8 With the exception of metastatic spinal column disease in the adult, spinal cord and spinal column tumors are rare. Nonetheless, when confronted with pediatric patients, appreciation of their differences compared with adults will assist clinicians. This chapter reviews pediatric spinal tumors within the classically described compartments—intramedullary, intradural extramedullary, and extradural—and emphasizes the differences from their adult counterparts. Malignancies are the second largest cause of death in children under 15 years of age in North America.1 Approximately 50% of childhood cancers are blood-borne, and 20% involve the central nervous system (CNS).1 Spinal cord tumors account for 4 to 10% of CNS tumors in children,2 and most of the intramedullary spinal cord tumors occur in the pediatric, adolescent, and young-adult age groups.2 In children, tumors of the spine and spinal cord are rarer than are the equivalent tumors in the adult population. The incidence of tumors at specific locations in the spine also differs in the pediatric population compared with adults. In children, ~40% of spinal tumors are intramedullary, 20% are intradural, and 40% are extradural (Table 8-1).3 In the adult population, in contrast, 20% of tumors are intramedullary, 60% are intradural, and 20% are extradural.4,5 Di Lorenzo and colleagues4 reported 1234 cases of pediatric spinal neoplasms, 56 of which were from their institution. In their analysis, the average ratio of pediatric spinal-to-intracranial tumors was 1:6.7, and the ratio of pediatric spinal tumors to those of all age groups was 1 to 12. In these collected series, 31.4% of tumors were intramedullary, 24.4% were intradural, 43.0% were extradural, and 1% was transdural. Raffel and Edwards5 reported 73 cases, with corresponding figures of 42%, 15%, and 36%, respectively. An added leptomeningeal category accounted for 7%. They also reviewed nine earlier series totaling 564 pediatric spinal tumor patients and classified the frequency of neoplasms based on histologic type. The most common tumors were astrocytomas (16%), followed by sarcomas (10%), neuroblastomas (9%), ependymomas (8%), dermoids (7%), and teratomas (7%). Medulloblastomas, neurofibromas, metastatic carcinomas, and lipomas each accounted for 5% of tumors.
Spinal Cord and Column Tumors in Childhood
 Epidemiology
Epidemiology
| Pediatric (%) | Adult (%) | |
| Intramedullary | 40 | 20 |
| Intradural extramedullary | 20 | 60 |
| Extradural | 40 | 20 |
 Intramedullary Spinal Tumors
Intramedullary Spinal Tumors
Several aspects of intramedullary spinal cord tumors differ among adults and children. Astrocytomas are the most common intramedullary childhood tumor, composing up to 90% of tumors. Their relative frequency decreases into adulthood, where ependymomas are most predominant at 60% compared with 24 to 30% for astrocytomas.6,7 In a series of 27 patients less than 3 years of age with intramedullary tumors, no ependymomas were found.8 Hemangioblastomas, the third most common adult intramedullary tumor (7.2% of cases), rarely affect children.7 Spinal gangliogliomas, which are very rare in adults, compose 30% of intramedullary tumors in children under age 3.8 A third of gangliogliomas occur in children. Of those, the spinal cord is involved more frequently (1.7% of CNS tumors) than cerebrum (1.4%) or cerebellum (0.7%).6 Lipomas account for 2 to 6% of pediatric intramedullary spinal cord is tumors.2,6 Lipomas may be true intramedullary lesions, cauda equina lipomas, or those associated with spinal dysraphism.
Low-grade histology predominates in both children and adults, whereas high-grade astrocytic lesions account for 10 to 15% cases.2,7,9 Also similar in both populations is the high incidence of tumor-associated cysts, an association that may contribute significantly to clinical presentation.
Location also slightly differs in children where the cervical spine is affected in 46% of cases, with a relative decrease in frequency in the thoracic (20.5%) and thoracolumbar area (23%).10 In the adult, the most common site of presentation is the thoracic spine.
Clinical Presentation
Typically the presentation of intramedullary spinal cord tumors is insidious. The delay between symptom onset and diagnosis has been as long as 9.2 months in the pediatric population.8,11 Their insidious course may account for the tendency of childhood intramedullary tumors to occupy many segments (six on average) and occasionally to extend throughout the entire spinal cord.12 Malignant lesions tend to exhibit a more rapid progression of symptoms and are typically diagnosed earlier (7-week latency).13 The increasing availability and use of magnetic resonance imaging (MRI) likely shorten the time to diagnosis in the future.
As is the case in adults, the most common presenting symptom is axial pain, typically dull and localized to the involved level. Worsening night pain may result from venous congestion and dural tube distention during re-cumbancy.7,8 Radicular pain is less common and probably caused by distention of the nerve root or infiltration of the dorsal root entry zone.7 Motor deficits in children often manifest as a regression of milestones, delay in walking or crawling, or subtle changes in gait.8 Torticollis associated with cervical spine tumors or kyphoscoliosis with tumors of the thoracic spine result from asymmetric muscle tone and have the potential to worsen neurologic dysfunction.8 Sensory disturbances most often manifest as dysesthesias. Less commonly, dorsal column dysfunction is due to the central location of these tumors in the spinal cord. Bowel and bladder dysfunction is rarely a presenting symptom except when tumors involve the conus medullaris.8,12,14
Hydrocephalus is more common in pediatric patients (15% of cases) than it is in adults.10 This condition may result when malignant tumors disseminate in the subarachnoid space producing metastatic arachnoiditis.13 In this regard, the presence of hydrocephalus increases the likelihood of malignancy and a poor outcome.15 However, 8% of benign tumors also become symptomatic with hydrocephalus.15 Cervical tumors associated with high rostral cysts may cause the leptomeninges at the cervicomedullary junction to thicken, thereby obstructing the outlets of the fourth ventricle. A marked increase in the concentration of cerebrospinal fluid (CSF) protein may also contribute to CSF obstruction.
Less commonly, incidental findings on plain radiographs obtained in response to nonspecific symptoms like abdominal pain or a refusal to bear weight reveal a tumor; however, plain radiographs may be normal in 25 to 50% of children with spinal neoplasms.10
Diagnostic Imaging Studies
The diagnosis of intramedullary spinal cord tumors has been revolutionized by the advent of MRI. Now, a swift and timely diagnosis of an intramedullary spinal cord tumor can be obtained noninvasively in most children. Although plain radiographs (showing interpedicular widening or scoliosis) or computed technology (CT) (suggesting intraspinal syrinx formation) are sometimes helpful, the use of these modalities has largely been supplanted by the availability of MRI.
Intramedullary tumors typically enhance markedly after the administration of contrast on MRI (Fig. 8-1). Spinal cord astrocytomas, hemangioblastomas, and ependymomas may have a tumor-associated cyst that helps delimit the tumor from the surrounding normal spinal cord. Such cystic collections are of great value to neurosurgeons in determining the limits of resection intraoperatively.
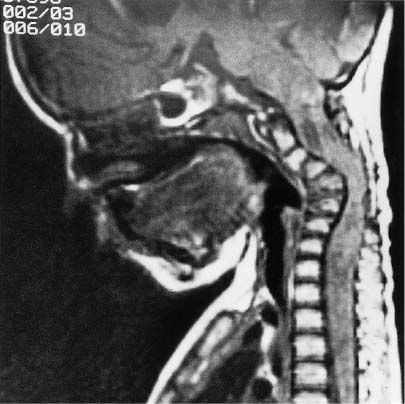
Intramedullary spinal lipomas are readily identified by T1-weighted MRI; the lipomatous mass lesion is identified as a high-signal intensity area (Fig. 8-2). In these cases, the demarcation between lipoma and normal spinal cord tissue is never precise. The fatty mass blends imperceptibly with the normal spinal cord tissue elements.
Electrophysiologic Monitoring
The use of electrophysiologic monitoring has become widespread in surgery for lesions of the spinal cord. The intent is to allow aggressive resection while minimizing neurologic morbidity. Somatosensory evoked potentials (SEPs) largely reflect posterior column function but are limited by inadequate baseline readings in most patients and signal loss resulting from dorsal myelotomy, which is the usual approach to these lesions.7 Motor evoked potentials (MEPs) largely record from motor tracts. MEPs are increasingly monitored in the operating room. Their use, however, is more difficult in the pediatric population because myelination of the corticospinal tract is incomplete in children less than 3 years old and the immature neural structures are more vulnerable to compression.7
Osteoplastic Laminotomy
The midline posterior approach to these tumors necessitates removal of the lamina. In the adult this procedure is usually well tolerated. Stability depends on the integrity of facet joints, and supplementation with instrumentation for spinal fusion is an option when facets have been breached.

FIGURE 8-2 Sagittal MRI showing extensive cervical intramedullary lipoma. This lesion extends from the medulla to the bottom of the cervical spine. There appears to be a clean plane of demarcation between lipoma and spinal cord, but this is not the case histopathologically. These lesions may be debulked, but aggressive surgical resection is not recommended.
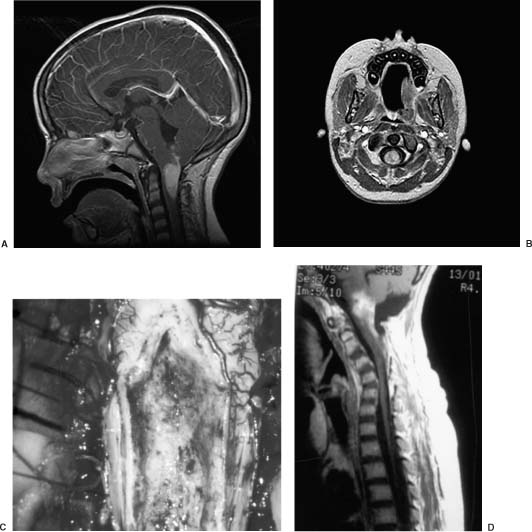
In the pediatric population, however, instability and fusion are more problematic. There is a 36% incidence of instability after multilevel laminectomy for intramedullary tumor in patients less than 15 years of age.16,17 This incidence falls to 6% for the group 15 to 24 years of age. Instability is most common in the cervical spine and almost nonexistent in lumbar cases. The instability is attributable to the role of the dorsal ligaments in providing a significant tension band that prevents overt forward flexion. Instability, coupled with neurologic dysfunction and muscle asymmetry as a result of the tumor, leads to progressive deformity (Figs. 8-3 and 8-4). To avoid this problem many surgeons advocate an osteoplastic laminotomy approach. In this procedure the posterior elements are replaced at the time of closure, allowing restoration of the ligamentous structures and protection from delayed deformity while avoiding spinal fusion (Fig. 8-5). In one study nine of 25 patients developed progressive kyphoscoliosis after laminectomy, whereas only three of 20 patients who underwent osteoplastic laminotomy progressed.3 In this latter group all patients developed a recurrent tumor. Using the same rationale, minimally invasive surgery, consisting of unilateral hemilaminectomy and reconstruction, has also been advocated. Two series appear to show adequate prevention of postoperative spinal deformity using this technique.18,19 Spinal bracing is also widely used to manage this problem; however, its efficacy is unproven.
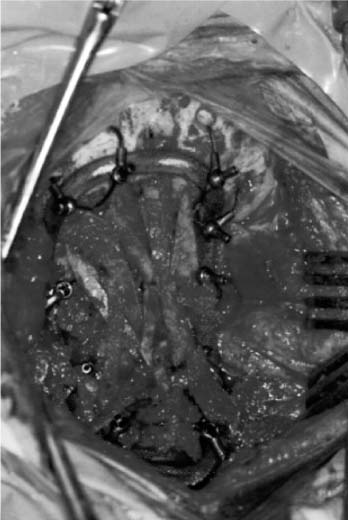
FIGURE 8-4 Intraoperative photograph showing an occipital-C4 fusion construct using a titanium Luque rod construct.

FIGURE 8-5 Immediate postoperative axial computed tomography (CT) of the cervical spine showing laminoplastic osteotomies with the spinous process replaced in situ. Such a technique has been associated with fewer instances of spinal deformities than multilevel laminectomies.
Extent of Resection
Intramedullary spinal tumors are rare in both the adult and pediatric population. Consequently, randomized trials are almost impossible to conduct. The literature on treatment is composed of uncontrolled series, largely retrospective, spanning lengthy periods, during which time advances in imaging and technique occurred. Although several studies address the issue of extent of resection, the reason for limiting a resection is unclear and a selection bias is likely. Nonetheless, it seems clear that low-grade solid tumors benefit from radical resection (Figs. 8-6 and 8-7).20 The controversy arises for infiltrative tumors, particularly fibrillary astrocytomas, where complete resection is impossible and a true radical resection causes significant neurologic morbidity.21 Although lipomas are benign, they also present a surgical challenge because a plane for dissection is rarely present. These tumors can seldom be resected without causing significant neurologic injury.6
Adjuvant Therapies
The scientific evaluation of adjuvant therapies for intramedullary spinal tumors is even more difficult than the evaluation of surgery because such treatment applies to an even smaller subset of patients. The indolent nature of low-grade lesions initially does not seem to warrant adjuvant treatment.20 Radiation and chemotherapy regimens are largely sought for high-grade lesions, especially when they are resected incompletely or recur.20
Because of its deleterious effect on the developing nervous system and secondary effects on the growing spinal column, radiation is offered reluctantly in such cases.22 Application to low-grade lesions is made further undesirable by the high incidence of secondary malignancy in children. In one study, the 10- and 20-year secondary malignancy rates after radiation were 4 and 13%, respectively.23
Outcome
The only significant predictors of outcome identified in the literature are histologic grade and preoperative neurologic function.7 Patients with a mild deficit tend to improve significantly, whereas those with significant disability tend to respond poorly to surgical resection.24,25 For ependymomas, total excision is often possible and is curative.26 Low-grade astrocytomas exhibit a high 5-year survival rate, with age being a positive prognostic factor; younger patients are more likely to develop the pilocytic variety with its more favorable prognosis. Here again, aggressive resection should be mandatory.27 Malignant astrocytomas exhibit a relentless progression, and the mortality rate (79%) within 6 months of diagnosis is high.13 In this condition the extent of surgical resection likely influences the outcome little.
 Extramedullary Spinal Tumors
Extramedullary Spinal Tumors
Extramedullary lesions include all tumors lying outside the neural tissue of the spinal cord. Unlike intramedullary tumors, this group constitutes a wide variety of neoplasms that can be further separated into intradural extramedullary and extradural. Most published studies on pediatric spinal tumors cover both intramedullary and extramedullary components, including nonneoplastic lesions and developmental masses.4,5,9,28–31 It is therefore difficult to estimate the true incidence of all spinal tumors, especially extramedullary lesions, due to their diverse nature (Table 8-2).
Clinical Presentation
In both adults and children, the most common presenting symptom of extramedullary spinal tumors is pain. In very young children, especially in the preverbal age group, pain is not expressed easily and can be manifested by irritability or refusal to ambulate. Because of this limitation, diagnosis is often delayed in young children until other symptoms such as motor deficits appear. Neurologic deficits, therefore, are often advanced at the time of presentation.9,32–34 Early, localized, spinal pain is often the predominant symptom of extradural tumors, whereas radicular pain often suggests an intradural-extramedullary location.35 In their review of intraspinal tumors, Raffel and Edwards5 analyzed a series of 431 children, and weakness was the predominant presenting symptom in more than 67% of cases. Other signs included reflex changes (49%), sensory changes (30%), abnormal spinal curvature (28%), muscle atrophy (19%), tenderness (14%), spasms (13%), paraspinal mass (12%), and torticollis (8%). Referred pain from nerve root compression sometimes leads to misdirected investigations for abdominal complaints.36 Cervical tumors can cause neck stiffness and head tilt. The tendency of several of these lesions to involve the conus medullaris and cauda equina yields a mixed myelopathic and radiculopathic neurologic picture. Metastatic lesions typically manifest with pain and neurologic dysfunction referable to the location of the tumor. Presentation is usually less insidious than with other tumors, and suspicion is often heightened by a history of a previous CNS malignancy.
| Intradural | Extradural |
| Congenital tumors Epidermoids/dermoids Teratomas Meningeal tumors Meningiomas Nerve sheath tumors Schwannomas Neurofibromas Vascular tumors Hemangioblastomas Metastatic tumors Blood borne Leukemias Lymphomas Neural origin Gliomas Peripheral neuroectodermal tumors | Neural crest tumors Ganglioneuromas Neuroblastomas Mesodermal tumors Sarcomas Bone tumors Primary benign Osteoblastomas Aneurysmal bone cysts Primary malignant Ewing’s sarcomas Osteogenic sarcomas Chordomas Metastatic |
Lipomas offer little diagnostic challenge because they become symptomatic at an early age with subcutaneous manifestations of the tumor. In early childhood these patients may develop an asymmetric foot deformity, foot-length discrepancies, atrophic skin ulcerations on the feet, scoliosis, and lower extremity weakness.37,38 Beyond 3 to 4 years of age patients often exhibit symptoms of a neurogenic bladder.38 In adolescents, back pain becomes more predominant.38
Tumors associated with a dermal sinus tract such as dermoids, epidermoids, and lipomas may present with repeated bouts of bacterial meningitis. Dermoids and epidermoids can rupture and also induce chemical meningitis. In this scenario the diagnosis is made by microscopic observation of keratin in the CSF.39 Subarachnoid hemorrhage from an intraspinal tumor has also been reported, although this phenomenon is unusual.5,33,40,41 The most common lesions leading to subarachnoid bleeding are ependymomas of the cauda equina and neurinomas.40,41 Both intradural and extradural spinal tumors have been associated with hydrocephalus and increased intracranial pressure. The hydrocephalus results from increased CSF viscosity or from obstruction of CSF pathways by tumor seeding.42–44 Laboratory investigations can be helpful in the diagnosis of neuroblastomas. Serum and urine levels of the catecholamines, vanilmandelic acid (VMA), and homovanillic acid (HVA) are elevated in patients with neuroblastomas. Ewing’s sarcoma can lead to leukocytosis, an increased sedimentation rate, and elevated lactate dehydrogenase (LDH).
 Intradural Extramedullary Spinal Cord Tumors
Intradural Extramedullary Spinal Cord Tumors
Epidemiology
This group of tumors includes dermoids and epidermoids, ependymomas, lipomas, germ cell tumors, nerve sheath tumors, meningiomas, and leptomeningeal deposits of intracranial or intraspinal neoplasms. In the pediatric populations the most common tumors are the metastatic CNS lesions, usually along the dorsal surface of the spinal cord or within the cauda equina.10,45 The most common neoplasms are medulloblastomas with spinal metastases reported in 9.6 to 45% of cases.10,46,47 Nerve sheath tumors and meningiomas, which compose most adult tumors (55%) in the intradural extramedullary compartment, account for only 10.9% and 4.3%, respectively, in children.10 Pediatric nerve sheath tumors rarely occur singly and are more common in patients with neurofibromatosis. These tumors can extend into the extradural compartment and do so more frequently than their adult counterparts (Fig. 8-8).48 Dermoid and epidermoid cysts account for 3 to 13% of spinal tumors in children and 17% of those discovered within the first year of life.39 These lesions may be associated with spina bifida or posterior dermal sinus tracts.39 Lipomas in the extramedullary compartment occur at the conus medullaris and are often termed lipomyelomeningoceles. They are almost always associated with a lumbar subcutaneous extension present at birth and occult dysraphism.37 Extramedullary ependymomas are located at the conus medullaris and are thought to arise from ependymal cell rests within the ventriculus terminalis and filum terminale.49
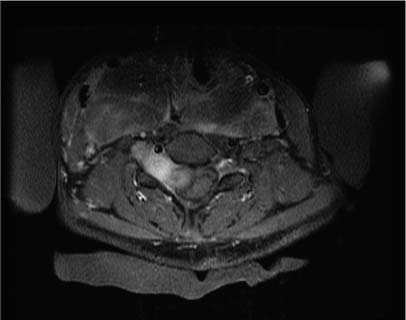
FIGURE 8-8 Axial CT of a large interverterbral foramen neurofibroma in a patient with neurofibromatosis type 1.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree