and Colin L. W. Driscoll2
(1)
Department of Otolaryngology – Head and Neck Surgery, Stanford University, Stanford, CA, USA
(2)
Department of Otorhinolaryngology, Mayo Medical School, Rochester, MN, USA
Endolymphatic Shunt
Concept
Endolymphatic hydrops is the most agreed-upon pathology associated with Meniere’s disease. The postulated mechanism of this procedure is to stent open the endolymphatic sac to relieve the pressure buildup within the endolymphatic compartment. In reality, the mechanism by which this procedure can help patients is unknown and its efficacy is questioned. Nevertheless, it is a valuable procedure for the neurotologist to know how to perform as it has a low side-effect profile compared to other invasive treatments for recalcitrant Meniere’s disease.
Conditions treated
Meniere’s disease refractory to medical management in patients with serviceable hearing or in whom there is desire to avoid a destructive labyrinthine procedure (e.g., bilateral disease, poor pre-existing balance)
Risks
Hearing loss
Dizziness
Facial nerve injury
CSF leak
Disease recurrence (estimated at ~40–50 %)
Benefits
This is a nondestructive outpatient surgical procedure that preserves hearing. If it doesn’t work, other treatment strategies can be still used.
Additional notes
Only the posterior fossa dura need be exposed. If the sigmoid sinus is small, bone can be left over it. If the sigmoid sinus is large, the bone can be egg-shelled to allow it to be compressed and aid exposure of the endolymphatic sac.
1.
Approach to the endolymphatic sac. A right ear is shown. A simple mastoidectomy is first performed. The lateral semicircular canal (LSCC) is identified at the floor of the antrum. Donaldson’s line (dotted line) is helpful in finding the posterior semicircular canal (PSCC). It travels posteriorly along the plane of the LSCC and bisects the PSCC. The dura inferior to the PSCC is then exposed to identify the endolymphatic sac (ELS). This involves careful delineation of the sigmoid sinus and the vertical portion of the facial nerve so as not to inadvertently damage them.
2.
Case 1. Placement of a right endolymphatic shunt. A standard postauricular incision was used and a standard mastoidectomy performed. The mastoid antrum was opened, and the lateral semicircular canal (LSCC) can be seen. There were large retrofacial air cells that were opened. As a landmark, Donaldson’s line (dotted line) is shown.
There is some debate regarding how much bone removal should be performed. It is nice to widely decompress the sigmoid sinus and posterior fossa dura. The dura is then exposed from Donaldson’s line inferiorly to the sigmoid sinus. Removal of bone this far superiorly makes it easier to identify the most lateral aspect of the sac. The demarcation between normal dura which is thinner and bluish can be differentiated from the thicker and whiter sac. Also, the region where the sac enters the temporal bone can be seen when the dura is dissected from the petrous bone superior to the sac. A large retrofacial air cell tract like in this picture facilitates decompression of the most medial part of the sac. The dura is often very thin medial to the sac and needs to be carefully decompressed and elevated from the bone to avoid a CSF leak. This is an area not easily repaired.
3.
The presigmoid posterior fossa dura was identified and dissected free from the posterior temporal bone. Note how the dense otic capsule bone of the posterior semicircular canal is clearly delineated at the tip of the suction. Dura should not be exposed superior to this or the posterior canal may be inadvertently opened.
4.
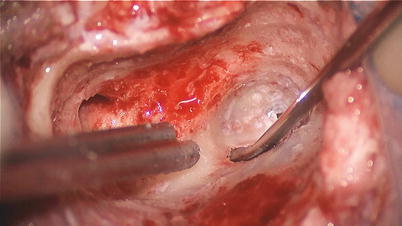
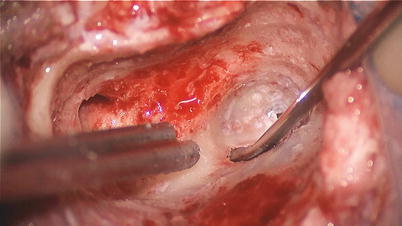
Drilling was continued deeper within the retrofacial air cells to fully expose the endolymphatic sac (ELS). The sac is simply a thickening of the dura in this region. It is often difficult to distinguish its margins, and so it is best to drill deep enough so that the endolymphatic duct can be identified coursing from the sac into the temporal bone. The lateral semicircular canal (LSCC) and posterior semicircular canal (PSCC) are shown.