Surgery for Ossification of the Posterior Longitudinal Ligament: Dorsal Approach
Morio Matsumoto
Yoshiaki Toyama
Kazuhiro Chiba
Ossification of the posterior longitudinal ligament (OPLL) compresses the ventral or ventrolateral aspects of the spinal cord as it progresses, causing progressive cervical myelopathy. Patients with symptomatic OPLL present with various myelopathic symptoms including numbness in the hands, hand clumsiness, walking disability, and bladder and bowel dysfunction. They usually require surgery rather than conservative treatment.
Although it makes sense for surgeons to directly decompress the spinal cord via a ventral approach, indirect decompression using a posterior approach is widely used for the treatment of OPLL. Advocates of a posterior strategy for the treatment of OPLL have claimed that, compared with the ventral approach, the dorsal approach is less technically demanding; that it is less frequently associated with serious complications such as intraoperative neural injury and symptomatic cerebrospinal fluid leakage, the dislodgement of grafts, and adjacent segment disease; and that the posterior approach is more applicable to multisegmental lesions, as is often the case with OPLL patients (1, 2, 3, 4, 5 and 6).
Dorsal procedures include a laminectomy with/without fusion and a laminoplasty. A laminectomy-alone strategy is rarely utilized for OPLL because OPLL is known to progress even after a laminectomy alone, potentially resulting in the recurrence and deterioration of neurologic symptoms (1). Therefore, a laminoplasty and a laminectomy with fusion are the currently accepted posterior surgical procedures for OPLL. The optimal dorsal surgical method, that is, laminoplasty versus laminectomy with fusion, remains controversial and is discussed in Chapter 131.
The authors favor laminoplasty as the treatment of choice for OPLL. Currently, two types of laminoplasty are widely used: an open-door type and a double-door type (1,6,7). No significant differences in surgical outcomes have been reported between these two surgical procedures to date, and either of the procedures can be selected according to the surgeon’s preference.
INDICATIONS FOR LAMINOPLASTY
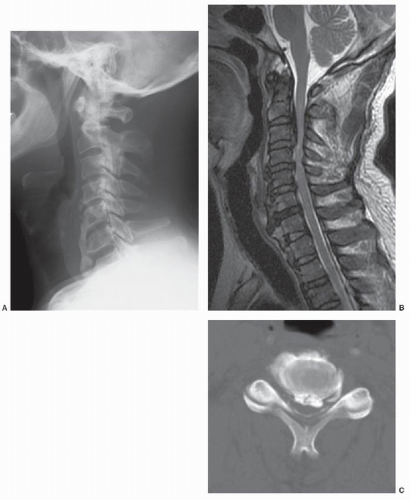
A laminoplasty may be indicated for the majority of patients with OPLL-induced cervical myelopathy. The best candidates for laminoplasty are patients with multisegmental OPLL and a developmentally narrow spinal canal who do not exhibit significant kyphosis of the cervical spine (Figs. 82.1 and 82.1 and 82.2). Patients with single-level segmental OPLL, without developmental cervical canal stenosis, may be better candidates for ventral surgery rather than for laminoplasty.
Several authors have reported factors that limit the indications for laminoplasty for OPLL. Yamazaki et al. (8) analyzed postoperative MRI images for 38 patients who underwent laminoplasty via midsagittal splitting for OPLL and found that the spinal cord was not free of the ossified lesion even after posterior decompression in 23 patients. They identified risk factors for suboptimal decompression as including lordosis of less than 10 degrees or kyphosis in the preoperative sagittal alignment and a preoperative maximal ossification thickness of more than 7 mm. Meanwhile, Suda et al. evaluated the effects of cervical alignment on the surgical results for expansive laminoplasty (ELAP) in 114 patients with cervical spondylotic myelopathy. They found that patients with local kyphosis exceeding 13 degrees showed a poorer recovery of myelopathy and recommended ELAP for patients with local kyphosis of less than 13 degrees (9).
Fujiyoshi et al. reported a new index, the K-line, which was defined as a line that connects the midpoints of the spinal canal at C2 and C7 (Fig. 82.3). They tried to evaluate the kyphotic alignment of the cervical spine and canal compromise as a result of OPLL simultaneously using the K-line (10). They found that a sufficient dorsal shift in the spinal cord and neurologic improvement was not obtained after dorsal decompression surgery in patients with OPLL that did not exceed the K-line (the K-line (-) group).
Iwasaki et al. (11) conducted a retrospective study of 66 patients who underwent laminoplasty for the treatment of
cervical myelopathy arising from OPLL (mean follow-up, 10.2 years). They found that the surgical outcome was significantly poorer in patients with an occupying ratio of OPLL in the spinal canal greater than 60% and that the most significant predictor of a poor outcome of laminoplasty was a hill-shaped (not sharp) ossification, followed by a lower preoperative Japanese Orthopaedic Association (JOA) score, a postoperative change in cervical alignment, and an older age at the time of surgery. They concluded that laminoplasty was effective and safe for patients with an occupying ratio of OPLL less than 60% and plateaushaped ossification.
cervical myelopathy arising from OPLL (mean follow-up, 10.2 years). They found that the surgical outcome was significantly poorer in patients with an occupying ratio of OPLL in the spinal canal greater than 60% and that the most significant predictor of a poor outcome of laminoplasty was a hill-shaped (not sharp) ossification, followed by a lower preoperative Japanese Orthopaedic Association (JOA) score, a postoperative change in cervical alignment, and an older age at the time of surgery. They concluded that laminoplasty was effective and safe for patients with an occupying ratio of OPLL less than 60% and plateaushaped ossification.
Matsumoto et al. (12) recently reported that patients with preoperative kyphosis tended to develop closure of the expanded laminae after surgery, potentially leading to the later deterioration of neurologic symptoms (Fig. 82.4 and 82.4). Thus, the indications for laminoplasty in patients with marked preoperative kyphosis and/or a large OPLL with spinal canal compromise of more than 60% may not be expected to respond favorably to a laminoplasty procedure. For patients with marked preoperative kyphosis, a ventral approach alone or in combination with a laminoplasty should be considered; alternatively, dorsal decompression with an instrumented fusion using pedicle screws or lateral mass screws may be indicated (Fig. 82.5).
SURGICAL PROCEDURES
The authors prefer to perform an open-door laminoplasty, as developed by Hirabayashi (Fig. 82.6 and 82.6) with some modifications (1,4,13). The patient is placed in a prone position on a surgical table with the head fixed using a Mayfield device. The table is tilted cranially upward at an angle of 20 to 30 degrees. A midline incision is made between C2 and T1 if the laminoplasty is to be conducted from C3 to C7. The paravertebral muscles are divided through the midline along the nuchal ligament and down to the spinous processes. Leaving the attachment of the semispinalis cervicis muscle to the tips of the C2 spinous process, the tips of the spinous processes from C3 to C7 are detached. If the canal compromise by the OPLL is not so remarkable at C6-C7, detachment of the muscles and ligament from the C7 spinous process should be avoided to prevent the development of postoperative axial symptoms. Instead of opening the C7 lamina, the rostral half of the C7 lamina is removed to decompress the C6-C7 segment. Bilateral paracervical muscles are then stripped from the laminae using a Cobb elevator and electric cautery, leaving the interspinous ligaments and muscles intact. Bleeding from the muscles should be meticulously stopped using a bipolar coagulator.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree