Chapter 7 Spinal Column
Spinal Cord and Its Coverings
The surface relationships of the spinal cord and its coverings are of great clinical importance throughout life (Fig. 7.1).
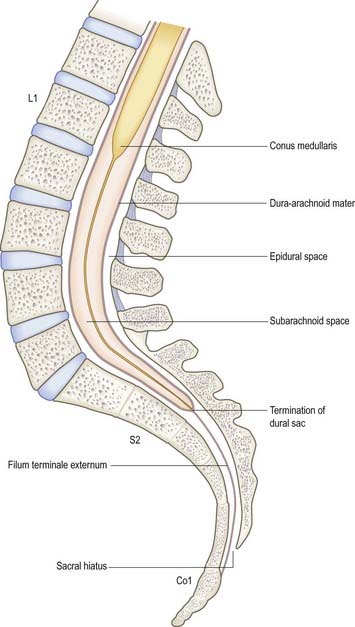
Fig. 7.1 Contents of the vertebral canal in the lumbosacral region.
(Modified with permission from Mackintosh, R.R. 1951. Lumbar Puncture and Spinal Analgesia. E&S Livingstone, Edinburgh.)
Clinical Procedures
Access to Cerebrospinal Fluid
The safest approach to the CSF is to enter the lumbar cistern of the subarachnoid space in the midline, well below the level at which the spinal cord normally terminates (see Fig. 7.1). The fine needle employed is unlikely to damage the mobile nerve roots of the cauda equina. This procedure is called lumbar puncture. It is also possible to access the CSF by midline puncture of the cerebellomedullary cistern (cisterna magna); this is called cisternal puncture.
Lumbar Puncture: Adult
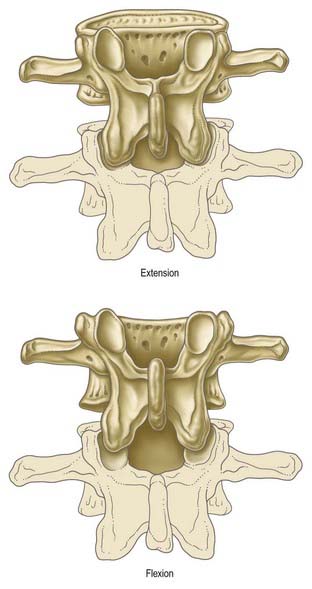
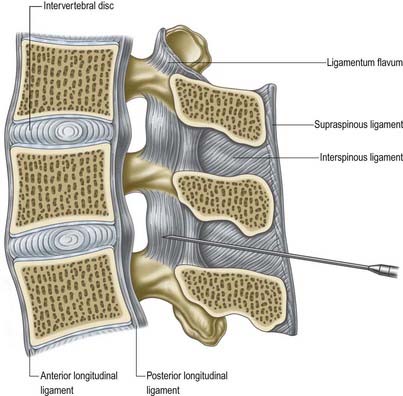
Lumbar puncture in the adult may be performed with the patient either sitting or lying on the side on a firm, flat surface. In each position, the lumbar spine must be flexed as far as possible to separate the vertebral spines maximally and expose the ligamentum flavum in the interlaminar window (Fig. 7.2). A line between the highest points of the iliac crests intersects the vertebral column just above the palpable spine of L4. With the spines now identified, the skin is anaesthetized and a needle is inserted between the spines of L3 and L4 (or L4 and L5). Exact identification of the level by palpation is difficult (Broadbent et al 2000). The soft tissues the needle will ultimately traverse should also be anaesthetized, but care should be taken to avoid injection of an excessive amount of local anaesthetic, which can compromise one’s appreciation of the structures being traversed. These include the subcutaneous fat and supraspinous and interspinous ligaments down to the ligamentum flavum itself. The lumbar puncture needle is then inserted in the midline or just to one side and angled in the horizontal and sagittal planes sufficiently to pierce the ligamentum flavum in or very near the midline (Fig. 7.3).There is a slight loss of resistance as the needle enters the epidural space, and careful advancement pierces the dura and arachnoid to release CSF.
Access to the Epidural Space
Caudal Epidural
The route of access to the caudal epidural space is via the sacral hiatus. The space is thus entered below the level of termination of the dural sac (S2). With the patient in the lateral position or lying prone over a pelvic pillow, the sacral hiatus is identified by palpation of the sacral cornua (Fig. 7.4). These are felt at the upper end of the natal cleft approximately 5 cm above the tip of the coccyx. Alternatively, the sacral hiatus may be identified by constructing an equilateral triangle based on a line joining the posterior superior iliac spines: the inferior apex of this triangle overlies the hiatus. After local anaesthetic infiltration, a needle is introduced at a 45-degree angle to the skin to penetrate the posterior sacrococcygeal ligament and enter the sacral canal. Once the canal is entered, the hub of the needle is lowered so that the needle may pass along the canal (Fig. 7.5). If the needle is angled too obliquely it will strike bone; if it is placed too superficially it will lie outside the canal. The latter malposition can be confirmed by careful injection of air while palpating the skin over the lower sacrum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree