FIGURE 50.1 A 33-year-old woman with systemic lupus erythematosus, antiphospholipid antibody syndrome, status postquintuple coronary artery bypass graft, who developed acute cardiac tamponade and hepato-renal syndrome. She was found to have flaccid paraplegia of the lower extremities. Pre- and postcontrast MRI (sagittal and axial) of the lower thoracic spinal cord and conus medullaris demonstrates abnormal high signal intensity most prominent at the levels of T11 and T12, as seen on the T2-weighted images. These findings are consistent with spinal cord ischemia. (Courtesy of Dr. José Biller.). MRI, magnetic resonance imaging.
ACUTE SPINAL CORD INJURY
A. Etiology. The major causes of acute spinal cord injury are motor vehicle accidents, falls, recreational injuries, and acts of violence. Fracture and compromise of the spinal cord (or cauda equina) occur most often at cervical and thoracolumbar levels. Although thoracic fractures are less common, neurologic injury is more common because of the narrowness of the spinal canal.
B. Prevention. Proper use of passive and active restraints in automobiles and use of helmets by motorcyclists and bicyclists prevent head and spinal injuries. For example, the Think First program, which addresses educational issues for youth in kindergarten through 12th grade and is actively supported by the neurosurgical community, should be embraced by health care providers.
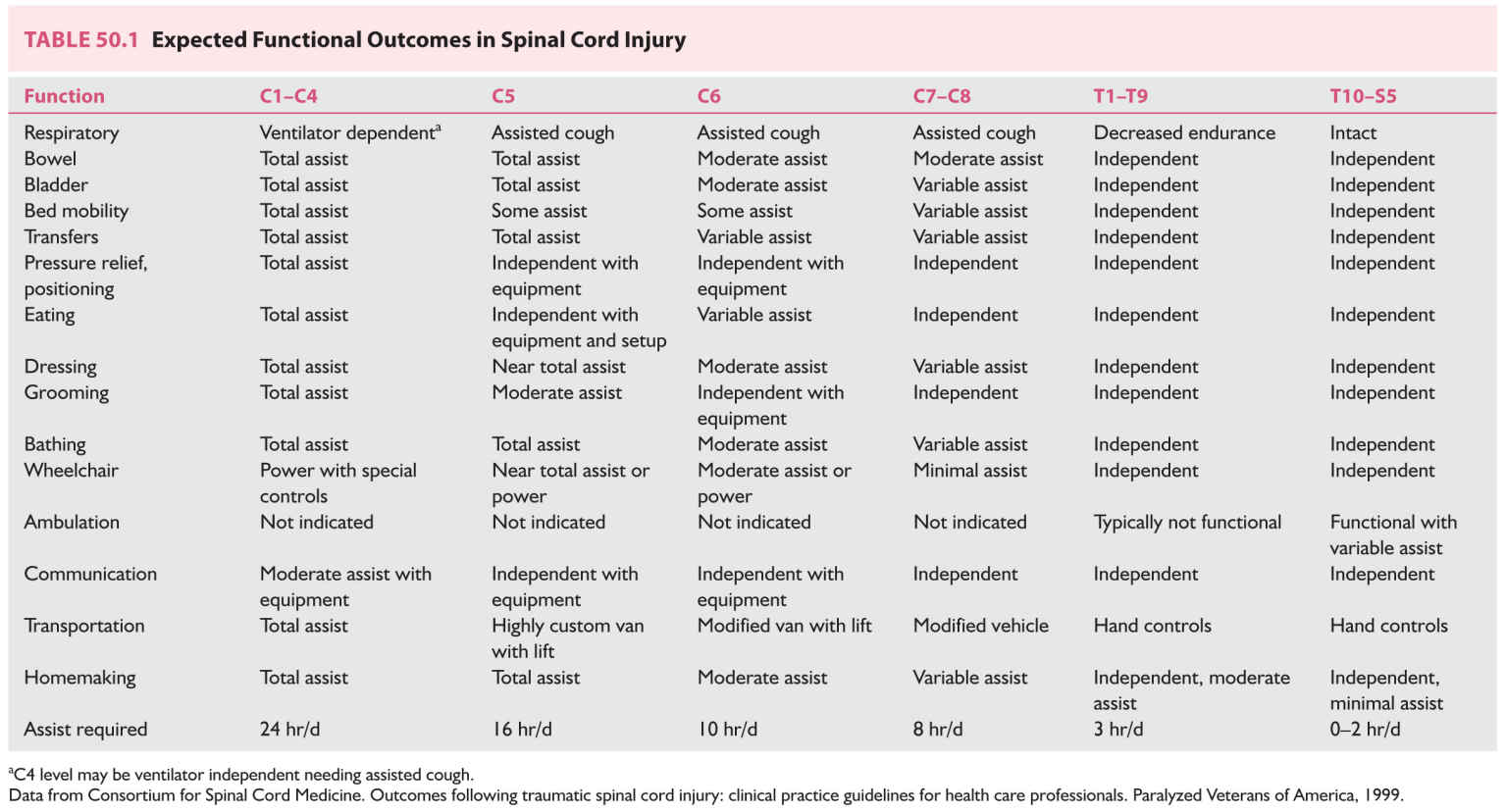
C. Prognosis. Improvement of even one level can have a dramatic effect on function, especially in cervical cord injuries (Table 50.1). Final neurologic function depends on severity of initial injury, prevention of secondary damage, and successful management of the complications and sequelae of the acute injury and intensive rehabilitation. Neurologic assessment 72 hours after injury according to American Spinal Injury Association guidelines is useful in estimating outcome.
1. Features suggesting a possibility of neurologic improvement are as follows:
a. Motor or sensory function below neurologic level (incomplete lesion).
b. Degree to which motor strength is preserved below neurologic level.
c. Preservation of pinprick response in addition to light touch below neurologic level.
d. Age <30 years.
e. Residual anal sphincter tone.
f. Relatively well-preserved vertebral alignment.
2. Features suggesting a poor prognosis are as follows:
a. Absence of residual function (complete lesion).
b. Hemorrhage or multilevel edema on MRI.
D. Principles of treatment.
1. Immobilization of the spine at the scene, in transport, and in the emergency department is critical in preventing further damage.
2. ABCs of trauma care; supplemental oxygen should be provided.
3. Primary survey of associated damage.
a. Alteration of sensorium necessitates investigation for accompanying head injury.
b. Neurologic level may mask the usual symptoms and signs of thoracic, abdominal, pelvic, or extremity injury. More reliance is placed on objective tests.
4. Radiologic evaluation of level of skeletal injury.
5. Skeletal traction for stabilization and closed reduction if indicated.
6. Assessment of neurologic level of injury.
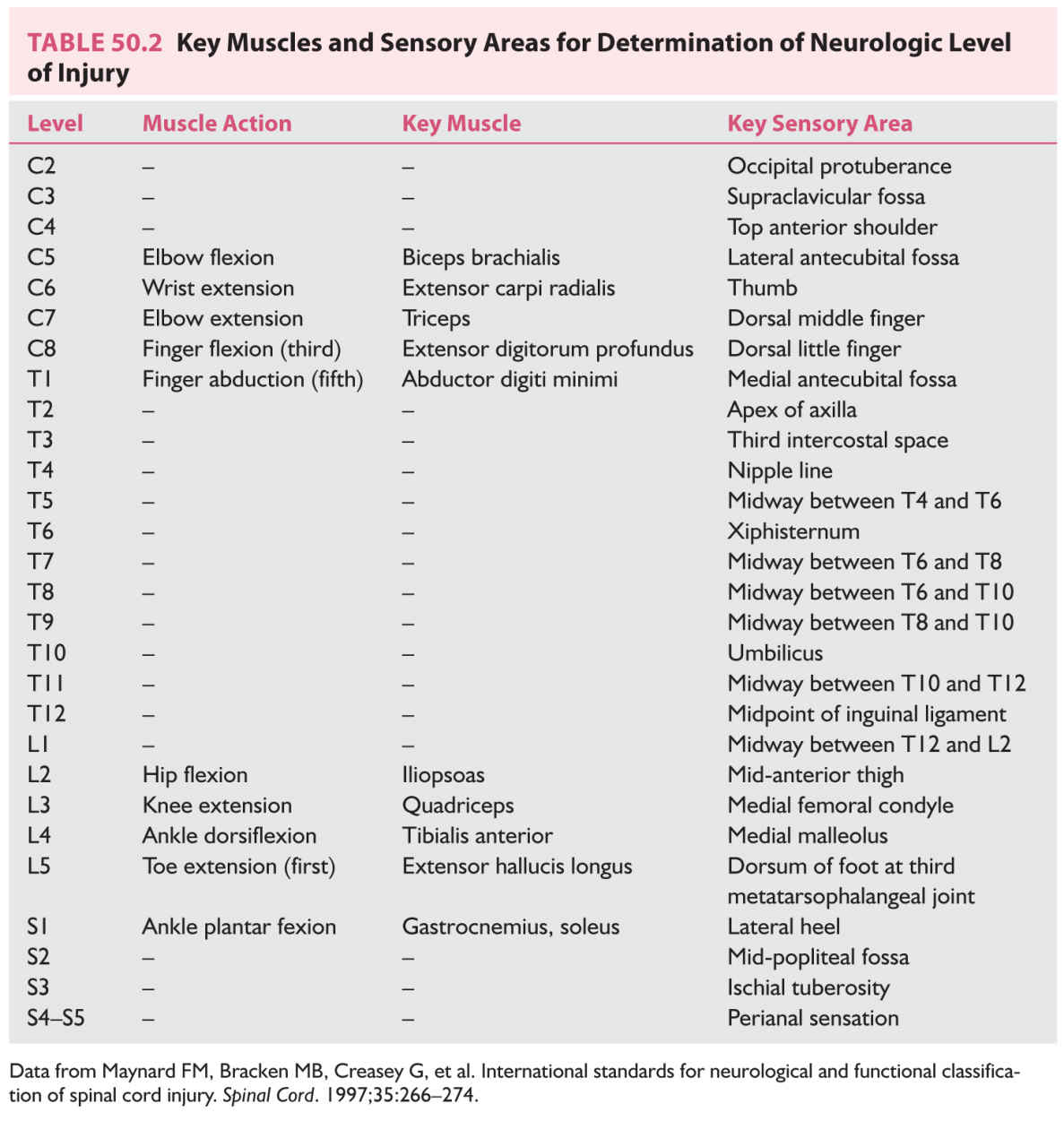
a. The neurologic level of injury is the most caudal segment at which both motor function and sensory function are intact bilaterally (Table 50.2).
b. The completeness of the injury is defined by American Spinal Injury Association classes grades A through E, which describe function at least three levels below the neurologic level of injury. Grade A indicates a complete level, grade E indicates recovery, and grades B through D describe incomplete levels.
7. Secondary survey and stabilization of patient’s condition.
8. Transport to spinal cord injury center.
9. Surgical decompression preferably done within 24 hours in select cases.
10. Medications to prevent secondary (oxidative) damage.
a. The National Acute Spinal Cord Injury Study 2 (NASCIS 2) showed a modest but significant benefit compared with placebo for high-dose methylprednisolone if started within 8 hours of injury. The initial dose of 30 mg/kg intravenous bolus is followed by 5.4 mg/kg/hour infusion for 23 hours. Complications include pneumonia, sepsis, and gastrointestinal hemorrhage.
b. NASCIS 3 showed an additional 24 hours of steroid infusion to be beneficial to patients who received the initial bolus between 3 and 8 hours after injury. Treatment started at later than 8 hours after injury resulted in poorer outcomes than did placebo treatment.
c. However in 2013, based on further data, the American Association of Neurological Surgeons (AANS)/Congress of Neurological Surgeons (CNS) Guidelines for the Management of Acute Cervical Spine and Spinal Cord Injury issued a level 1 recommendation that administration of MP for the treatment of acute spinal cord injury is not recommended.
d. There is some controversy around this change of guideline, and some physicians advocate treating on a patient to patient basis, balancing the potential risks and benefits for each patient. Specifically, patients with cervical spinal cord injury have been found to be less prone to the complications of methylprednisolone.
11. Restoration and maintenance of spinal alignment.
SEQUELAE OF SPINAL CORD INJURIES
A. Pressure sores are the most preventable complication of spinal cord injury.
1. Prevention. Patient and family education are important. Pressure is relieved by turning in bed every 2 hours and “wheelchair” lifts for 5 to 10 seconds every 15 to 30 minutes. Special mattresses and wheelchair cushions do not obviate proper positioning and frequent repositioning. The skin is kept clean, dry, and inspected daily. Attention is paid to nutritional requirements.
2. Pressure relief. A repositioning schedule ensuring that the sore is always pressure free needs to be rigidly followed because the reduced number of possible weight-bearing position makes another sore more likely. Simultaneous management of more than one pressure sore requires special frames or flotation beds.
3. Debridement. Saline wet-to-dry gauze and whirlpool therapy are standard, but commercial enzyme preparations are less labor intensive. If the eschar is hard and blackened, necrotic tissue is removed surgically.
4. Dressings. Shallow ulcers are covered with sterile gauze. Occlusive dressings may promote more rapid healing and have to be changed less often but are much more expensive. Deeper, pear-shaped ulcers are loosely packed with saline-soaked gauze to prevent abscess formation and to promote “bottom-up” healing. The goal is to keep the wound moist, whereas the surrounding tissue is kept dry.
5. Electrical stimulation may accelerate wound healing.
6. Surgical excision with a myocutaneous flap to fill the cavity is usually required for deeper ulcers. Reduction of bony prominences may be necessary.
B. Deep venous thrombosis is a serious concern after spinal cord injury. Pain may not be felt below a sensory level, and swelling may be masked by edema and vasomotor changes.
1. Prophylaxis is needed for up to 3 months or until discharge from the rehabilitation unit. Intermittent pneumatic compression devices or compression stockings are used for the 2 weeks after injury. Anticoagulation with low-molecular-weight heparin or adjusted-dose unfractionated heparin should be started 48 to 72 hours after injury and continued 8 to 12 weeks depending on associated risk factors. Vena caval filters are placed in patients with contraindications to or who have undergone unsuccessful anticoagulation therapy. Filters should also be considered in addition to anticoagulation in the care of patients with complete C2 or C3 neurologic levels of injury.
2. Treatment is the same as that of patients without spinal cord injury. Mobilization and exercise of the lower extremities should be withheld 48 to 72 hours until anticoagulation is adequate. Pain relief should be provided to lessen the possibility of autonomic dysreflexia.
C. Autonomic dysreflexia. From 30% to 85% of patients with quadriplegia or high paraplegia have paroxysmal episodes of severe hypertension, sweating, flushing, and piloerection accompanied by headache, chest pain, and bradycardia or tachycardia in response to relatively benign stimuli below the level of injury. Pulmonary edema, intracranial hemorrhage, cerebral infarction, seizures, or death can result. Bladder and bowel distention, instrumentation, or irritation are the most common precipitating stimuli.
1. Etiology. In the setting of a spinal lesion above the major splanchnic outflow tract (T6–L2), reflex activation of sympathetic discharge occurs below the lesion unchecked by descending inhibitory pathways from supraspinal centers.
2. Management. Initial treatment entails removal of the precipitating stimulus and medication for the hypertensive crisis.
a. Removal of precipitating stimulus.
(1) Stop procedure.
(2) Check for urinary catheter blockage.
(3) Remove tight clothing, shoes, straps, and other restrictive items.
(4) Catheterize carefully with 2% lidocaine jelly.
(5) Perform kidney, ureter, and bladder and rectal examination with lidocaine jelly to check for impaction.
(6) Check for sores, infection, trauma, and fractures.
(7) Consider acute abdomen and deep venous thrombosis.
b. Management of hypertension.
(1) Elevate head of bed or place patient in sitting position to induce postural changes in blood pressure.
(2) Drug therapy.
(a) Nifedipine 10 mg by mouth (immediate release form—bite through capsule and swallow); monitor response or
(b) Nitroglycerin 2% ointment—1 inch (2.5 cm) applied above neurologic site of injury; monitor response.
(3) If blood pressure remains critical, intravenous protocols (e.g., hydralazine, diazoxide, and sodium nitroprusside) for hypertensive crisis must be initiated.
c. Management of profuse sweating without hypertension. Give propantheline at 15 mg by mouth (may be repeated after 10 minutes) or oxybutynin at 5 mg by mouth (may be repeated after 10 minutes).
3. Prophylactic medications.
a. Nifedipine 10 mg by mouth 30 minutes before procedure.
b. Phenoxybenzamine 10 to 20 mg by mouth three times a day.
c. Scopolamine patch may help with reflex sweating.
D. Depression must be continually assessed and managed.
E. Central pain syndrome. Development of chronic dysesthesia or central (neuropathic) pain above, at, or distal to the level of injury poses therapeutic challenges. Central pain is in addition to the musculoskeletal and visceral pain experienced by patients with spinal cord injuries.
1. Etiology.
a. Above level of injury. Compressive mononeuropathy (e.g., ulnar and median) and posttraumatic syringomyelia formation.
b. At level of injury. Central pain from cord damage, radicular pain from root damage, and complex regional pain syndrome.
c. Below level of injury. Central pain.
2. Pharmacologic approach is trial and error.
a. Tricyclic antidepressants for nonlancinating pain.
(1) Amitriptyline (Elavil) or nortriptyline (Pamelor) 10 to 25 mg by mouth at bedtime; increase by 10 to 25 mg every 5 to 7 days as tolerated to 75 to 150 mg at bedtime.
(2) Side effects include sedation, anticholinergic effects, orthostatic hypotension, weight gain, and cardiac arrhythmia.
(3) If side effects are not tolerable, a chemically unrelated compound, such as duloxetine (Cymbalta) at 30 to 60 mg/day by mouth, may be tried.
b. Anticonvulsants (frequently in combination with tricyclic antidepressants) for lancinating central pain.
(1) Carbamazepine (Tegretol) 100 mg twice a day increased 100 mg every 3 days as tolerated to a serum level of 8 to 10 mg/mL in three or four doses per day.
(a) Side effects include sedation, diplopia, gastrointestinal upset, ataxia, weakness, rash, and bone marrow suppression.
(b) Monitor CBC with platelets every 2 weeks for 3 months, then CBC, platelets, and liver function every 3 to 6 months.
(2) Gabapentin (Neurontin) 100 mg three times a day increased 100 to 300 mg every 3 days as tolerated up to 600 to 900 three or four times a day.
(a) Side effects include drowsiness and dizziness.
(b) Blood levels are not used clinically, and no monitoring is needed.
(3) Pregabalin (Lyrica) 50 mg three times a day increased to 100 mg three times a day after 1 week as tolerated.
(a) Side effects include peripheral edema, weight gain, constipation, dizziness, and somnolence.
(b) Blood levels are not used clinically and no monitoring is needed.
3. Physical methods may provide some temporary relief for central pain at the level of the injury.
a. Transcutaneous electrical nerve stimulation.
b. Warm or cool packs, ultrasound and massage.
4. Surgical treatment should be considered only after conservative therapy has failed.
a. Dorsal root entry zone (DREZ) surgery.
(1) Laminectomy and radiofrequency ablation of DREZ is performed two levels above and one level below the site of injury.
(2) Improvement is realized in 60% to 90% of patients. Best results are achieved in patients with pain at or just below the level of injury.
(3) Complications include loss of one or two sensory levels, CSF leakage, hematoma, and bowel, bladder, and sexual dysfunction.
b. Avoid sympathectomy, rhizotomy, and cordotomy.
5. Narcotic therapy is indicated only after both conservative and surgical therapies have failed.
a. Combination with tricyclic antidepressants may be synergistic.
b. The patient must be carefully selected and carefully supervised.
c. Methadone (Dolophine) sustained release oxycodone (Oxycontin), and an intrathecal morphine pump (if possible) are options for selected patients.
(1) A formal contract detailing expectations and criteria for termination of treatment are made with the patient.
(2) Periodic attempts should be made to wean the medication.
(3) Side effects include sedation and cognitive slowing, respiratory depression, constipation, and reduced sexual function.
SPINAL EPIDURAL ABSCESS
A. Etiology. Epidural abscesses occur in patients with predisposing conditions, such as a chronic disease (alcoholism and immunodeficiency states), a spinal abnormality or intervention, or a source for local or systemic infection. Bacteria seed the epidural space by either contiguous spread or hematogenous dissemination (about half of cases). Methicillin-sensitive Staphylococcus aureus accounts for 40% of cases, Methicillin-resistant S. aureus account for 30% of cases, other gram-positive cocci account for 13% and gram-negative bacteria occur in about 15% of cases.
B. Clinical features. Back pain, fever, and neurologic deficits are the most common symptoms; however, this triad is not often found in all patients. The clinical features are divided into four stages:
1. Back pain at the level of the abscess.
2. Radicular pain from the involved level of the spinal column.
3. Motor weakness, sensory deficit, and bowel and bladder dysfunction.
4. Paralysis.
The rate of progression between stages can vary between a few hours to days.
C. Diagnosis. Two-thirds of patients will have a leukocytosis. The vast majority of patients will also have an elevated erythrocyte sedimentation rate upon presentation. CRP levels are also useful, but processing can take hours to days, which may unnecessarily delay the diagnosis. The initial CRP value is useful for comparison to repeat values as a measure of treatment response. Bacteremia can be detected in up to 60% of cases. However, definitive diagnosis is best established by contrast-enhanced MRI of the affected area.
D. Treatment. Emergent surgical decompression and debridement combined with systemic antibiotics for at least 6 weeks is the treatment of choice. Empiric antibiotic therapy should provide coverage against staphylococci and gram-negative bacilli.
E. Prognosis. Prompt diagnosis and the patient’s neurologic status prior to surgical drainage are the most important predictors of outcome.
DEMYELINATING LESIONS OF THE SPINAL CORD
The most common cause of demyelination in the spinal cord is multiple sclerosis (MS). Up to 50% of cases will involve the spinal cord. The lesions are typically dorsolateral, longitudinal, and flame-shaped (Video 50.1). Another less common cause of demyelination in the spinal cord is neuromyelitis optica (NMO) or Devic’s disease. It is currently recognized as its own distinct disorder, separate from MS. Diagnostic criteria for NMO include optic neuritis, acute myelitis, and at least two of the three following supportive criteria: (1) contiguous spinal cord MRI lesion extending three or more vertebral segments (Fig. 50.2), (2) brain MRI not meeting diagnostic criteria for MS, and (3) NMO-IgG seropositivity. The NMO-IgG antibody has a sensitivity of 74% and a specificity of >90%. Treatment of acute attacks of optic neuritis or myelitis often only partially respond, or do not respond at all to high-dose glucocorticoids. In this setting, plasmapheresis is often used. Maintenance of remission in NMO requires long-term immunosuppressive therapy. There has been evidence for the use of azathioprine, methotrexate, mitoxantrone, mycophenolate mofetil, and rituximab. ![]()
CENTRAL CORD SYNDROME
A. Etiology. Hyperextension injuries may produce a spinal cord contusion primarily affecting the central gray matter. Lamination of tracks in the cervical cord (sacral fibers, lateral; cervical fibers, and medial) explains the clinical signs and symptoms.
B. Clinical features. Patients have “inverted quadriparesis,” in which upper-extremity weakness exceeds lower extremity weakness. Transient burning dysesthesia in the hands with little weakness, or urinary dysfunction can also occur. With recovery, the leg, bladder, and upper-extremity weaknesses improve. The fingers are last to recover.
C. Treatment.
1. Medical management consists of intensive care unit (ICU) care, rigid immobilization of the neck, and physical therapy.
2. Surgical therapy. Surgery is recommended for patients with focal cord compression or instability of the spine. Surgical management for patients without bony injury is a subject of debate in recent literature, and should be decided on a patient to patient basis.
D. Prognosis. Almost all patients have improvement, but often to an incomplete degree among the elderly. Delayed progressive myelopathy can develop in approximately 25% of cases.
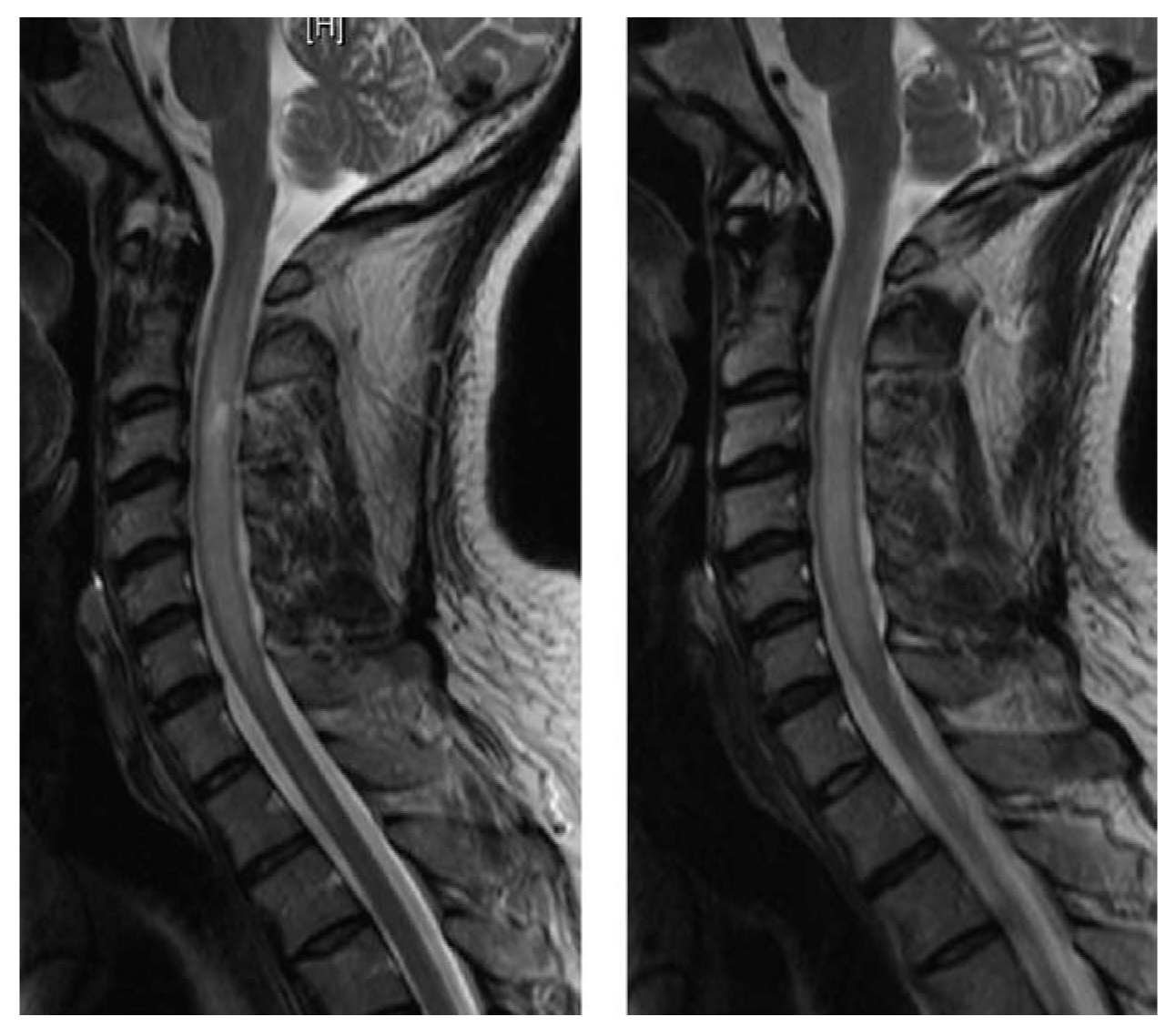
FIGURE 50.2 A 44-year-old African American man with neuromyelitis optica (Devic’s disease). MRI of the cervical spine without and with contrast shows contiguous cord signal abnormality identified involving the cervical spinal cord from the craniocervical junction to the C6–C7 level. The spinal cord signal abnormality involves nearly the entire central spinal cord symmetrically with relative sparing of the lateral portions bilaterally. The cervical spinal cord signal abnormality is associated with tapered cord expansion resulting in circumferential, partial to complete effacement of the thecal sac at the involved levels. (Courtesy of José Biller, MD). MRI, magnetic resonance imaging.
HYPEREXTENSION–FLEXION INJURY (WHIPLASH INJURY)
A. Etiology. Automobile accidents account for approximately 85% of whiplash injuries. The cardinal symptoms of neck pain and headache are musculoskeletal. Concomitant symptoms may include dizziness, visual impairments, nausea, tinnitus, deafness, paresthesias, lower back pain, arm or shoulder pain, posttraumatic stress disorder, and cognitive dysfunction. The roles of mild CNS injury and psychosocial factors are controversial and have led to biopsychosocial models of outcome in the disorder.
B. Prevention. Automobile head restraints reduce flexion–hyperextension motion of the head in automobile accidents, especially during rear-end collisions. However, surveys have shown that the restraints frequently are adjusted incorrectly.
C. Natural history. Rear-end collisions are involved in most whiplash injuries. Cynicism and controversy exist over the cause of chronic whiplash syndrome. Although figures vary widely, approximately 15% to 30% of patients continue to have symptoms 6 months after the injury. By 12 months, 80% of patients have no symptoms, whereas 5% of patients remain severely affected. Results of fluoroscopically guided nerve block studies suggest that zygapophyseal joint pain (usually C2–C3) accounts for 50% of chronic neck pain after whiplash.
D. Treatment. Compensation concerns hinder controlled clinical trials of treatment.
1. Positive attitude and encouragement.
2. Ice for first 24 hours.
3. Muscle relaxants, nonsteroidal anti-inflammatory drugs, and adequate pain relief in the first 7 to 14 days.
4. Resumption of most normal activities together with active therapy or home exercises results in better outcome than with conventional regimens of restricted activity, rest, and soft cervical collar.
5. Heat, ultrasound, massage, and trigger-point injections often make patients more comfortable but remain unproven.
6. Percutaneous radiofrequency neurotomy for cervical zygapophysial joint pain has been showed to be effective in several studies, but the pain frequently returns and necessitates repeated procedures.
SPASTICITY
Spasticity is one of the cardinal manifestations of chronic spinal cord disease. In acute spinal lesions, spasticity develops after a variable period of spinal shock, whereas in disorders with insidious onset, it may be the first symptom noticed.
A. The decision to treat a patient must be made on an individual basis. Treatment is indicated when the advantages of spasticity outweigh the disadvantages. Specific treatment goals need to be formulated.
1. Advantages.
a. Bowel training maintains sphincter tone.
b. “Internal crutches” are available for ambulation.
c. Weight-bearing is possible in transfers.
d. Osteopenia is reduced.
e. Muscle bulk is increased.
f. Venous tone is increased, and deep venous thrombosis may be decreased.
2. Disadvantages.
a. Pain and falls result from paroxysmal spasms.
b. Hygiene is impaired owing to hip adductor spasticity.
c. Joint contractures occur.
d. Pressure sores form.
e. Renal damage occurs because of external sphincter spasticity.
f. Movements required for activities of daily living are impaired or interrupted.
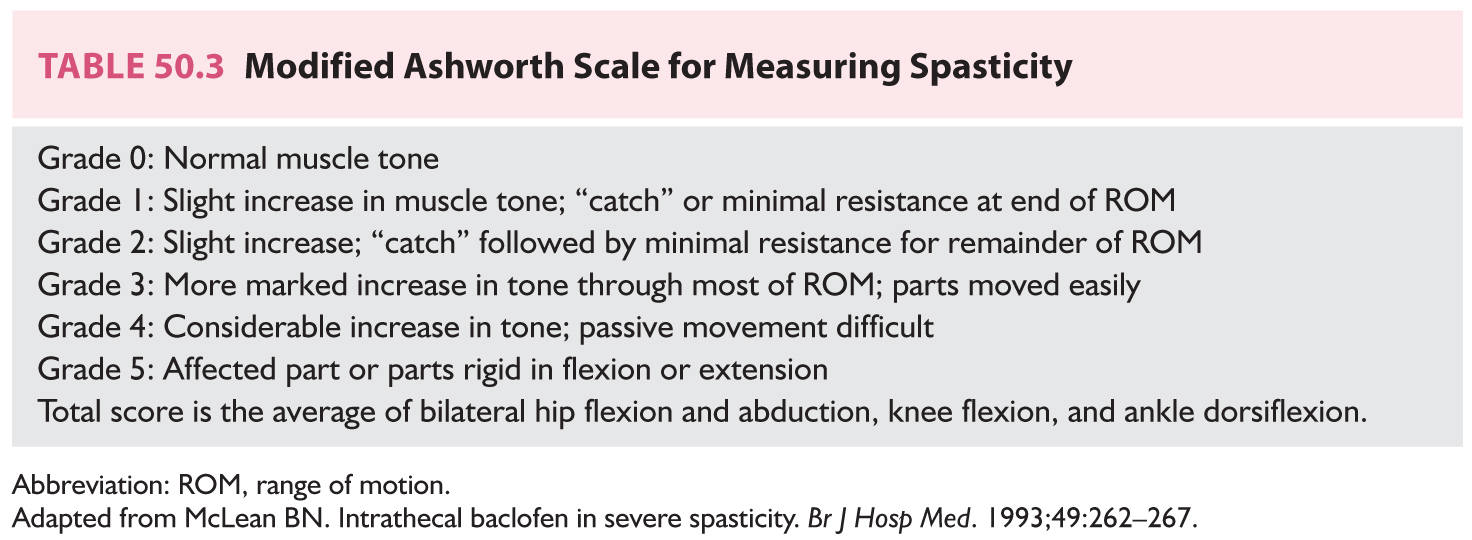
B. Assessment of severity can be made with the modified Ashworth scale (Table 50.3).
C. A changing pattern in a previously stable degree of spasticity should alert the clinician to varying etiologic factors.
1. Medication: fluoxetine, sertraline, or trazodone.
2. Anxiety.
3. Tight clothing or shoes.
4. Inadequate or prolonged postures.
5. Formation of pressure sores.
6. Development of deep venous thrombosis.
7. Ingrown toenails.
9. Fractures.
10. Posttraumatic syringomyelia.
11. Gastrointestinal dysfunction: impaction, hemorrhoids, and acute abdomen.
12. Genitourinary dysfunction: infection, stones, blocked catheters, and disorders of testicle, prostate, vagina, uterus, or ovary.
D. Management is based on a multidisciplinary approach with a rigorous program of both passive and active stretching.
1. Physical modalities.
a. Range of motion and stretching exercises.
b. Heat or cold.
c. Vibration (increases presynaptic spinal inhibition).
d. Splints, casts, and orthotics to prevent contractures and increase mobility.
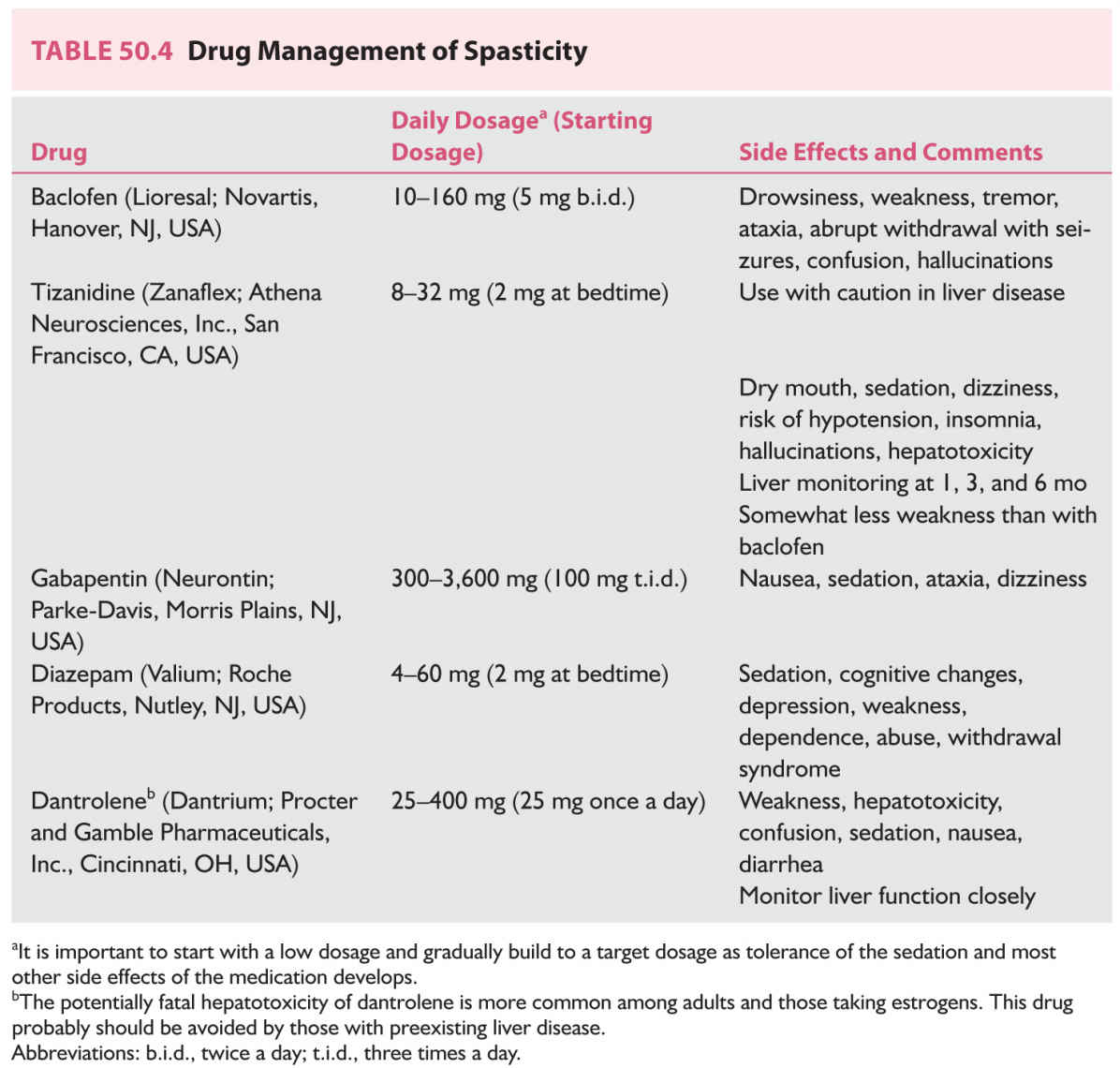
2. Useful medications are summarized in Table 50.4. Muscle relaxants (antispasmodics) are not used in the long-term management of spasticity.
3. Nerve blocks.
Botulinum toxin type A (Botox; Allergan, Irvine, CA, USA) injection has been found effective for focal spasticity at a variety of sites.
a. The discomfort and expense of numerous injections in large lower extremity muscles limit this technique to relatively small muscles.
b. Transient postinjection discomfort and side effects are generally well-tolerated. Excessive weakness and flu-like syndromes may be experienced at initiation of treatment. Botulinum injections should be avoided by patients receiving aminoglycosides. Neutralizing antibodies are more common with larger, more frequent doses.
c. Advantages are reversible block (2 to 6 months) and selectivity toward motor fibers.
d. Disadvantages are expense and need for repeated injections.
4. Neurosurgical procedures.
a. An intrathecal baclofen pump is a safe alternative to ablative surgery for intractable spasticity at experienced centers.
(1) Referral to an experienced center should be considered for patients with stable neurologic disorders accompanied by spasticity seriously interfering with quality of life. Oral agents should have been found ineffective or limited owing to intolerable side effects.
(2) Patients are selected after a test dose of 50 to 75 mg baclofen administered by lumbar puncture. Spasticity is assessed 1, 2, 4, and 8 hours after injection with the modified Ashworth scale (Table 50.3). If two-point improvement is not documented and side effects are tolerable, a second larger test dose (75 to 100 mg) is given the next day.
(3) During the first year after implantation, daily doses generally increase before stabilizing in the range of 300 to 800 mg/day.
(4) Improvement is observed in muscle tone, mobility, and bladder function, and spasms and musculoskeletal pain are relieved. There is little or no relief of central pain.
(5) Systemic side effects are less than with oral therapy. Drowsiness, nausea, hypotension, headache, and weakness may be experienced during the dose titration phase. Infections and catheter or pump complications are rare but potentially serious side effects.
(6) Depletion of the pump battery in 5 to 7 years necessitates replacing the entire pump unit.
(7) Although life-threatening, all instances of drug overdose have been completely reversible. Experience and better pump design have decreased the complication rate to <5%. In early series of patients, surgical revision was needed in 20% of cases for catheter-related problems.
b. Selective posterior rhizotomy with intraoperative EMG selection of lumbosacral rootlets for sectioning is useful in the management of cerebral palsy. Two-thirds of patients’ conditions are improved with minimal sensory loss and few side effects. DREZ operations are functionally similar microsurgical procedures.
c. Percutaneous posterior rhizotomy is technically more difficult, and recurrence may be more of a problem.
d. Efficacy of spinal cord stimulators is controversial.
e. Peripheral neurectomy is occasionally used to relieve specific joint contractures.
f. Longitudinal myelotomy, nonselective posterior rhizotomy, and anterior rhizotomy are rarely performed.
5. Orthopedic procedures are used most often performed in a supportive role to relieve pain, increase mobility, and decrease deformity in cerebral palsy.
a. Tendon release, lengthening, and transfer.
b. Osteotomy and arthrodesis.
Key Points
• Spinal cord disorders can be due to various etiologies: developmental, nutritional, vascular, infectious, demyelinating and traumatic.
• MRI is the preferred method of initial diagnosis in any disorder of the spinal cord. Other testing is then needed on an individual basis, based on clinical judgment.
• Specific treatment should be instituted as soon as the diagnosis has been made.
• In any traumatic spinal cord disorder, it is important to stabilize the spine first.
• In chronic spinal cord disorders, one must manage sequelae appropriately for best patient outcome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree