13 Spinal Radiation Therapy
I. Key Points
– Conventional fractionated radiotherapy, defined as radiation delivered in one to two radiation beams without high precision or highly conformal techniques, is well established and widely accepted as an appropriate treatment modality for many spinal tumors.
– Stereotactic spinal radiosurgery allows for the highly conformal delivery of radiation to spinal lesions and avoids toxicity to normal tissues.
– Spinal radiosurgery has proven effective in the treatment of benign and malignant lesions along the entire length of the spine.
II. Description
Epidemiology
– Over 200,000 cases of spinal tumors are diagnosed yearly in North America.1
– Up to 40% of cancer patients will develop metastatic disease of the vertebrae.
– In approximately 20% of patients, spinal metastases will progress to neural element compression.
– With improved multimodality approaches for cancer treatment and greater long-term survival, the incidence and prevalence of spinal metastases are likely to increase.
Overview
– The traditional therapy for spinal tumors, primary or metastatic, includes open surgical excision, systemic chemotherapy, and conventional fractionated radiation therapy, alone or in combinations.
– In a randomized trial comparing conventional radiation therapy alone to surgery followed by radiation therapy for the treatment of spinal metastases causing spinal cord compression, Patchell and colleagues demonstrated that surgery combined with conventional radiation therapy is a superior treatment in its ability to preserve ambulation and decreases the need for both corticosteroids and opioid analgesics.2
– With conventional radiation therapy, one or two low-precision radiation beams are delivered to the spine over several fractions to allow for repair of the normal tissues.
– The goals of local radiation therapy have been palliation of pain, prevention of local disease progression and subsequent pathologic fractures, and halting progression of, or reversing, neurologic compromise.
– Conventional radiation therapy is limited in its effectiveness by the relative intolerance of the adjacent normal tissues (e.g., the spinal cord, nerve roots, and conus medullaris) to high radiation doses. Thus, treatment doses are limited to subtherapeutic levels, resulting in disease recurrence or progression.
– Stereotactic spinal radiosurgery is the delivery of a highly conformal, large radiation dose to a specific target, often in a single fraction (Fig. 13.1A,B).
– Radiosurgery offers the advantages of applying radiobiologically effective doses to a target and sparing surrounding structures.
– Intensity-modulated radiation therapy is a technology that provides the ability to vary the integrated intensities of radiation beams for the delivery of therapy. With several radiation beams all passing through multileaf collimators with different apertures, the intensity of the radiation dosing can be shaped in three-dimensional space.
Conventional Radiotherapy
– Three randomized trials have been published for spine metastases.3
– Approximately 70% of patients remained ambulatory after conventional radiation therapy for epidural spinal cord compression.
– Between 20 and 60% of patients regained ambulation after conventional radiotherapy.
– Pain is palliated in 50 to 70% of patients.
– The most commonly used treatment is 30 Gy delivered in 10 fractions.
– The specific dose-fractionation schedule used has not been found to have a significant impact on ambulatory status or the probability of regaining ambulation.4
– Local control rates for spine metastases with conventional radiotherapy are reported to be 60 to 90%.
– The effectiveness of conventional radiotherapy has been limited by the intolerance of the spinal cord to high-dose radiation.
– Certain histologies such as sarcomas, melanoma, and renal cell carcinoma are known to be relatively resistant to conventional radiotherapy doses.
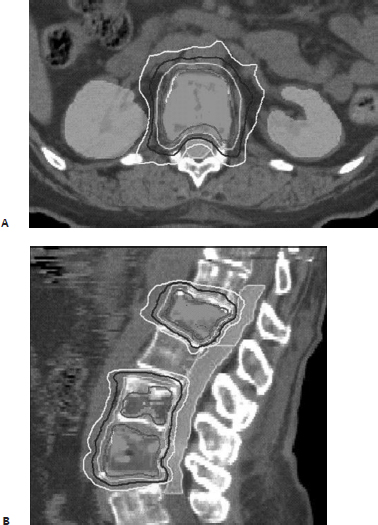
Fig. 13.1 (A,B) Case example of a 54-year-old woman with symptomatic progression on magnetic resonance image (MRI) of L1 and L4 breast metastases after prior conventional irradiation treatment. She complained of significant mechanical back pain upon ambulation. She first underwent a percutaneous cement augmentation procedure followed by radiosurgery. The prescribed dose to the planned tumor volume was 16 Gy using 9 coplanar beams (Synergy S, Elekta, Atlanta, GA). Axial and sagittal images of the treatment plan are presented.
Radiosurgery
– No randomized data are available to date.
– Reported outcomes demonstrate 85 to 100% of patients experiencing palliation of pain.5
– Use of both single fraction doses (16 to 24 Gy × 1) and hypofractionation (4 Gy × 4, 6 Gy × 5, 8 Gy × 3, 9 Gy × 3) has been reported.
– Significant toxicity does not appear to be associated with any fractionation schedule.6
– The majority of reported local control rates are around 90%.
Spine Radiosurgery: Two Fundamental Principles
– Target immobilization
• Early spinal radiosurgery protocols applied an approach similar to that of cranial radiosurgery through the application of an invasive rigid frame directly to the spine.
• Frameless techniques have become the methodology of choice because of their relative noninvasiveness.
• Perfect static positioning cannot be accomplished using frameless methods; thus pre- and intratreatment imaging must be obtained to account for target movement due to respiration.
– Target localization
• Frequent acquisition of localizing images during the delivery of radiation combined with adjustments to the patient’s position allow for accurate targeting of the desired lesion(s).
• Volumetric imaging allows for the detection of rotational errors in patient setup, making robust automatic registration procedures possible.
• Cone beam imaging uses gantry-mounted kilovolt sources and detectors to acquire images during gantry rotation. The images are converted to computed tomography (CT)–like axial slices, yielding high spatial resolution and resulting in submillimeter targeting errors.
Indications for Treatment with Spinal Radiosurgery
– Pain from spinal tumors
– Primary treatment modality for newly discovered spinal metastases instead of open surgery or conventional radiation therapy
– Radiation boost for radioresistant tumors
– Progressive neurological deficit
• May need to perform decompressive/debulking surgery for patients with progressive myelopathy (instead of using radiation treatment)
– Treatment of residual tumor after surgery
– Postsurgical tumor progression
Candidate Lesions for Spinal Radiosurgery
– Lesions associated with minimal spinal cord compromise
– Previously irradiated lesions
– Radioresistant lesions that would benefit from a radiosurgical boost
– Residual tumor following surgery
– Recurrent tumor after prior surgical resection
– Lesions requiring difficult or morbid surgical approaches
– Short life expectancy of patient, precluding open surgery
– Significant medical comorbidities precluding open surgery
– Lesions not involving overt spinal instability
III. Surgical Pearls
– Conventional radiotherapy is safe and effective, with good symptomatic response and local control of spine tumors, particularly for radiosensitive histologies, such as lymphoma, myeloma, and seminoma.
– Conventional radiotherapy is an appropriate initial therapy option for spine tumors where no contraindication exists. Contraindications include spinal instability, prior irradiation, radioresistant histology, and high-grade spinal cord compression.
• Consider surgical decompression/debulking/instrumented stabilization procedures for cases where radiotherapy is contraindicated.
– Radiosurgery is safe and effective, with durable symptomatic response and local control for even radioresistant histologies, regardless of prior fractionated radiotherapy.
– Radiosurgery should be preferred over conventional radiotherapy for the treatment of solid-tumor spine metastases in the setting of oligometastatic disease or radioresistant histology.
– Single-fraction, highly conformal large-dose radiosurgical treatments offer excellent tumor control, symptomatic relief, and patient convenience.
Common Clinical Questions
1. What is the major factor limiting the effectiveness of conventional radiotherapy for the treatment of spine tumors?
A. The relative resistance of the spinal cord to high-dose radiation
B. The intolerance of the spinal cord to high-dose radiation
C. The resistance of tumors of the spine to even high doses of radiation
D. The instability of the spine that develops after conventional radiotherapy treatment
2. Which of the following statements is true?
A. The most commonly used radiation dose prescription for the treatment of spine metastases is 20 Gy in 10 fractions.
B. Randomized clinical trials have demonstrated the superiority of radiosurgery over conventional fractionated radiotherapy for the treatment of spine tumors.
C. Certain histologies such as myeloma and lymphoma are known to be relatively resistant to radiation therapy.
D. Reported outcomes demonstrate that 85 to 100% of patients experiencing pain from spine metastases report improvement after radiosurgery.
3. Radiosurgery should be considered as a first-line treatment for a spine tumor over conventional radiotherapy in which setting?
A. In the setting of gross spinal instability
B. When the lesion has already undergone treatment using fractionated radiotherapy with spinal cord tolerance doses
C. For lymphoma, myeloma, or seminoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







