Fig. 16.1
Frontolateral approach (drawing). The craniotomy is performed through a burr hole at the orbital button of the frontal bone behind the anterior temporal line
16.6.2 Bifrontal Approach
The patient is lying in the supine position on the operating table with the head secured in the Mayfield head holder. The skin is cut slightly posterior to the frontal hair line from zygoma to zygoma. The scalp and pericranial flaps are reflected anteriorly. A burr hole is placed on each side of the orbital buttons. A craniotomy is performed extending anteriorly as close as possible to the orbital roof and posteriorly along the convexity of the cranium. The basal line of the craniotomy involves both tables of the frontal sinuses, and the mucous membranes are completely removed. The dura is cut parallel to the base and the sagittal sinus is ligated and cut at the cecal foramen; the falx is transected to open up the operative field (Fig. 16.2).
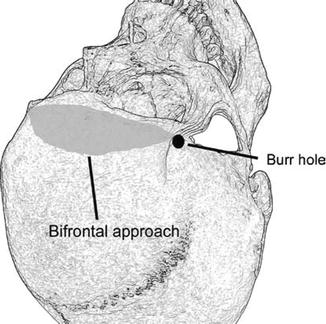
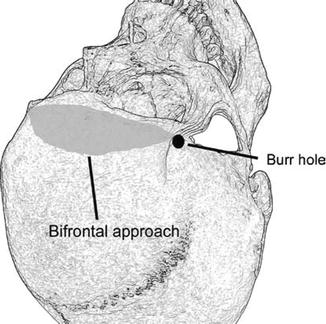
Fig. 16.2
Bifrontal approach (drawing). The craniotomy is performed through a burr hole at the orbital button of the frontal bone behind the anterior temporal line
16.6.3 Pterional/Frontotemporal Approach
For the pterional approach, operative positioning is similar to the frontolateral approach, but the head is rotated more to the contralateral side (30–40°). The single burr hole is placed at the same location, but the craniotomy is performed more posteriorly exposing the frontal and temporal lobe with the Sylvian fissure and the sphenoid ridge. The lesser wing of the sphenoid is resected to the superior orbital fissure depending on the tumour size, to allow exposure of the lesion with minimum brain retraction (Fig. 16.3).
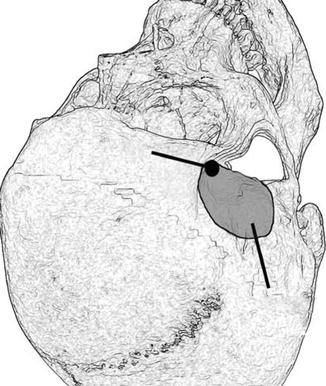
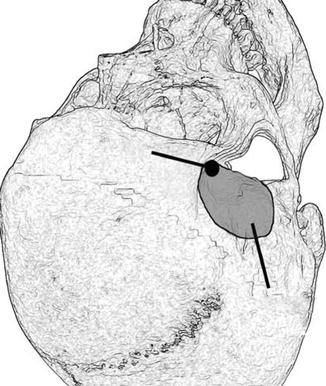
Fig. 16.3
Pterional approach (drawing). The craniotomy is performed through a burr hole at the orbital button of the frontal bone behind the anterior temporal line extending more to the frontotemporal region compared to the frontolateral approach
16.6.4 Microsurgical Tumour Resection
When the frontolateral or pterional approach is performed, the ipsilateral optic nerve and the internal carotid artery are first identified. The tumour capsule is opened medial to the ipsilateral optic nerve and the tumour debulked to decompress the optic nerve using microsurgical techniques. Tumour resection is continued in a piecemeal fashion until the optic chiasm and the contralateral optic nerve are visible. Regardless of the selected surgical approach, it is paramount to avoid injury to the blood supply of the optic apparatus. As the inferior surface of the optic nerve and chiasm receive their blood supply from a group of small arteries, which arise from the medial wall of the internal carotid artery [6], these may not be mistaken as tumour feeders and the use of bipolar coagulation should be restrictive. Special attention has to be paid for the identification and preservation of the optic cistern and also the separation of the layers of the optic cistern and the tumour capsule. To preserve the small arteries supplying the optic nerve and chiasm, it is advisable to leave the tumour capsule until the end of sufficient tumour debulking and preparation. This will provide a protective plane of dissection for the optic nerves and optic chiasm as well as the perforation vessels. Only when enough space is achieved after tumour removal, the tumour capsule should be removed respecting the arachnoidal plane to the small vessels.
Then the tumour matrix is coagulated and the basal dura resected. In case of hyperostosis or bony tumour involvement, this site is removed with a diamond drill. Tumour resection is completed to the posterior direction, when the pituitary stalk becomes visible and is preserved. In case of eventual opening of the sphenoid sinus, a pericranial flap or fascia of the temporal muscle with addition of fibrin glue has been used for covering the defect to avoid any postoperative CSF fistula.
The authors’ surgical series includes 72 meningiomas solely arising from the tuberculum sellae treated through three different surgical approaches between 1978 and 2002. Tumours were operated through the frontolateral (1984–2002, n = 30), pterional/frontotemporal (1982–2002, n = 21) and bifrontal (1978–1995, n = 21) approaches. Four patients of them experienced previous surgeries in outside hospitals.
The maximum tumour diameter ranged from 1 to 5 cm with a mean diameter of 2.8 cm. Tumours size was <3 cm in 39 cases (54.2 %) and ≥3 cm in 33 cases (45.8 %).
The mean diameter of tumours was 2.5 cm (1–5 cm) in patients operated through the frontolateral approach, 2.66 cm (1–5 cm) in cases where the pterional/frontotemporal approach was used and 3.49 cm (1.5–5 cm) in cases where the bifrontal approach was performed. In tumours involving the cavernous sinus, the intracavernous part of the tumour was not radically removed to prevent any new cranial neuropathies (Fig. 16.4a–e).
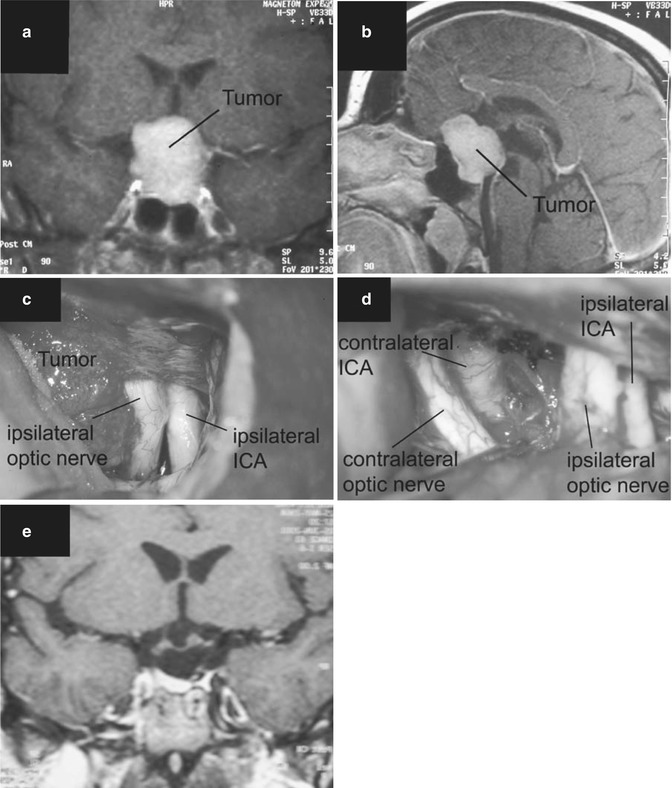
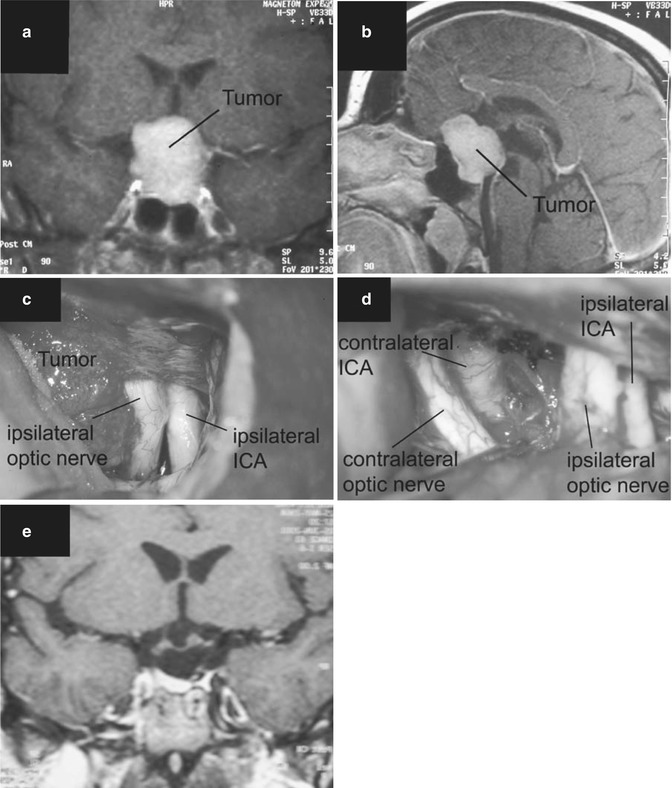
Fig. 16.4
(a) Tuberculum sellae meningioma on preoperative T1-weighted coronal MRI scan with gadolinium enhancement. (b) Same tumour on preoperative T1-weighted sagittal MRI scan with gadolinium enhancement. (c) The intraoperative view of the tumour through a right frontolateral approach shows a lateral displacement of the ipsilateral optic nerve, which is also partially covered by the tumour. ICA internal carotid artery. (d) After complete tumour removal, the contralateral optic nerve and internal carotid artery (ICA) are visible. (e) Postoperative T1-weighted coronal MRI scan with gadolinium enhancement confirming total tumour removal
16.7 Results
16.7.1 Morbidity and Mortality
The mortality rates for surgery of tuberculum sellae meningiomas ranged from 0 % in microsurgical series [18, 38] to even as high as 67 % in earlier macrosurgical series [32]. The mortality rates of surgical series published since the year 2000 ranged from 0 to 8.7 % [4, 18, 21, 27] including our present series. Concerning our current surgical series, it has to be emphasized that mortality rates were considerably different depending on the selected surgical approach. The mortality rates of the frontolateral and pterional groups were 0 %, whereas the mortality rate in patients who underwent bifrontal craniotomy was 9.5 %.
Some authors noted the influence of tumour size on surgical outcome for suprasellar meningiomas [8, 19, 28, 49]. Higher mortality rates were reported in patients with tumours larger than 3 cm in diameter compared with mortality rates in patients with smaller tumours. However, others could not confirm this finding in their surgical series [3, 24], and we also cannot support this observation in our series.
In the literature, several potential complications were reported with removal of tuberculum sellae meningiomas. They have been mainly divided into ophthalmological and nonophthalmological causes.
In a review of suprasellar meningiomas, Finn and Mount [19] found that 20 % of survivors had evidence of serious morbidity. The reported nonophthalmological complications of removal of these tumours include diabetes insipidus, CSF fistula (via the frontal sinus or an eroded base of the skull), meningitis, cerebral infarction or haemorrhage [10, 15, 19, 30, 39, 48, 49]. Diabetes insipidus after removal of a suprasellar meningioma is one of the most frequently reported endocrinological events in the literature with a frequency of 5–33 % [2, 13, 17, 19, 30, 49] although we did not observe any case of diabetes insipidus in our series.
Injury of the olfactory nerves was reported more frequently after a subfrontal (unilateral frontal or bifrontal) approach. This observation is also reflected in our series, especially in patients who underwent bifrontal craniotomy.
Some authors therefore advocated the pterional approach, which has the advantage to minimize injury to the olfactory nerves [27].
Also the occurrence of CSF leakage or infection from frontal sinus transgression was considered as a disadvantage of the subfrontal approach [27]. However, it has already been shown in the past that violating the frontal sinus does not necessarily lead to serious complications. In early reports, the infection rate was less than 2 % [43] and there was no incidence of fatal meningitis. Also more recent series did not reveal any severe complications from entering the frontal sinus [2, 5, 35, 46]. In our surgical series, postoperative CSF fistula did not lead to postoperative meningitis with proper precautions.
It needs to be emphasized that postoperative CSF leak has been a significant concern using the endoscopic endonasal approach to resect meningiomas of the frontal base including tuberculum sellae meningiomas with reported rates as high as 20–43 % [7, 16, 50]. Further studies need to determine if the use of vascularized nasoseptal flap can lead to lower CSF leak rates than those reported to date with other multilayer repair methods.
In our surgical series, the incidence of postoperative brain oedema (n = 4, after bifrontal craniotomy) and venous brain infarction (n = 1, after bifrontal craniotomy) was considerably higher in patients who underwent bifrontal craniotomy. In our experience, these complications have to be ascribed to the routine sectioning of the superior sagittal sinus and draining midline veins when performing the bifrontal approach. Due to our experience, we no more can support previous statements, that the anterior third of the superior sagittal sinus can be safely transected without risking serious complications. Due to these results, the senior author no more performs the bifrontal approach for resection of tumours in the anterior skull base and sellar region.
16.7.2 Extent of Tumour Resection
The percentage of gross total tumour resection of suprasellar meningiomas ranged from 35 to 100 % [1–5, 12, 13, 15, 18, 19, 21–25, 27, 28, 34, 35, 39, 46, 48, 49]. The extent of tumour resection has improved with the advent of modern microsurgery with a total resection rate of 35–76 % in macrosurgical series compared to 58–100 % in microsurgical series. Although it has been stressed that complete tumour resection should not be attempted risking higher morbidity rates, recent microsurgical series (including our series) showed that high rates of complete tumour resection can be performed without increasing morbidity [2, 5, 13, 18, 27, 34, 35, 40, 46, 47].
The rate of total tumour removal (Simpson 1 + 2) did not differ significantly among different approaches in our series. In patients operated through the frontolateral approach, total tumour removal (Simpson 1 + 2) could be achieved in 28 of 30 cases (93.3 %). Tumours operated through the pterional or bifrontal approach could be totally resected in 19 of 21 cases (90.5 %) in each group. Total tumour removal could be achieved in 66 cases altogether (Simpson 1 + 2, 91.7 %).
Previously, it was often mentioned that the frontolateral approach does not allow attacking the tumour from various angles compared to the bifrontal approach; however, we have learned that there is no need to see the tumour from different directions to achieve high rates of total tumour resection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








