Surgery for Ossification of the Posterior Longitudinal Ligament: Ventral Approach
Atsushi Okawa
Makoto Takahashi
Kenichiro Sakai
Kenichi Shinomiya
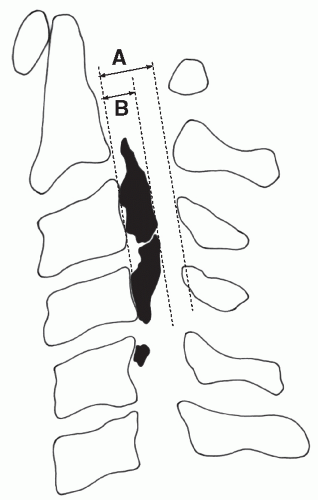
As ossification of the posterior longitudinal ligament (OPLL) of the cervical spine develops, the cervical spinal cord is compressed ventrally, resulting in myelopathy. Dorsal surgery can relieve the compression of the spinal cord that results from extensive OPLL, but there is a limitation. In particular, laminoplasty does not always produce the expected space for a locally protruded OPLL, which is similar to a beak and causes a highly narrowed spinal canal (a canal narrowing ratio [CNR] >60%, Fig. 81.1) (1).
The technique of corpectomy and floating of the ossification of the OPLL can provide an immediate decompression effect to the spinal cord. In this method, ossified ligaments are cut very thin and allowed to float away from the dural sac without removal. This method is a rational way to enlarge the narrowed spinal canal while at the same time restoring the spinal cord to its original place and shape (Fig. 81.2).
Yamaura introduced the floating method for multisegmental and continuous OPLL to minimize surgical invasion and the risk of hemorrhage from the epidural venous plexus while simultaneously avoiding too close an approach to the spinal cord, which would risk neural damage (2,3). This method can decrease the risk of localized acute spinal cord swelling and leakage of cerebrospinal fluid. Long-term follow-up has shown that the remnant of the ossification stops growing after anterior flotation (3). In this chapter, the technique of the ventral floating method and the longterm results of the procedure are demonstrated.
OPERATIVE INDICATION
The operative indication is cervical myelopathy resulting from OPLL in a patient, for which conservative management provides little to no improvement. Access to the C2 vertebral body, down to the T1 vertebra, can be achieved without sternum resection. With the ventral method, there is no particular limitation regarding the degree of the narrowing ratio. The procedure is especially useful in cases with extensive adhesions to the ventral surface of the dura mater and widespread dural ossification (i.e., in cases presenting with a high ratio of narrowing exceeding 60% to 70%). The ventral method is more appropriate for cases of the continuous or mixed type of ossification (4) as well as for cases with kyphotic curvature in the cervical spine. A high degree of localized, continuous, or mixed-type ossification, in which the spinal cord is severely compressed ventrally, constitutes a solid indication for the ventral floating method, because the spinal cord alignment of this disease is considered to be kyphotic (5).
PREOPERATIVE PREPARATION
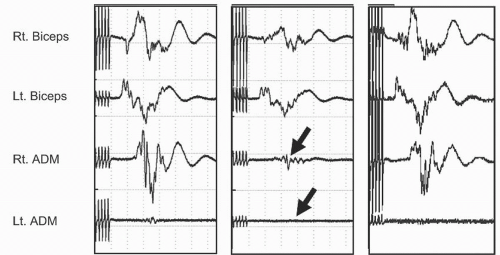
The general condition of the patient should be thoroughly assessed, as preoperative latent disorders may become symptomatic postoperatively. In particular, impaired respiratory function is crucial because the retropharyngeal space is enlarged after surgery, which may result in respiratory disturbance. Although smoking cessation at least 4 weeks before surgery has proved to reduce the occurrence of perioperative respiratory and wound complications (6), the authors believe that patients should quit smoking by all means no later than 3 months before ventral cervical surgery. Smoking also delays bone union. Glucose intolerance should be checked, as OPLL patients have a tendency toward diabetes mellitus. It is necessary for all disorders to be controlled prior to surgery. Additionally, assessing the presence of provocation of symptoms (e.g., radiating pain to the arm in an extension position) preoperatively is an important test. It provides, when present, an indication that the patient is at risk for neural injury during surgery due to incorrect positioning of the neck. Spinal monitoring may also be used (Fig. 81.3).
OPERATION DESIGN
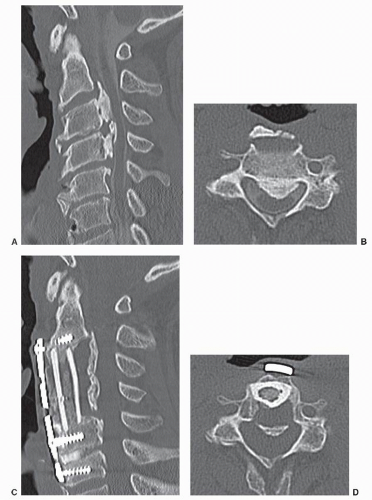
Diagnostic imaging of the site and the actual shape of the ossification permits determination of the degree of its
maturity, the stenosis of the vertebral canal, and any abnormal position of the vertebral artery. Flexion-extension plain radiographs can show abnormal mobility between two adjacent ossifications. A computed tomography (CT) of coronal and sagittal reconstruction views is required to precisely show the extent and shape of the OPLL. A CT myelogram and/or magnetic resonance imaging (MRI) can be used to clearly define the extent of the lesion compressing the spinal cord and the level at which the vertebral body and the ossification should be transversely bisected. The surgeon should craft a surgical plan of the area to be decompressed and decide preoperatively on a graft size. It is necessary to include the hyperplastic ligament next to the OPLL to avoid the gradual spread of ossification. Visualization of hyperplastic ligaments has been well demonstrated by MRI (Fig. 81.4).
maturity, the stenosis of the vertebral canal, and any abnormal position of the vertebral artery. Flexion-extension plain radiographs can show abnormal mobility between two adjacent ossifications. A computed tomography (CT) of coronal and sagittal reconstruction views is required to precisely show the extent and shape of the OPLL. A CT myelogram and/or magnetic resonance imaging (MRI) can be used to clearly define the extent of the lesion compressing the spinal cord and the level at which the vertebral body and the ossification should be transversely bisected. The surgeon should craft a surgical plan of the area to be decompressed and decide preoperatively on a graft size. It is necessary to include the hyperplastic ligament next to the OPLL to avoid the gradual spread of ossification. Visualization of hyperplastic ligaments has been well demonstrated by MRI (Fig. 81.4).
The ventral floating method thins the ossification and disconnects it from the surrounding bony tissues, which makes the ossification migrate forward. The upper and lower margins of the corpectomy are situated at the end of the uncompromised area of the subarachnoid space. The width of excision for transverse decompression should be more than 20 mm to avoid residual ossification to prevent insufficient floating. Awareness of the position of the vertebral artery is particularly important to prevent arterial injury during transverse decompression of the OPLL. The corpectomy is deepened straight to maintain the perpendicular line relative to the ventral surface of the vertebrae. An oblique thinning of the OPLL may cause uneven decompression of the spinal cord, resulting in neural complications such as Brown-Sequard syndrome.
After decompression is complete, the vertebral column is reconstructed. Reconstruction, as well as decompression of the vertebral column, is important. An unskilled fusion technique is certain to nullify the decompression. A fibular bone graft with a ventral plate is preferred for reconstruction. When a ventral plate is employed, a soft brace is used postoperatively for about 3 months instead of a halo vest.
OPERATIVE TECHNIQUE
Spinal monitoring during the operation is usually performed. The authors typically measure compound muscle action potentials induced by brain stimulation to monitor the motor tract during surgery (Fig. 81.3). Hyperextension position of the cervical vertebrae is avoided when the preoperative provoking test is positive. If neck extension is required for high cervical cases, the mandible is pulled rostrally in the neutral neck position to optimize access to the spine.
An oblique skin incision is made along the border of the sternocleidomastoid on the left side of the neck. When the OPLL is short or segmental, extending less than three vertebral bodies, a horizontal skin incision is sufficient. The ventral surface of the vertebral column is exposed. Bilateral longus colli muscles are retracted, and retractors are set up carefully on these edges so as not to injure the esophagus, trachea, or carotid sheath. The disk material is removed roughly with a rongeur, pituitary forceps, or a curette until the annulus becomes visible.
The disks should be sufficiently curetted as far as the bilateral Luschka joints to ensure accurate canal width. This also ensures maintenance of the correct midline of the vertebral column during surgery. The corpectomy is initiated by drilling bilateral holes in the joints of Luschka and nibbling away at the vertebral body. Discectomy and corpectomy are performed in an alternating fashion. Upon reaching the dorsal cortex, a careful and skillful air drill technique under a microscope is essential.
In cases in which the ossification has a wide base, the ossification is thinned in the shape of the bottom of a ship until part of the ossification is removed and the soft tissue underneath the ossification is slightly visible or felt by the light touch of a microprobe (Fig. 81.2). However, in cases involving a mushroom-like OPLL (i.e., an ossification with a narrow base and a large head), the width of decompression should be carefully planned. When the dorsal wall disappears, a soft tissue full of epidural blood vessels around the ossification emerges and covers the ossification. If thinning is stopped at this stage, a large ossification will remain
intact. The fibrocartilage-like soft tissue is cauterized with a bipolar electric forceps and regresses outward. The ossification then gradually becomes wider and can be thinned from the midline to the lateral side with an air drill or an ultrasound scalpel if necessary (Fig. 81.5 and 81.5).
intact. The fibrocartilage-like soft tissue is cauterized with a bipolar electric forceps and regresses outward. The ossification then gradually becomes wider and can be thinned from the midline to the lateral side with an air drill or an ultrasound scalpel if necessary (Fig. 81.5 and 81.5).
When freeing the ossification from the surrounding bone tissues, the rostral and caudal ends of the ossification are first cut transversely and then disconnected from the pedicle that is situated laterally. When the thinned OPLL appears to be like a board floating on water, decompression of the entire spinal cord is complete. If the surrounding soft tissue is still hard, the margin of the ossification should be removed to obtain a sufficient decompression. Early release of the OPLL from the vertebral bodies should be avoided, as this may induce uneven floating. In addition, a thin drilling of the OPLL is necessary for it to float sufficiently, because an already mature, rock-like ossification does not float as easily as an immature ossification.
The released ossification gradually migrates ventrally over time to enlarge the vertebral canal, likely due to pressure from the cerebrospinal fluid, up to 4 to 8 weeks postoperatively (7).
Unless the lateral wall of the vertebral body is completely removed in a massive OPLL bounded by the pedicle, the vertebral artery does not enter the operative field. In this case, to release the OPLL with greater safety, the position relative to the foramen should be checked on the preoperative CT.
RECONSTRUCTION
For reconstruction, the authors normally use a fibular bone graft reinforced by a ventral plate. Fibular bone is prepared by filling it with cancellous bone as shown in Figure 81.4C, which will promote graft union. Internal fixation using a plate stabilizes the cervical spine immediately after the operation, making a postoperative care easy. Additionally, it can prevent postoperative graft dislodging and spine deformity before fusion is complete. The length and the shape of the graft are appropriately determined such that the decompressed cervical column is extended slightly by mild manual power or by a Caspar distractor. In our experience, a graft that is too long causes anterior slipping of the graft or a vertebral body fracture (Fig. 81.6). A peg-in-hole bone grafting technique is used, in which small pieces of the ventral edge of the graft at the top and bottom are inserted into ditches of the upper- and lower-end vertebrae. The authors normally use a fixedtype screw for the bottom and a variable-type screw for the top of the graft. The bilateral muscles of longus colli are sutured to cover the plate as much as possible to avoid esophageal irritation.
Recently, the prefabricated hydroxyapatite graft has become available in some regions. This decreases donor site morbidity (Fig. 81.7).