CHAPTER 262 Stereotactic Radiosurgery for the Treatment of Spinal Metastases
Metastatic spine disease represents a significant source of morbidity in the cancer population. Therapy is aimed at reducing pain, maintaining or improving neurological status, stabilizing the spine, and achieving local tumor control. Traditionally, the principal modalities used to treat spinal metastases are radiation therapy and surgery, although hormonal therapy, immunotherapy, and chemotherapy are playing increasingly large roles for selected tumors. The wide application of technologic advances in both surgery and radiation therapy over the past 5 years has improved patient outcomes. Surgical advances include the application of posterolateral approaches to the spine,1 pedicle screw fixation, and percutaneous augmentation of the vertebral body with cement.2,3 However, the biggest advance has been the development of high-dose conformal photon radiation therapy, which can deliver cytotoxic tumoral doses while sparing normal tissue tolerance, particularly the spinal cord, kidney, and bowel. Because of the steep dose gradient, radiation techniques such as image-guided intensity modulation radiotherapy can deliver high-dose radiation within millimeters of the spinal cord. For spinal metastases, radiation can be delivered as stereotactic radiosurgery (SRS), which is given as a single fraction in doses commonly 10 to 24 Gy.4–6 Hypofractionated radiation therapy or stereotactic body radiation therapy (SBRT) is often delivered in doses of 24 to 30 Gy at 6 to 9 Gy per fraction.7,8 The greatest utility of SRS and SBRT is their ability to treat tumors that are traditionally considered resistant to conventional external beam radiation therapy (cEBRT), such as 24 to 50 Gy at 1.8 to 3 Gy per fraction. A number of published clinical series have shown long-term, durable local tumor control in excess of 15 months for radioresistant tumors when using SRS or SBRT as primary treatment, for reirradiation after failed cEBRT, or as adjuvant therapy postoperatively or after percutaneous cement augmentation.4,5,9–12 Delivery of high-dose photon therapy represents a major advance in the treatment of metastatic spinal tumors in terms of both local tumor and pain control. Additional advantages include shorter treatment times and less soft tissue toxicity than seen with cEBRT.
Conventional External Beam Radiation Therapy
Traditionally, spine tumors have been irradiated with cEBRT at doses of 30 to 50 Gy in fractions of 1.8 to 3 Gy. cEBRT provides a safe therapeutic window to irradiate the spinal cord and surrounding radiosensitive structures, but the response of the tumor is dependent on histology. Conventional fractionation schemes provide durable tumor and pain control for hematologic malignancies such as multiple myeloma and lymphoma and for solid tumors such as breast and prostate carcinoma, but they often fail to control radioresistant solid tumors such as sarcoma, melanoma, renal cell carcinoma, non–small cell lung cancer, and colon carcinoma. Maranzano and Latini presented a prospective trial of 275 consecutive patients undergoing 30-Gy radiation with two different conventional fractionation schedules for metastatic epidural spinal cord compression (ESCC).13 Twenty patients underwent initial surgery for gross spinal instability followed by radiation therapy, and 255 underwent radiation therapy alone. Patients were excluded from analysis for early death (10%) or failure to initiate steroids at the time of radiation therapy (8%) for a total of 205 evaluable patients. Significant relief of biologic pain was achieved in only 70% of patients. Overall, 89% of pretreatment ambulatory patients maintained ambulation, whereas just 60% regained ambulation. In the group that recovered ambulation, 70% had radiosensitive tumor histologies, but radioresistant histologies responded poorly. For example, breast carcinoma had an 80% response rate versus a 20% rate for hepatocellular carcinoma. Additionally, patients with favorable tumor histology had a more durable response of 10 to 16 months, in contrast to unfavorable tumors, which had a response lasting just 1 to 3 months. Similarly, a retrospective analysis from Nagoya University reported the result of 101 patients treated for spinal metastases; 95% of patients received 40-Gy cEBRT at 2 Gy per fraction.14 The cumulative survival rate was 45% at 1 year, but only 20% showed durable pain relief.
Patchell and colleagues also demonstrated lack of response to cEBRT in a prospective cohort study comparing surgery followed by cEBRT with cEBRT alone in myelopathic patients with solid tumor metastases.15 Patients with hematologic malignancies were excluded because of the known radiosensitivity. Surgery followed by cEBRT was significantly better in terms of maintenance and recovery of ambulation, continence, narcotic requirements, and survival. Of the patients who recovered ambulation, 9 of 16 in the surgery group did so but only 3 of 16 in the cEBRT group. All 3 who recovered in the radiation arm crossed over to the surgical arm in keeping with the intention-to-treat paradigm. In this study, no patient regained ambulation with radiation therapy alone. In patients who can tolerate surgery and have a predicted meaningful survival, surgery is the treatment of choice for solid tumors causing high-grade ESCC or myelopathy (or both). This is predicated on the failure of solid tumors to respond to cEBRT.
Stereotactic Radiosurgery
Classic radiobiology teaches that ionizing radiation kills tumor by creating double-stranded breaks in DNA.16 Mitotic cell death is dependent on the biologic effective dose, which is predicted by the linear quadratic model and is dependent on the dose per fraction, number of fractions, and response to therapy denoted as the α/β ratio. Based on the linear quadratic equation, radioresistant tumors are predicted to respond better to radiation given at higher dose per fraction. Although cell killing is primarily dependent on disruption of mitosis, additional factors may affect tumor response, such as apoptosis and damage to stromal cells. Experimental evidence suggests that high-dose single-fraction radiation therapy greater than 8 to 10 Gy activates the acid sphingomyelinase pathway and causes endothelial apoptosis and disruption of blood vessels.17
From a radiation biology standpoint, increasing the dose per fraction increases the biologic effective dose, particularly in the treatment of radioresistant tumors. This observation is underscored in the treatment of intracranial metastases with SRS (18 to 24 Gy), which has demonstrated 85% local control rates at 1 year.18 A large experience exists in treatment of intracranial metastases with SRS, but recent technologic advances have enabled the delivery of SRS to large, irregularly shaped spinal tumors within millimeters of the spinal cord. Photon delivery of cytotoxic tumoral doses within normal tissue tolerance is accomplished by using micromultileaf collimation with inverse treatment planning to deliver image-guided intensity modulation radiotherapy or by using robotic technology to guide the photon beams. A number of devices have been developed to immobilize patients and provide image-guided patient setup and isocenter verification.
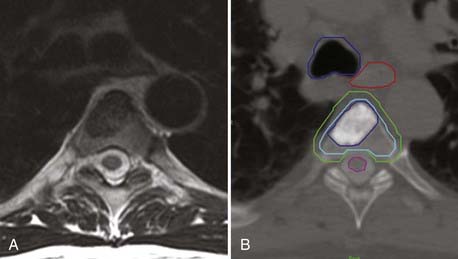
In terms of tumor delineation, the gross tumor volume (GTV) is contoured to precisely identify the tumor that is visualized on MRI and CT. The best images to identify bone tumors are the T1-weighted and T2-STIR (short tau inversion recovery) sagittal images, in which bone tumor is hypointense or hyperintense, respectively. Tumor has variable intensity on T2-weighted images, which is not useful for tumor delineation; however, T2-weighted axial images provide the best assessment of spinal canal impingement and spinal cord compression. From the GTV contour, a clinical target volume (CTV) is drawn to account for microscopic disease outside the defined GTV. As opposed to brain metastases, vertebral body tumors are thought to have an infiltrative penumbra through the entire bone. If the GTV involves a small portion of the vertebral body, the CTV will be defined as the entire vertebral body. The CTV is then extended to define the planning target volume (PTV) to account for uncertainties in setup and delivery and is the actual volume that receives treatment. The PTV is a 2- to 4-mm expansion of the CTV with care taken to not transgress the spinal cord contour based on CT myelography. The PTV is the volume that is treated, although by using dose painting, one can give an additional boost to the GTV or CTV (Fig. 262-1).
Dose escalation to treat spinal metastases has been limited by knowledge of spinal cord tolerance. Spinal cord toxicity is related to the absolute dose, fractionation schedule, and length of spinal cord irradiated. Although not well defined, the toxic dose at which myelopathy develops in 5% of patients at 5 years (TD5/5) is thought to be 50 Gy for a 5- to 10-cm length of spinal cord with conventional fractionation of 1.8 to 2 Gy.19 The Northeast Proton facility reported acceptable toxicity when delivering 60 Gy to the surface of the spinal cord and 56 Gy to the central area via mixed photon and proton beam therapy in conventional fractions.20
The TD5/5 with SRS or SBRT is unknown, but careful dose escalation has provided safe parameters.4 Hypofractionated radiation therapy consisting of 10.4 to 24 Gy at 3.7 to 7 Gy per fraction with treatment of a 1.6-cm3 volume of the spinal cord caused no morbidity at 2 years’ follow-up.19,21 For high-dose single-fraction radiation therapy, the dose to the spinal cord has been defined either as the maximal dose to a single voxel on the spinal cord (cord Dmax) or as the percentage of spinal cord irradiated. Cord Dmax is currently defined at Memorial Sloan-Kettering Cancer Center as 14 Gy to the spinal cord or 16 Gy to the cauda equina. No toxicity was encountered at this dose.4 Ryu and coauthors reported a median dose of 9.8 Gy to 10% of the spinal cord and encountered 1 case of radiation myelopathy in 230 lesions treated.22
Stereotactic Radiosurgery in Current Treatment Paradigms
High-dose single-fraction radiation therapy has been very effective in providing palliation for metastatic spinal tumors, especially radioresistant tumors, either as initial therapy or after failure of cEBRT. In most series, exclusion criteria for SRS include high-grade ESCC from radioresistant tumors and spinal instability.23 The potential morbidity from treating high-grade ESCC with SRS relates to spinal cord tolerance. To avoid radiation myelopathy, one would have to underdose at the margin of the spinal cord and thereby risk progression at the site demanding the highest degree of tumor control. Conversely, delivering a cytotoxic dose to the margin of the dura risks spinal cord injury. For this reason, in accordance with data from Patchell and colleagues,15 resection of high-grade ESCC and myelopathy in solid tumors is recommended rather than treating with SRS or SBRT. The change in treatment paradigms involves the use of SRS as a postoperative adjuvant to gain local control with radioresistant tumors, as opposed to cEBRT.
The second surgical indication is spinal instability. This is broadly defined as movement-related pain, in contradistinction to biologic pain, which is night or morning pain that resolves with steroids and frequently with radiation therapy. Symptoms of spinal instability are dependent on the level of spinal involvement.23 Patients manifest cervical spine instability in flexion-extension. Patients with occipitocervical tumors additionally demonstrate pain with lateral rotation of the head, often in association with occipital neuralgia. Counterintuitively, thoracic instability is often worse in recumbency because patients straighten an unstable kyphosis. Finally, lumbar instability is often manifested as mechanical radiculopathy or severe radicular pain on axial loading. Radiographic criteria in the occipitocervical spine include fracture subluxation greater than 5 mm or 3.5-mm subluxation with 11-degree angulation. In the subaxial cervical and thoracic spine, most instability is seen with a burst or compression fracture and extension into a unilateral joint. Finally, lumbar mechanical radiculopathy is seen with a burst or compression fracture and extension into the neural foramen or joint. Although these patients often require surgery, percutaneous cement augmentation (i.e., vertebroplasty or kyphoplasty) is now being used successfully in patients with burst or compression fractures who have axial load pain in the absence of gross instability.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree