Chapter 33 Surgical Approach to Falcine Meningiomas
Falcine meningiomas arise from the falx cerebri and make up approximately 5% to 9% of all intracranial meningiomas.1–2 Falcine meningiomas differ from parasagittal meningiomas in that parasagittal tumors originate from the dura mater enclosing the superior sagittal sinus and are up to 5 to 7 times more common that falcine lesions.3–4 Cushing further distinguished falcine meningiomas from parasagittal tumors by how, from the surgeon’s perspective, falcine tumors are often concealed by overlying cerebral cortex;5 however, large falcine meningiomas can grow superiorly to secondarily invade the superior sagittal sinus.
Symptoms and Presentation
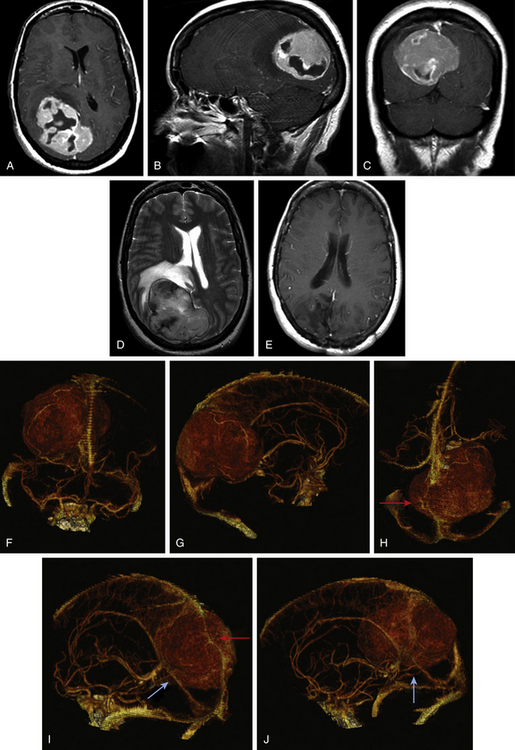
Falcine meningiomas located at the level of the anterior third of the superior sagittal sinus often present somewhat insidiously and result in a frontal lobe syndrome (Fig. 33-1A to F). Slowly progressive symptoms include short attention span, poor short-term memory, personality changes, apathy, and emotional instability; often this complex is confused with age-related dementia, delaying diagnosis. Consequently, anterior third tumors are frequently larger in size at the time of presentation than tumors in other regions. In extreme cases, patients can also present with signs of increased intracranial pressure, including headache, papilledema, or optic atrophy. Of patients with anterior third falcine meningiomas, 25% have seizures, but they are less frequent and less localizing than when tumors abut motor cortex.6
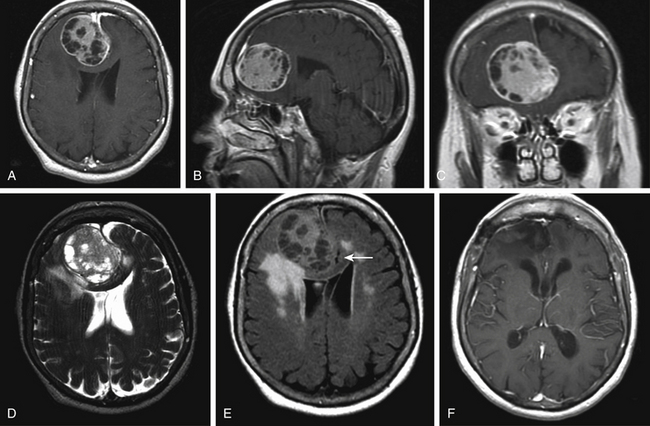
Tumors along the middle third of the superior sagittal sinus are usually located adjacent to the motor and sensory regions and produce more focal and localizable symptoms that cause patients to seek earlier medical intervention. Earlier presentation of symptoms allows for earlier diagnosis, and, thus, tumors in this region rarely attain the same bulk as tumors in the anterior third. While symptoms of increased intracranial pressure are rare, tumors in this region are more likely to produce spastic weakness and focal seizures that involve the contralateral foot and leg. Both motor cortices may be affected if the tumor extends bilaterally from the midline. Patients with meningiomas involving the posterior third of the sagittal sinus usually present with persistent headache and often are found on exam to have a hemianopsia (Fig. 33-2A to E). The degree of visual field involvement depends on the size and location of the tumor. Smaller tumors located above the calcarine fissure can cause anopia to the inferior quadrant. Smaller tumors along the tentorium cerebelli may involve the visual cortex below the calcarine fissure and only produce anopia in the upper quadrants. Larger tumors, on the other hand, can case homonymous hemianopsia with macular sparing. Some patients may present with reports of visual hallucinations. Tumors of the middle and posterior third can occasionally present with bilateral symptoms as the tumor extends across the falx.
Radiographic Findings
Magnetic resonance (MR) imaging is the gold standard for preoperative assessment of falcine meningiomas. Falcine meningiomas also frequently extend bilaterally, acquiring a dumbbell or bi-lobed shape with invagination into the medial aspects of both left and right hemispheres. Attempts to use MR imaging to differentiate histologic types of meningiomas have thus far been limited. Although efforts to differentiate benign from atypical meningiomas using MR spectroscopy (MRS) have been attempted, noninvasive measures have been unreliable.7 The majority of tumors appear iso- or slightly hypo-intense relative to the cortex on noncontrast T1-weighted MR images. The T2-weighted characteristics can be variable and are believed to correlate best with histologic subtype, vascularity, and consistency.8 Tumors that are hypo- to iso-intense on T2-weight imaging are found to be more firm and are histologically more fibroblastic or transitional (Fig. 33-1D and Fig. 33-2D). More malignant meningiomas, on the other hand, are more likely to exhibit greater brain edema that manifests as increased hyperintensity on T2-weight imaging and can be suggestive of pial invasion.9–10
For preoperative planning, multi-planar T1-weighted gadolinium enhanced MR images can provide coronal, sagittal and axial views that help in defining the tumor’s anatomic location, size, and cortical involvement (Fig. 33-1A to C and Fig. 33-2A to C). Brain edema adjacent to the tumor can be a sign of pial invasion and can be assessed preoperatively using T2-weighted images and fluid-attenuated inversion recovery (FLAIR) sequences (Fig. 33-1E). Three-dimensional (3D) T1-weighted gadolinium enhanced multiecho, magnetization-prepared, rapid gradient echo images can also be used with neuro-navigational tools to provide surgeons with intraoperative guidance.
Cerebral angiography can provide essential information delineating the tumor’s arterial feeding pattern. Additionally, arterial phase of the angiography can provide crucial information on the course, displacement and possibly the encasement of the anterior cerebral arteries (ACA), pericallosal arteries, and callosomarginal arteries. The venous phase of the angiogram is also vital toward determining the patency of the superior sagittal sinus, understanding the anatomy of the draining cortical veins in relation to the tumor and the degree of collateral circulation.11,12 If the sinus is occluded, the anatomy of the draining collateral vessels needs to be clearly identified during preoperative planning and meticulously preserved during surgery. Inadvertent occlusion of collateral vessels may result in severe postoperative complications such as venous infarct and cerebral edema.
The gold standard for cerebral angiography remains digital subtraction angiography (DSA). DSA provides a dynamic view of both the arterial and venous phases, better resolution of small vessel feeders, better accuracy in identifying sinus obstruction, and areas with reversal of normal venous flow. However, DSA is invasive and associated with a small, but not insignificant, risk for strokes, vessel injury, postdiagnostic hematoma, and possible renal injury from contrast use. Noninvasive means to evaluate the cerebral vasculature include MR angiography and CT angiography. MR angiography/venography capitalizes on its intrinsic sensitivity to flow to detect the patency of vessels. Vessels with high flow give rise to high signal intensity while the absence of flow is characterized by reduced signal intensity.13,14 The technical limitations to MR-angiography include its susceptibility to flow-related artifacts such that patent but obstructed regions of the sinus may appear completely occluded due to decrease in flow and the ability for intracellular deoxyhemoglobin/methemoglobin found in clot can create false signals to suggest a patent vessel. Other practical limitations include longer image acquisition times, and sensitivity to patient movement. CT-angiography/venography (CTA/CTV) is acquired using thin 0.625-mm slices on a helical 64-channel multidetector scanner during the peak arterial and venous enhancements. The acquired images can be viewed using maximum intensity projection (MIP) images, multi-planar reconstruction (MPR) images, and Vitrea 3D reconstruction images (Vital Images, Minnetonka, MN) to provide the surgeon a better sense of the tumor and its relationship to the vasculature (Fig. 33-2F to J). The faster image acquisition times as well as its ability to maintain high spatial resolution has made CTA/CTV the preferred method for routine preoperative vessel assessment at our institution. CTA/CTV has better small-vessel and sinus resolution and fewer motion and flow artifacts seen in MR venography.15–16 In a study by Wetzel and colleagues, CTV was compared to digital subtraction angiography and CTV was found to have an overall sensitivity of 95% and 91% specificity while DSA had 90% sensitivity and 100% specificity.17 Additionally, the shorter image acquisition times allow for less motion artifacts and makes CTA/CTV better suited for uncooperative or sick patients.
Operative Technique
Positioning
For tumors located in anterior third of the sagittal sinus, the patient is placed in a supine position with the head slightly elevated. Tumors around the middle third of the sagittal sinus can be approached with the patient supine with the head elevated and flexed, or, alternatively, a semiprone or lateral approach can be used, especially if the tumor is located more posteriorly. A semilateral, semi-sitting position with the head well elevated so that the scalp over the area of the tumor is at the highest point can also be considered for tumors in this area. For tumors involving the posterior third, the patient is placed in the lateral position and the head is elevated and turned to the opposite side so that the center of the tumor is uppermost.18–19 The head is secured with the Mayfield 3-point fixation head rest and the patient’s body is secured to table with tape. Foam padding and gel rolls are used to pad all pressure points.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree