Chapter 36 Surgical Management of Sphenoid Wing Meningiomas
Sphenoid wing meningiomas (SWMs) constitute about 14% to 20% of intracranial meningiomas.1 Although they originate from arachnoid cells, they are usually attached to dural thickening or folding, where they receive their blood supply. Infiltration of the adjacent bone is not unusual; neither is growth around or inside the cranial base foramina.2 Most SWMs are relatively easy to remove; however, they are sometimes challenging, especially when they invade the cavernous sinus, internal carotid artery (ICA), and visual pathway. In these cases, total excision is extremely difficult, resulting in high morbidity and a high rate of regrowth or recurrence.3
Anatomic Observations
The designation SWM refers to tumors that originate in any part of the bony crest formed by wings (lesser and greater) of the sphenoid bone, which represents the boundary between the anterior and the middle cranial floor.4 This anatomic portion is also known as the sphenoid ridge, where the lesser wing constitutes its internal two thirds and the greater wing its external third. The lesser wing is the most complex area because of its relationship with the orbit, ICA, cavernous sinus, optic foramen, superior orbital fissure, sylvian fissure, middle cerebral artery (MCA), tip of the temporal lobe, and basal surface of the frontal lobe. In contrast, the greater wing is located in the external portion and is in relation to the frontal and temporal lobes (predominantly with their opercular areas) in its intracranial surface and with the orbit and zygomatic fossa in its extracranial surface, where it serves as insertion to the temporal muscle. It also forms the pterion when it articulates with the frontal squama, temporal, and parietal bones.4
Classification
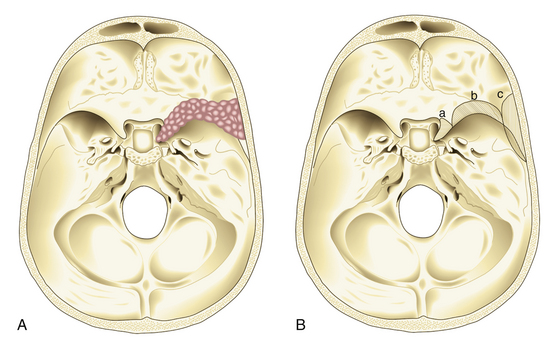
In 1938, Cushing and Eisenhardt classified SWMs into two main varieties: en plaque and globoid (Fig. 36-1).
En-plaque Meningiomas
Also known as spheno-orbital meningiomas or hyperostotic meningiomas of the sphenoid wing, en-plaque meningiomas refer to tumors with a carpet-like dural growth, which are associated with a reactive hyperostosis that, in most cases, is marked and principally responsible for clinical manifestations5,6 (Fig. 36-1A). Sphenoid wing hyperostosis has been reported as high as 42% of all meningiomas in this area.7,8 Due to its extensive bone involvement, differential diagnosis should include fibrous dysplasia, osteoma, osteoblastic metastasis, Paget’s disease, hyperostosis frontalis interna, erythroid hyperplasia, and sarcoidosis.6,9,10 It frequently extends posteriorly toward the cavernous sinus and anteriorly toward the orbital apex, where it causes proptosis and oculomotor deficits, the primary clinical manifestations of these lesions.5 Hyperostosis in meningiomas was initially described by Brissaud and Lereboullet in 1903.11 Theories regarding the cause of hyperostosis include vascular disturbances, irritation of bone without actual invasion, previous trauma, bone production by tumor cells, or osteoblastic stimulation of normal bone. Currently, the most widely accepted theory is that this bone growth is actually bone invasion by tumor cells.3,11,12
Globoid Meningiomas
Globoid meningiomas have traditionally been classified into three groups: (1) deep, inner, or clinoidal; (2) middle or alar; and (3) lateral, outer, or pterional (Fig. 36-1B). Middle or alar meningiomas have radiologic characteristics similar to lateral or pterional meningiomas. Surgical resection and clinical results of both types are almost identical. For this reason, some authors suggest that globoid meningiomas of the sphenoid wing can be classified into only two groups: deep, inner, or clinoidal and lateral, outer, or pterional, discharging the middle or alar variety.13 Deep, inner, or clinoidal meningiomas represent the most complex variety of these tumors, whose resection, in most cases, implies increased morbidity and a high rate of recurrence.14–17 In this region, the cavernous sinus is the most critical area; therefore, clinoidal meningiomas are subclassified into two groups: tumors without extradural growth and tumors with extradural growth into the cavernous sinus.13,18
There is a third and debatable variety of SWMs. These are tumors that grow within the diploë without an epidural, subdural, or subcutaneous component and are referred to as intraosseous or intradiploic meningiomas.3,6 The origin of these tumors in the skull base is controversial. Arachnoid cells have been described, following the vessels and nerves in bone foramina or trapped within the sutures. However, some authors19 doubt the existence of these tumors, proposing that they are really a variety of en-plaque meningiomas in which the dural component of the tumor is not well identified on preoperative imaging studies, mostly considering that many of these tumors were described before the era of magnetic resonance imaging (MRI).
Clinical Course
The most common clinical sign of en-plaque meningiomas is proptosis, which usually is slowly evolving, unilateral, nonpulsatile, and irreducible.11 Possible causes of this sign are hyperostosis of the orbital walls, periorbital tumor invasion, intraorbital tumor, and venous stasis caused by compression of the ophthalmic veins. Related symptoms include headache, orbital pain, visual deficit, ptosis, diplopia, ectropion, conjunctivitis, corneal ulceration, and scleral hemorrhages. Unilateral loss of vision is rare and is caused by a narrowing of the optic foramen.
In regard to clinoidal meningiomas, clinical manifestations are dominated by visual field problems presenting virtually any pattern. On the other hand, visual acuity deficits are only somewhat variable and are reported in between 39% and 92% of patients.1,7 When these tumors invade the cavernous sinus, the most common symptoms are oculomotor deficit (especially on cranial nerve VI) and facial hypoesthesia.
Diagnosis
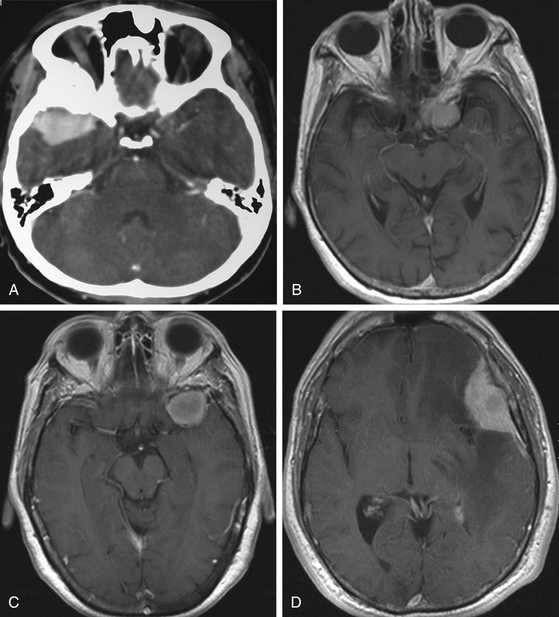
Although clinical manifestations may be strongly suggestive of the diagnosis, especially in spheno-orbital meningiomas, imaging studies are indispensable to establish the diagnosis and to propose the best therapeutic option (Fig. 36-2).
Computed Tomography
Computed tomography (CT) is predominantly useful in en-plaque meningiomas because it provides more precise information regarding the extent of bone invasion, also allowing correct planning for reconstruction (Fig. 36-2A). The dural component of these tumors is typically found as an isodense image with contrast enhancement, being contiguous with the surrounding dura mater.11 However, it is not always possible to observe this due to its carpet-like appearance. Also, it may be occulted by the high hyperdensity of the contiguous bone growth. There is no correlation between size of the hyperostosis and size of the meningeal tumor. In fact, small dural components are frequently found associated with large bone masses. A bone window algorithm is mandatory in terms of obtaining better definition of bone thickening. Performing axial and coronal projections, as well as three-dimensional (3D) reconstruction, also facilitates both complete resection and reconstruction. The most common locations of hyperostosis of en-plaque meningiomas are, in order of frequency, the lesser wing of the sphenoid bone, the greater wing of the sphenoid, the roof of the orbit, the inferior orbital fissure, the infratemporal fossa, and the orbital rim.
Globoid tumors appear on CT as well-defined isodense lesions that present an intense and homogeneous contrast enhancement. Even though they are usually slow-growing masses, it is not uncommon to find perilesional edema invading the temporal lobe and centrum semiovale, which is attributed to compression or occlusion in the superficial middle cerebral vein or sphenoparietal sinus; there is no direct relationship between the grade of edema and the size of the tumor. Clinoidal meningiomas usually show hyperostosis of the anterior clinoid process (ACP), causing narrowing of the optic canal and the superior orbital fissure.1 CT has some limitations when these tumors infiltrate the cavernous sinus; however, computed angiotomography (CAT) may help by providing more precise information about blood supply and vascular relations of the tumor.
Magnetic Resonance Imaging
MRI is more useful in globoid meningiomas (Fig. 36-2B to D) and for the correct evaluation of the dural component of en-plaque meningiomas; however, this study’s principal limitation is the osseous tissue. Globoid meningiomas show different appearances on MRI. When their vascularity is not so marked, they usually present as a homogeneous isointense lesion in both T1- and T2-weighted images;20 on the other hand, when they are highly vascularized (angioblastic meningiomas), multiple hypointense images (“empty signals”) can be seen in the interior of the tumor. Gadolinium enhancement is usually intense and uniform, and a T2-weighted image is particularly useful in demonstrating perilesional edema.
Angiography
Considering the clear image of the vascular anatomy obtained with CAT and MRA, particularly with 3D reconstructions, angiography is indicated only in special SWM cases. Selective catheterization provides specific information about the blood supply of the tumor1 and allows the possibility of preoperative embolization. Another indication for angiography is for performing carotid occlusion tests, especially in tumors invading the cavernous sinus and when arterial bypass is planned.
Treatment
Surgical management is, without doubt, the best therapeutic option for SWMs. This treatment is indicated considering the following factors: size of the lesion, presence of signs or symptoms, patient’s condition, changes in the adjacent cerebral tissue (edema) on imaging studies, and surgeon’s experience. In general, surgery is indicated in all patients who are in good health and have a tumor size greater than 2.5 cm. The goal of surgery in all cases should be radical excision of the tumor, which means resection of the lesion, along with the dural implant (1-cm margin) and all hyperostotic bone. This objective is accomplished in the large majority of SWMs except in some spheno-orbital and clinoidal meningiomas, particularly when they present invasion to the cavernous sinus. For these cases, most authors recommend excising the tumor, dura mater, and infiltrated bone on extracavernous areas but leaving the intracavernous portion for another adjuvant treatment, such as radiosurgery, because even in experienced hands, oculomotor morbidity is extremely high after a direct approach to this region.1,2,4,18,21
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree