Chapter 28 Sensory Abnormalities of the Limbs, Trunk, and Face
Anatomy and Physiology
Sensory Transduction
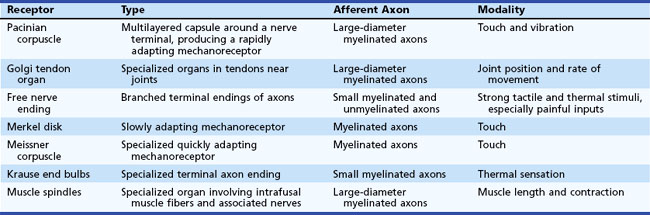
Sensory transducers are seldom directly affected by neuropathic conditions, although peripheral vascular disease can produce dysfunction of the skin sensory axons, and systemic sclerosis can damage skin sufficiently to produce a primary deficit of sensory transduction (Table 28.1).
Sensory Afferents
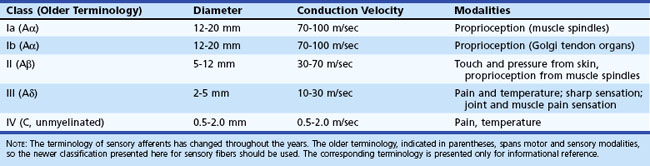
The rate of action potential propagation differs according to the diameter of the axons and depending on whether the fibers are myelinated or unmyelinated. In general, nociceptive afferents are small myelinated and unmyelinated axons. Non-nociceptive afferents are large-diameter myelinated axons. Afferent fiber characteristics are shown in Table 28.2.
Spinal Cord Pathways
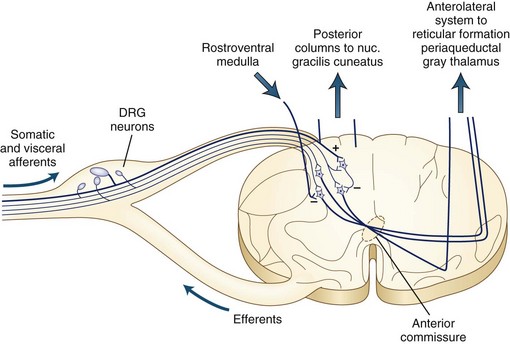
The dorsal column tracts ascend to the cervicomedullary junction, where axons from the leg synapse in the nucleus gracilis and axons from the arms synapse in the nucleus cuneatus. Fig. 28.1 shows the ascending pathways through the spinal cord to the brain.
Brain Pathways
Cerebral Cortex
Classic neuroanatomical teaching presents a picture of the central sulcus bounded by the motor strip anteriorly and the sensory strip posteriorly. This division was derived largely from study of lower animals, in which the separation between these functions is marked. On ascending the evolutionary ladder, however, this division becomes less prominent, and many neurologists refer to the entire region as the motor-sensory strip. In general, sensory function is served prominently on the postcentral gyrus. The mapping of the cortex follows the same homunculus presented in Chapter 23 (see Fig. 23.1), with the head and arm portions located laterally on the hemisphere and the leg region located superiorly near the midline and wrapping onto the parasagittal cortex.
Sensory Abnormalities
Neuropathic pain can result from damage of any cause to the sensory nerves. Peripheral neuropathic conditions result in failure of conduction of the sensory fibers, giving decreased sensory function plus pain from discharge of damaged nociceptive axons. The pathophysiology of neuropathic pain is interesting. Part of its basis is lowering of the membrane potential of the axons so that minor deformation of the nerve can produce repetitive action-potential discharges (Zimmermann, 2001). An additional feature with neuropathic conditions appears to be membrane potential instability, so that the crests of fluctuations of membrane potential can produce action potentials. Finally, cross-talk (ephaptic transmission) between damaged axons allows an action potential in one nerve fiber to be abnormally transmitted to an adjacent nerve fiber. These pathophysiological changes also produce exaggerated sensory symptoms including hyperesthesia and hyperpathia. Hyperesthesia is increased sensory experience with a stimulus. Hyperpathia is augmented painful sensation.
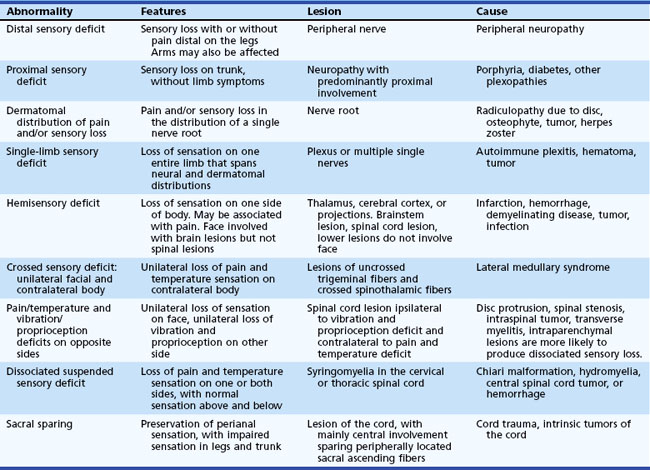
Localization of Sensory Abnormalities
A general guide to sensory localization is presented in Table 28.3. Guidelines for diagnosis of these sensory abnormalities are summarized in Table 28.4. Details of specific sensory levels of dysfunction are discussed next.
Table 28.3 Sensory Localization
| Level of Lesion | Features and Location of Sensory Loss |
|---|---|
| Cortical | Sensory loss in contralateral body restricted to portion of the homunculus affected by lesion. If entire side is affected (with large lesions), either the face and arm or the leg tends to be affected to a greater extent. |
| Internal capsule | Sensory symptoms in contralateral body which usually involve head, arm, and leg to an equal extent. Motor findings common, although not always present. |
| Thalamus | Sensory symptoms in contralateral body including head. May split midline. Sensory dysfunction without weakness highly suggestive of lesion of the thalamus. |
| Spinal transaction | Sensory loss at or below a segmental level, which may be slightly different for each side. Motor examination also key to localization. |
| Spinal hemisection | Sensory loss ipsilateral for vibration and proprioception (dorsal columns), contralateral for pain and temperature (spinothalamic tract). |
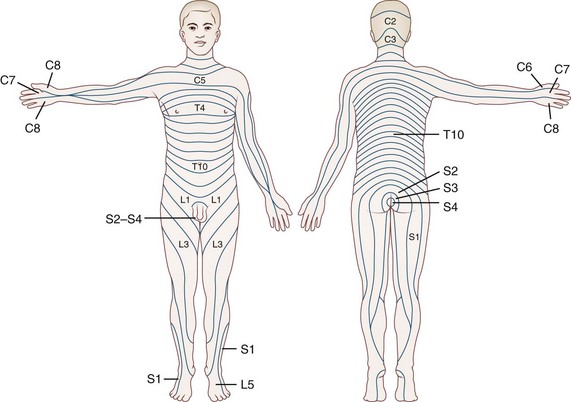
| Nerve root | Sensory symptoms follow dermatomal distribution. |
| Plexus | Sensory symptoms span two or more adjacent root distributions, corresponding to anatomy of plexus divisions. |
| Peripheral nerve | Distribution follows peripheral nerve anatomy or involves nerves symmetrically. |
Peripheral Sensory Lesions
 Distal sensory loss and/or pain in more than one limb suggests peripheral neuropathy.
Distal sensory loss and/or pain in more than one limb suggests peripheral neuropathy.
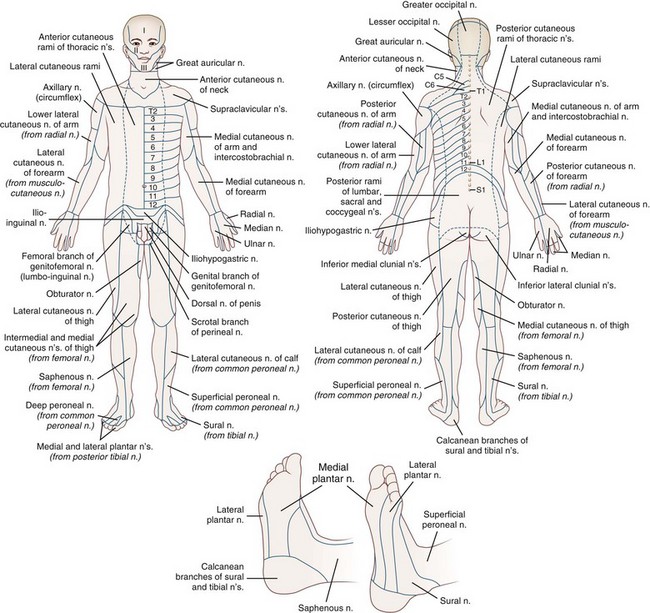
 Sensory loss in a restricted portion of one limb suggests a peripheral nerve or plexus lesion, and mapping of the deficit should make the diagnosis.
Sensory loss in a restricted portion of one limb suggests a peripheral nerve or plexus lesion, and mapping of the deficit should make the diagnosis.
 Sensory loss affecting an entire limb seldom is due to a peripheral lesion, because even proximal plexus lesions rarely affect the entire limb. A central lesion should be sought.
Sensory loss affecting an entire limb seldom is due to a peripheral lesion, because even proximal plexus lesions rarely affect the entire limb. A central lesion should be sought.
Fig. 28.2 summarizes the peripheral nerve anatomy of the body, and Fig. 28.3 shows the dermatomal distribution.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree