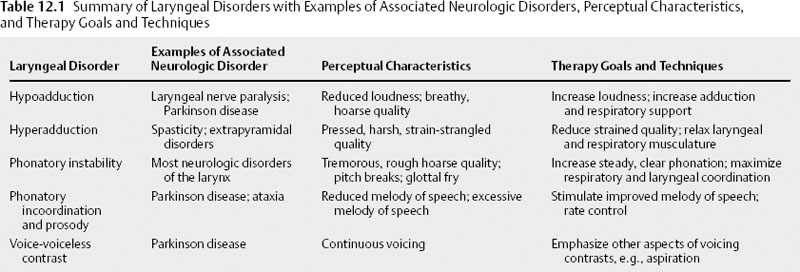
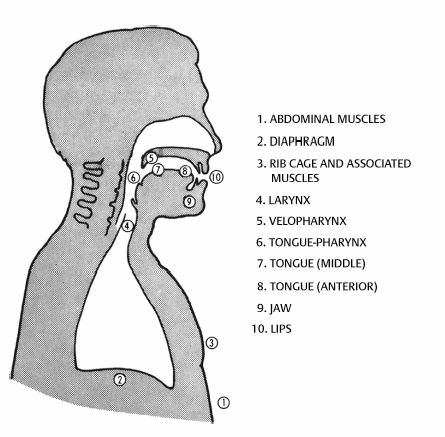
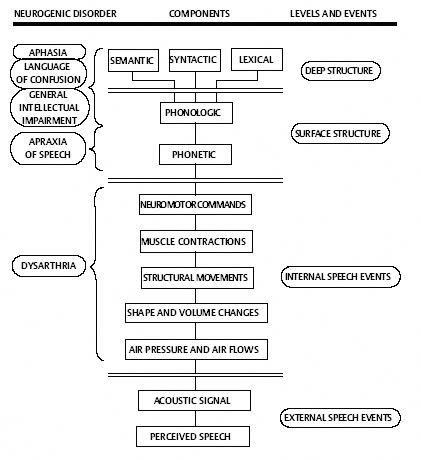
Chapter 12 Speech treatment is essential for overall management of patients with speech and voice disorders secondary to neurologic conditions. Speech treatment may occur in conjunction with medical (surgical, pharmacologic) intervention or as a separate entity. Whatever the case, speech treatment can facilitate maximum improvement in speech intelligibility, acceptability, functional communication, and overall quality of life. The speech pathologist, neurologist, and otolaryngologist function as a team to provide comprehensive diagnosis and management of patients with neurologic disorders of the larynx. Historically, speech treatment of individuals with neurologic voice disorders, especially those associated with degenerative diseases, has been challenging.1 These individuals often have complex disorders that are progressive and involve multiple systems, including cognitive, sensory, and motor problems, as well as attention, vigilance, learning, and memory challenges.1–4 These limitations can make it difficult to obtain successful treatment outcomes. Recently, it has been demonstrated in humans and animals, through clinical and experimental studies, that effective exercise-based behavioral treatment of neurologically based motor disorders, including motor speech disorders (dysarthria), is possible.2,5–9 Among the key elements of such successful treatment are intensive training, increased practice, and active engagement in tasks (salience). These key elements have also been shown to contribute to neural plasticity, brain reorganization, and neural protection, as evident in molecular and cellular studies in animals10,11 and brain imaging and electrophysiologic studies in humans.6,12–14 Importantly, the impact of such exercise has maximum effects when delivered early in the disease process. It has also been suggested that exercise could reactivate mechanisms of plasticity and enhance treatment of functional deficits. Given these facts, the impact of exercise, and its potential to promote or sustain brain plasticity, has moved to the forefront in management of symptoms accompanying neurologic disorders. Our ability to embrace these principles of neural plasticity in the design of our speech treatments for individuals with neurologic voice disorders may allow us to optimize outcomes with these complex and challenging patients. Evidence to support that notion comes from outcome data of Lee Silverman Voice Treatment (LSVT)® LOUD, an intensive, high-effort voice treatment program that embraces many of the plasticity-inducing principles. LSVT LOUD has generated the first level-one evidence for a speech treatment for Parkinson disease through a series of randomized trials (RTCs).2–4 Case studies also indicate effective treatment of speech disorders in other neurologic conditions such as multiple sclerosis,15 cerebellar dysfunction,16 stroke,17 Down syndrome,18 and cerebral palsy.19 If we are to make a significant and lasting impact on speech and voice production in individuals with neurologic voice disorders, we may need to change our conventional treatment paradigms and embrace principles of neural plasticity in the design of our interventions.20 Furthermore, to deliver treatment consistent with the plasticity-inducing intensity and dosage, we may need to turn to technology (Webcam, software, personal digital assistant [PDA]) to offer our patients feasible and adequate access to support learning and long-term maintenance. Some studies in these directions are already being conducted.21,22 The speech therapy approaches presented in this chapter are mainly organized in relation to laryngeal dysfunction, rather than being associated with a specific neurologic condition, as has been done traditionally.23,24 We assume that a direct relationship exists between the laryngeal dysfunction and the resulting sound of the voice and therefore the approach to treatment. We believe that this approach establishes the most direct path to improving the sound of the voice. This approach also accommodates the numerous sources of variation in voice characteristics accompanying neurologic disorders, such as compensatory behaviors, multiple neural pathologies, and neuropharmacologic effects. It also facilitates application of principles of normal laryngeal function to treatment. Specific information about the neurologic disorder is included when it is relevant for determining the most efficacious method to address the disorder. When laryngeal dysfunction is a primary contributor to reduced speech intelligibility, speech therapy is designed to improve or compensate for the underlying disordered laryngeal physiology. Laryngeal dysfunctions in patients with neurologic disorders include problems in adducting the vocal folds (hypoadduction, hyperadduction), producing a stable voice (phonatory instability), and coordinating movements (respiratory-phonatory and phonatory-articulatory incoordination). These dysfunctions may reduce speech intelligibility by affecting the perceptual characteristics of voice pitch, loudness, quality, intonation (prosodic modulation of pitch), and voice-voiceless contrasts (Table 12.1).25 When laryngeal function is affected due to a neurologic disorder, other components of the speech production system are frequently affected as well.23,24 Therefore, it is important to assess laryngeal function and apply treatment strategies within the framework of the entire speech mechanism. One such framework includes the following functional components that are primarily responsible for producing speech: the abdominal muscles, diaphragm, rib cage and associated muscles, larynx, velopharynx, tongue-pharynx, middle portion of the tongue, anterior portion of the tongue, jaw, and lips. (Fig. 12.1).26 Using a sampling of perceptual, acoustic, aerodynamic, and physiologic measures, the speech pathologist evaluates the individual and the interactive contribution of all components of the speech production system to a reduction in speech intelligibility, and makes hypotheses about the disordered physiology underlying the speech problem (Fig. 12.2).27 This information, used in combination with otolaryngologic and neurologic findings, is likely to result in a program of speech therapy that maximizes treatment outcomes for each patient. Fig. 12.1 Functional components of the speaking mechanism, showing areas where the airstream may be valved.(From Netsell R. Lip electromyography in the dysarthrias. Paper presented at the American Speech and Hearing Association, San Francisco, 1972. Adapted with permission.) Fig. 12.2 Components and levels and events involved in different neuropathologies of speech and language.(From Kent R. Study of vocal tract characteristics in the dysarthrias. Paper presented at the Veterans Administration Workshop on Motor Speech Disorders, Madison, WI, 1976. Adapted with permission.) Certain neurologic disorders are accompanied by inadequate vocal fold adduction or hypoadduction. The particular type and extent of hypoadduction may be associated with the site and extent of the related neurologic damage.24 Hypoadduction is typically associated with lower motor neuron involvement, which is characterized by flaccid paresis (weakness) or paralysis (immobility), atrophy (in the case of amyotrophic lateral sclerosis), or fatigue (in the case of myasthenia gravis). Some patients do not adduct the vocal folds and are unable to produce phonation voluntarily. Common etiologies for this form of hypoadduction are closed head injury with brainstem contusion28,29 and brainstem cerebrovascular accident (CVA). Other patients can only partially adduct their vocal folds during speech. This may be unilateral or bilateral and result from damage to (or a disease of) the laryngeal adductor muscles (lateral cricoarytenoid and interarytenoids), to the nerve that innervates them (recurrent laryngeal nerve branch of the vagus),30 or to a disease of brainstem motor neurons, such as flaccid forms of amyotrophic lateral sclerosis.24,31 Other patients may adduct their vocal folds posteriorly, but the folds do not close medially and are said to be bowed. This form of hypoadduction has been associated with bilateral superior laryngeal nerve paralysis24,32 and Parkinson disease (PD).33 Progressive hypoadduction involving restriction of adductor-abductor movements, associated with fatigue accompanying continuous talking, has been observed in patients with myasthenia gravis.32 The major effects of hypoadduction on speech intelligibility are reduced loudness, breathy or hoarse voice quality, and, in some cases, diplophonia (the perception of two pitches). Aerodynamic and acoustic data may show high airflow, short or absent closed phase, low signal-to-noise ratio, reduced intensity range, and short maximum duration.34,35 In certain cases of hypoadduction, patients may be unable to produce adequate voice–voiceless contrasts. Hypernasality and nasal air escape may accompany laryngeal paralysis or paresis if the pharyngeal branch of the motor vagus is affected. Thus, careful examination of the velopharyngeal system is necessary whenever hypoadduction of the vocal folds is present.24 Laryngeal The primary focus of voice therapy for patients without voluntary phonation is to obtain regular vocal fold vibration (voicing) through adduction of the vocal folds with sufficient subglottal air pressure.36 This may be accomplished by attempting to elicit emotive or primitive phonatory behaviors (i.e., laughing, coughing) on a repetitive basis with simultaneous stimulation of subglottal pressure using externally applied abdominal pressure.37 Sapir and Aronson38 reported that digital manipulation of the larynx, stimulated coughing, and prodding to phonate successfully elicited phonation in two patients with whispered phonation accompanying closed head injury. The larynx in these individuals was intact and functional for swallowing and other vegetative functions, suggesting that the abnormal voice was related to limbic–prefrontal lobe dysfunction rather than true paralysis or apraxia of the vocal folds. For patients with reduced adduction accompanying muscle or nerve damage, the primary goal is to increase loudness and reduce breathy, hoarse voice quality by increasing vocal fold adduction and reducing undue vocal fold tension. Procedures to accomplish this are probably the best referenced of all techniques in the area of neurologic voice disorders. The techniques include pushing, pulling, and lifting while phonating.36 When done as a systematic exercise, progressing from vowels to syllables to words to phrases, pushing helps to strengthen the muscles of adduction. In certain cases, these adduction exercises are included as part of LSVT LOUD (described below) to increase loudness in patients with bowed vocal folds accompanying PD.39,40 Other adduction enhancing techniques include hard glottal attack, turning the head to one side or the other (to increase tension on the paralyzed fold), digital manipulation of the thyroid cartilage (to approximate the vocal folds more closely),24 and speaking at a higher or lower pitch (to make use of the adductory function of the cricothyroid muscle).36 Some of these techniques are combined with auditory training and kinesthetic feedback so that the patient can learn how to keep the vocal folds adducted by maintaining audible phonation with good voice quality. Such auditory and kinesthetic monitoring and training41 are facilitated through various forms of biofeedback, including visual feedback of vocal fold adduction through videoendoscopy,42,43 or intensity feedback through a voice light or Visi-Pitch. Support Systems To facilitate the goal of increased loudness and improved quality, the respiratory system is often a focus of treatment. The goal is to achieve a consistent subglottal pressure during speech that is produced with minimal fatigue and appropriate breath group lengths.44 The first step may be to stabilize body posture.45 This may involve the use of support devices such as neck braces, girdling, expiratory boards, or paddles that are implemented in collaboration with the physical therapist and physician. For some patients, working on respiratory support from the supine position is most effective.46 Once the patients’ postural support is maximized, they are instructed, through a hierarchical schedule, to optimally inhale and increase air intake, sustain expiratory airflow for as long as possible, control the rate of expiratory air flow, and produce various levels of subglottal pressure. Various procedures assist patients in increasing systematically the duration and the level of air pressure they can sustain.47 Other techniques to strengthen respiratory muscles include exercises against a resistive load, tracking of a visible analogue of respiratory behavior, and controlled exhalation.48 A 4-week, daily intensive respiratory training with a pressure threshold device and with a regimented treatment protocol based on principles of neural plasticity training has been shown to markedly improve expiratory muscle strength in patients with multiple sclerosis and spinal cord injury.49 To train improved coordination of respiration and phonation, various techniques such as maximum duration vowel phonation39,40 and phonation with simultaneous respiratory (e.g., Respitrace) and vocal (e.g., Visi-Pitch) feedback have been suggested.50 During speech tasks, patients are encouraged to take breaths more often, produce fewer syllables on each exhalation,41,51 and initiate phonation at the beginning of exhalation.37 The goal is to assist patients in organizing their linguistic output into units that are manageable by patients’ peripheral speech mechanism41 and that afford them the greatest gains in speech intelligibility. Patients with hypoadduction may also be encouraged to maximize oral resonance to increase loudness and quality. Linguistically appropriate pauses may help breathing, speech perception, and intelligibility. The use of articulatory gestures to increase vocal loudness is also justified by evidence for orofacial biomechanical and sensorimotor (reflexogenic) influences on vocal folds closure and muscle tone.52 In the case of velopharyngeal insufficiency associated with vagus motor impairment, surgical or prosthetic intervention may be necessary to provide adequate physiologic support, after which speech therapy is initiated.41 Management of the velopharyngeal and articulatory mechanisms are summarized elsewhere.53,54 In certain cases of hypoadduction, a combination of medical management and voice/speech therapy offers maximum results. Voice therapy may precede surgery, or vice versa, for optimal management. After such surgery, speech therapy teaches patients how to achieve maximum vocal efficiency and optimal voice quality and prosody within the new range of function afforded by their modified laryngeal mechanism. In cases where the paralysis is at a paramedian position, with the voice being only moderately affected, it is suggested that the physician and voice clinician should prescribe voice therapy; surgery should be considered only if there is no significant improvement.55,56 In other cases, such as in myasthenia gravis, the primary improvement in voice production may occur with medical management (thymectomy or anticholinesterase drugs)57; intensive exercises to increase vocal fold adduction should not be attempted. To prevent fatigue in these patients, speech therapy may help them learn to economize air intake and use and to minimize vocal effort by using short phrases. Before medical management or speech therapy, or when neither provides the necessary gains in speech intelligibility, augmentative forms of communication (discussed below) may be useful. Hypophonia and dysphonia in individuals with PD have been shown to improve in small pilot studies with repetitive transcranial magnetic stimulation (rTMS) of the primary motor cortex (M1)–mouth area58 and transoral vocal fold collagen injection.59 Hypophonia and dysphonia in other neurologic diseases affecting the laryngeal nerves may also benefit from surgical and prosthetic medialization of the vocal folds.60 Hypoadduction may also occur secondary to conversion disorder and other psychological causes. Coexisting neurogenic and psychogenic dysphonia (such as a paralyzed vocal fold in the paramedian position with complete aphonia that is alleviated with one session of voice therapy) may be seen in some patients. Thus, careful differential diagnosis and special therapy methods are needed for treating the dysphonia.61–63 Certain neurologic disorders result in excess vocal fold adduction, or hyperadduction. In some cases, the ventricular (false) vocal folds may hyperadduct as well.24,64 The particular type and extent of hyperadduction may be associated with the site and extent of the related neurologic damage. Hyperadduction most frequently occurs in cases of bilateral upper motor neuron system disorders characterized by spasticity or hypertonicity, and extrapyramidal system diseases accompanied by abnormal involuntary movements (e.g., tics, chorea, dystonia) that may be focal or generalized.24 Hyperadduction may also occur in cases of long-term use of psychotropic and antiparkinson drugs and is then considered a symptom of tardive dyskinesia.65 In some patients, hyperadduction is so extreme that phonation cannot be initiated or sustained, or can be sustained only with abrupt voice breaks or long duration of aphonia (no voicing). A severe case of adductory laryngospasm associated with adductor spastic dysphonia is an example. Other patients may have moderate hyperadduction, which results in a strained-strangled, harsh voice quality with excessively low pitch and reduced loudness,24 such as in cases of bilateral stroke (pseudobulbar palsy) and spastic cerebral palsy. Still other patients have a mild, continuous hyperadduction, resulting in pitch breaks and a pressed, strained, harsh quality, such as in cases of spastic amyotrophic lateral sclerosis.24 When random periods or “bursts” of hyperadduction or hypoadduction occur, they are frequently associated with dyskinesias such as those associated with Huntington disease, dystonia, and myoclonus. The resulting periods of adductory or abductory laryngeal spasm may generate random, intermittent periods of spastic or breathy voice arrest, respectively.24,66,67 In the case of myoclonus or severe tremor, vocal arrests may be rhythmical.24 It should be pointed out that hyperadduction may be compensatory. For example, a patient may have weak respiratory support or velopharyngeal closure and hyperadduct to manage the airstream for adequate loudness.48 The harsh, high-pitched voice with reduced loudness and pitch variations observed in patients with spinal forms of multiple sclerosis has been associated with the extreme neck and laryngeal tension and upper thoracic and clavicular breathing adopted by these patients in an attempt to produce phrases of normal length.25 The major effect of hyperadduction on speech intelligibility is a quality disorder ranging from a pressed, strained, harsh voice to inaudible speech. Smitheran and Hixon68 reported extremely high measures of laryngeal resistance for a speaker who had a strained-strangled voice quality after multiple, bilateral cerebrovascular accidents. Aerodynamic and acoustic data reveal decreased mean airflow rate69 and reduced fundamental frequency and fundamental frequency range associated with such hyperadduction. Laryngeal The primary focus of voice therapy for patients with hyperadduction is to decrease the pressed, strained voice by reducing vocal fold hyperadduction. Behavioral procedures to accomplish this include those designed to relax laryngeal musculature and facilitate easy voice onset. These techniques frequently begin with progressive whole-body relaxation70 and then focus on relaxing laryngeal musculature. Humming, confidential speech, chanting, and other types of vocalizations mentioned below may help reduce hyperadduction. Techniques of biofeedback-enhanced relaxation have been applied to laryngeal musculature.71,72 The specific form of feedback may be electromyographic or visual (videoendoscopy). Another approach for relaxing laryngeal muscle tension and thereby hyperadduction includes manual massage of extrinsic laryngeal muscles.24,25 Some approaches such as “chewing,” “yawn-sigh,” chanting, and delayed auditory feedback have been used to teach more relaxed and less hyperadducted phonation.36 This relaxed voice production is then shaped into more natural sounding conversational speech. The breathy sigh can be shaped into a relaxed vowel, then to single-syllable words beginning with “H,” followed by open mouth vowels and a nasal consonant or continuant, followed by short duration nasal humming.73 Improved voice quality has been reported in a strained-strangled voice when a speaker raises his pitch, rotates his head backward, and initiates utterances from a high lung volume; these behaviors are associated with decreased airway resistance.68 It was suggested that improved voice quality was the result of passive abduction or relaxation of the vocal folds brought about by the tracheal tug associated with a lower diaphragm position at a higher lung volume level.68 Support Systems To facilitate improved voice quality, the respiratory system is often a focus of treatment in patients with hyperadduction. The goal of respiratory treatment is to achieve consistent, steady airflow with relaxed respiratory musculature.73 The first step may be stabilization of posture. Supporting the abdominal musculature with an elastic band or selective positioning in a reclining wheelchair has helped some patients with spastic dysarthria produce better air flow with less effort and reduced strained-strangled phonation.73 Once the patients’ postural support is maximized, they may then be instructed in procedures of relaxed abdominal breathing73
Speech Treatment for Neurologic Disorders
Speech Therapy Approaches for Laryngeal Disorders that Are Secondary to Neurologic Disorders
Problems with Vocal Fold Adduction
Hypoadduction
Speech Therapy
Speech Therapy and Medical Management in Combination for Hypoadduction
Hyperadduction
Speech Therapy
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







