INTRODUCTION
“Normal human consciousness consists of a serially, time-ordered, organized, restricted, and reflective awareness of self and the environment. Moreover, it is an experience of graded complexity and quantity.” Schiff and Plum, J Clin Neurophys, 2000.
Philosophical and religious frameworks may influence definitions of consciousness. Consciousness is classically defined as awareness of self and the environment and requires both arousal (i.e., wakefulness) and cognitive content (i.e., thoughts and perceptions).
Coma is a state of unconsciousness that differs from sleep in that it represents a neurologic deficit and is not readily reversed. Cerebral oxygen uptake (cerebral metabolic rate of oxygen [CMRO2]) is normal in sleep, and brain electrical activity progresses thorough organized stages of synchronized activity on electroencephalography (EEG). In coma, CMRO2 is abnormally reduced and EEG activity progressively slows and becomes attenuated, with loss of normal reactivity to sensory stimuli.
NEUROANATOMY
Confusional state and delirium are terms that refer to a state of inattentiveness, altered cognitive content, and sometimes hyperactivity, rather than to a decreased level of arousal; these conditions may presage or alternate with obtundation, stupor, or coma.
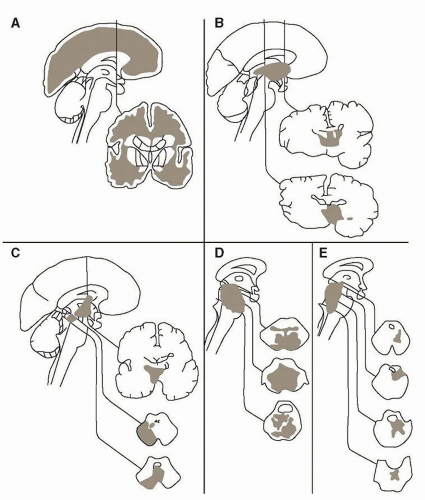
The anatomic substrate of consciousness lies within the reticular activating system, thalamus, and cerebral cortex. Location for classic structural brain lesions associated with stupor and coma have been derived from lesion studies and more recently confirmed and expanded based on structural and functional brain imaging studies such as diffusion tensor and resting state magnetic resonance imaging (MRI) (
Fig. 18.1).
MANAGEMENT STRATEGY
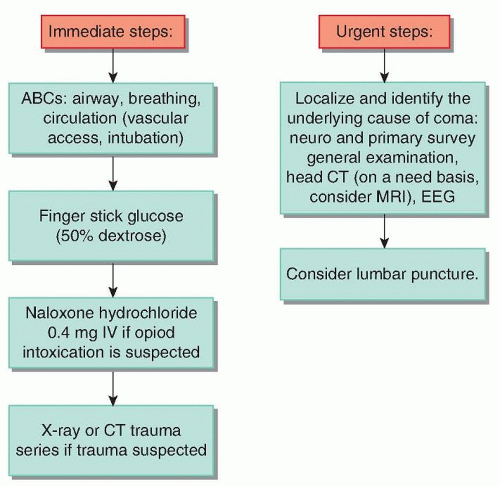
A suggested algorithm for the initial management of new-onset coma is shown in
Figure 18.2.
INITIAL RESUSCITATION
Initial management of the comatose patient should always focus on the ABCs: airway, breathing, and circulation. Assuring a patent airway, securing adequate ventilation, and restoring or maintaining circulation should take precedence, as it does with any critically ill patient. Vascular access needs to be obtained as soon as possible and may include central venous access and large bore peripheral access. Detection and treatment of immediately life-threatening systemic conditions may include stopping a hemorrhage; supporting the circulation by administration of fluids, blood products, or pressors; intubation when necessary (e.g., to prevent aspiration in a patient who is vomiting); and obtaining an electrocardiogram to detect dangerous arrhythmias. Fingerstick glucose should be obtained immediately and if in doubt, 50% dextrose should be given intravenously with parenteral thiamine. (Administering glucose alone to a thiamine-deficient patient can precipitate Wernicke-Korsakoff syndrome.) When opiate overdose is a possibility, naloxone hydrochloride (Narcan) 0.4 mg IV is given. If trauma is suspected, damage to internal organs and cervical fracture should be assumed until radiographs determine otherwise and emergency ultrasound scanning (i.e., focused assessment with sonography for trauma [FAST]) or other imaging has ruled out major internal bleeding or organ injury.