many injuries will recover spontaneously. The patient should be followed with serial neurological and electrodiagnostic examinations, and if a significant deficit persists without improvement beyond 3 to 4 months, then surgical intervention is recommended. At surgery the lesion is approached working from the normal nerve on either side, and intraoperative nerve action potential (NAP) recording is performed. If an NAP is identified, then external neurolysis is performed. If the NAP is absent, then the lesion is resected back to normal-appearing fascicles, and most often an interposition cable nerve graft is placed. If the lesion appears to affect one division of the nerve more than the other, the tibial and common peroneal components are separated and individually tested electrically. As with other nerves, a clean laceration of the sciatic nerve should be repaired within 48 to 72 hours so that an interposition nerve graft is not needed. In penetrating trauma to the pelvis or leg (including missile injuries) where a ragged laceration of the sciatic nerve is discovered on surgical exploration, the two nerve stumps are sutured with large nonabsorbable suture (or metallic suture material, for later radiographic localization) to the fascia under some tension to minimize nerve retraction. Definitive repair of the nerve occurs at a later time, usually at ˜3 weeks after injury. Most civilian gunshot wounds do not result in complete nerve disruption, and most often a neuroma-in-continuity is the result. If there are no general surgical, vascular, or orthopedic indications for acute exploration, these wounds may be managed as closed, blunt injuries. General management principles of sciatic nerve injury include early mobilization of the affected extremity with physical therapy and appropriate pain control by gabapentin, tricyclic antidepressants, and/or narcotics. Areas of sensory deficit should be assiduously examined for skin breakdown and ulceration. Motor deficits such as a foot drop should be treated with bracing to allow for early ambulation. The deficits associated with partial injury to the sciatic nerve, as seen in blunt injury and contusion, will often improve with conservative management and not require operative intervention. However, in cases of complete or severe deficit in the sciatic nerve distribution, surgery provides the greatest chance for functional recovery. Another indication for surgery is pain refractory to medication, even if the motor deficit is only partial. External neurolysis may result in some degree of pain relief, but a subsequent modulatory procedure such as peripheral nerve or spinal cord stimulation may be needed. The operative approach depends on the level of sciatic nerve injury, either proximally in the buttock or more distally in the thigh. For a proximal lesion, the patient is positioned prone with the injured side elevated slightly and the knee minimally flexed. The classic incision for maximal exposure extends from the posterior inferior iliac spine to midline of the posterior thigh, curving lateral to the gluteal muscles. The gluteus maximus is divided near its insertion into the greater trochanter and reflected medially. A cuff of muscle and tendon must be left for reattachment following nerve repair. Blunt dissection medially along the muscle allows exposure of the sciatic nerve with minimal blood loss. Division of the piriformis muscle improves access to the sciatic notch. During dissection, branches of the sciatic nerve to the hamstring muscles and posterior femoral cutaneous region, as well as gluteal nerves and vessels, must be identified and preserved. Shorter incisions may be used with a muscle-splitting technique directed at more focal regions of the sciatic nerve. Exposure of the sciatic nerve distally is accomplished through a midline incision on the posterior thigh, which may be extended toward the gluteal fold or popliteal fossa. Again the posterior femoral cutaneous nerve should be protected during the exposure. Hamstring muscles may be split in the midline and the long head of the biceps femoris mobilized to expose the nerve. The peroneal division of the sciatic nerve supplies the short head of the biceps femoris, and care must be taken to prevent injury to these branches during dissection. Once the sciatic nerve has been identified, the injured area must be carefully dissected. This is best accomplished by sharp dissection with scalpel or scissors proximal and distal to the presumed area of the injury. The area of injury is dissected last. It is often useful to divide the sciatic nerve into its peroneal and tibial divisions for full assessment of the lesion and to facilitate repair. Each division may be directly stimulated while the nerve is monitored below the injury for the presence of an action potential. If an action potential can be recorded from both divisions, good functional recovery may be achieved by external neurolysis alone. However, the absence of the action potential in either or both divisions necessitates resection and repair of the lesion. If the sciatic nerve is well mobilized and the extent of the lesion is limited, epineurial repair under minimal tension produces optimal outcome. During epineurial repair, careful attention must still be paid to the alignment of the sheath to avoid twisting of the fascicles. Superficial vascular markings on the nerve sheath can help guide the alignment during microsurgical repair. Coaptation of the two nerve ends should be achieved using a minimal number of interrupted nylon sutures, size 6–0 to 10–0, to limit the amount of intraneural scarring, which may obstruct axonal regrowth. To ensure the greatest chance of functional recovery, frayed or devitalized nerve ends must be cleanly trimmed. Because lesions of the sciatic nerve are often extensive, nerve-grafting techniques may be employed to bridge the gap between the two nerve ends, commonly utilizing the sural nerve. In the case described here, the sciatic nerve was exposed through a midline linear incision in the posterior thigh. The tibial and common peroneal branches of the nerve were carefully dissected apart proximal and distal to the site of injury. Both components of the sciatic nerve appeared to contain a traumatic neuroma, but the tibial nerve had minimal scarring after external neurolysis and successfully propagated an NAP. The common peroneal nerve, on the other hand, was densely scarred and did not conduct an NAP. The large neuroma bridging the ends of the common peroneal portion of the sciatic nerve was serially sectioned with a no. 11 blade (“bread-loafing”) until healthy fascicular architecture was identified at each nerve stump. The ipsilateral sural nerve was harvested, and multiple sural nerve cable grafts were then coapted to each nerve stump using interrupted 8–0 nylon suture (Fig. 42–2). Care was taken to avoid any tension at the suture lines, and the repair sites were coated with Tisseel fibrin glue (Baxter International Inc., Deerfield, IL). The patient was discharged from the hospital 2 days postoperatively wearing a knee immobilizer and molded ankle foot orthosis (MAFO). His activity was liberalized 4 weeks postop for range of motion exercises of the leg. The patient was seen serially for the next 3 years, during which time the patient recovered full knee flexion, plantar flexion, and foot inversion. Dorsiflexion and foot eversion recovered to 3/5, but toe extension did not recover. He regained protective sensation on all surfaces of the foot. He was able to ambulate without an orthosis or cane.
 Case Presentation
Case Presentation
 Diagnosis
Diagnosis
 Anatomy
Anatomy
 Characteristic Clinical Presentation
Characteristic Clinical Presentation
 Differential Diagnosis
Differential Diagnosis
 Diagnostic Tests
Diagnostic Tests
 Management Options
Management Options
 Surgical Treatment
Surgical Treatment

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


