14 Spinal Navigation
I. Key Points
– Allows intraoperative real-time navigation of instruments relative to the spinal anatomy
– Provides three-dimensional (3D) real-time anatomic information
– May increase the safety, accuracy, and efficiency of certain spine procedures
– Eliminates intraoperative radiation exposure to surgeons and accompanying staff members during procedures
– Provides a versatile array of techniques facilitating the ability to perform complex spine surgery safely
II. Description
Spinal navigation uses computer vision technology to plan and guide surgical interventions. It has evolved from a cumbersome to a more user-friendly system. Early-generation systems required a complex preregistration process through the use of either the paired-point technique or surface mapping. These techniques introduced the potential for error and were time consuming but critical in linking image data to spinal anatomy. Most of the resistance to the universal adoption of image navigation stemmed from such requirements. Newer systems combine high-precision robotics with unparalleled imaging capability, eliminating the need for preregistration. Computer-aided surgery now enables the acquisition of imaging data intraoperatively prior to incision. Current software can use either a 2D or 3D image data set acquired intraoperatively by a fluoroscopy unit or high-resolution computed tomography (CT) scanner. These images are then automatically imported into the computer workstation and used to create a 3D picture of the patient’s anatomy, completing the registration process. This automatic registration process improves the anatomic localization accuracy and eliminates the need for manual point-based or surface-based registration. Subsequently, real-time tracking data are matched with previously obtained image data through the use of a fixed reference point on the patient, computer workstation, and camera system. For spine procedures, affixing the fixed reference frame/point to bone is the initial step in registration.
Components of a Navigation System
After the intraoperative image data are obtained through one of the commercial systems available, this data set is automatically uploaded to the computer workstation. A 3D image is created and linked to your working position relative to the patient’s anatomy through a tracking system. There are currently two types of tracking systems that will triangulate your position in space: optical and electromagnetic (EM). Both systems allow localization of surgical instruments or implants in real time. In electromagnetic tracking an EM field is created, and changes in field are monitored to localize a tracked device. With optical tracking, cameras track instrument positions relative to the fixed reference point through an active or passive method. Active tracking entails the use of light-emitting diodes (LEDs) on the instruments and passive tracking involves the reflection of infrared light from the camera to reflective spheres on instruments. Both systems require a direct line of view between the camera and the tracked instruments to link surgical anatomy to the 3D data set in the computer workstation. The system can then triangulate the instrument’s tip location, angle, and trajectory. The systems are comparable in positioning accuracy and can provide real-time, precise 3D imaging quality (Fig. 14.1).
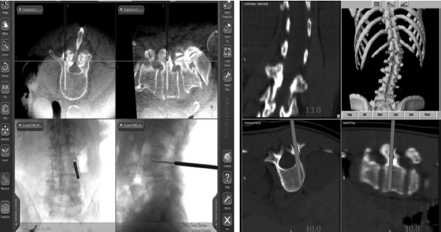
Fig. 14.1 Examples of 3D images with navigation provided by the computer workstation, with a superimposed projection of the navigated instrument or probe.
Applications and Advantages
Image navigation has improved the safety of and ability to perform complex procedures where visibility is not optimal or anatomic deformity is present. Numerous published studies have demonstrated its effectiveness in improving pedicle screw placement for complex multiplanar spinal deformities.1 A meta-analysis of pedicle screw placement accuracy demonstrated a 95% median accuracy with navigation compared with 90% without it.2 It is intuitive that the capability to visualize a pedicle in 3D should minimize screw insertion risks associated with pedicle asymmetry, smaller diameters, and vertebral rotation and thereby prevent nerve root or spinal cord compression. Because of the improved accuracy, operative times have also been shown to decrease with the use of image navigation.3 Drawbacks related to increased operative time, patient registration, and data acquisition are controlled with the current real-time intraoperative data acquisition technology and software systems.3 In addition, mean radiation exposure using image navigation has been shown to be statistically significantly lower compared with conventional fluoroscopy.4
Aside from pedicle screw insertion, many other versatile applications are being described for image navigation, including C1-C2 transarticular and percutaneous translaminar facet screw placement, lumbar disc arthroplasty placement, and balloon kyphoplasty. These possibilities are incorporating the advantages of image navigation and demonstrating feasibility, accuracy, and operative time reduction while reducing radiation exposure.
III. Surgical Pearls
– All staff using the system should be properly trained, to prevent errors that can lead to improper setup, inaccurate information, and surgical complications.
– The fixed referenced frame must not be inadvertently bumped, moved, or altered. This can lead to tracking and positional errors during navigation. It’s important to keep the reference frame close to the surgical field for maximum accuracy.
– Spinal navigation is not a substitute for fundamental knowledge of anatomic landmarks and appropriate surgical technique. Improper use or malfunction of the system can cause navigational inaccuracies.
– Image navigation should be used to confirm anatomic landmarks and suspected locations and trajectories for hardware placement.
– The room setup plan should provide for a direct line of view between navigation components (camera, computer workstation, and reference frame).
Common Clinical Questions
1. Which of the following is not a feature of spinal image navigation?
A. Real-time views
B. Decreased operative time
C. Axial views
D. Increased radiation exposure
E. Improved accuracy
2. Current spinal image navigation systems provide real-time tracking through what technique?
A. Paired-point preregistration
B. Surface mapping preregistration
C. Continuous fluoroscopic imaging
D. Optical or electromagnetic tracking
E. None of the above
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







