Fig. 43.1
Syringomyelia from an arachnoid cyst. MR-T2-weighted sagittal image with no obvious pathology seen (left); MR-3D-true-fisp-weighted sagittal image (CISS sequence) with visualisation of an arachnoid cyst compressing the spinal cord and ascending syringomyelia (middle). Intra-operative photo of CSF disturbance by the subarachnoid cyst and its resection (right)
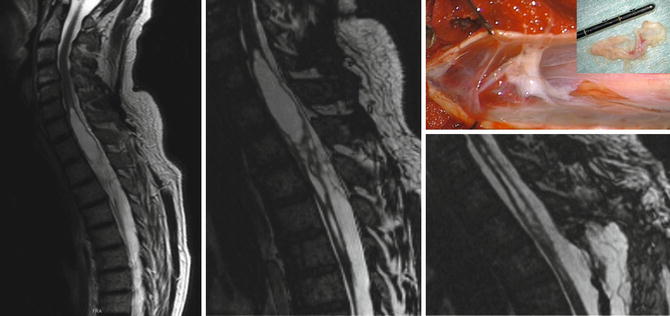
Fig. 43.2
Post-traumatic syringomyelia. MR-T2-weighted sagittal image with extensive syringomyelia (left). MR-3D-true-fisp-weighted image reveals post-traumatic tethering leading to CSF disturbance and consecutive syringomyelia (middle) [22]. Intra-operative visualisation of the thickened arachnoid membranes leading to a post-traumatic tethered cord with consecutive syringomyelia
43.1.5 Hydromyelia
As a result of the increased use of diagnostic imaging procedures in recent years, there have been larger numbers of patients diagnosed with filiform enlargement of the central spinal canal. Sometimes, these patients are quickly given the diagnosis of syringomyelia and thereby stigmatised. In these cases, it is useful to perform a careful diagnostic evaluation in order to differentiate between true early-stage syringomyelia and a congenital enlargement of the central canal or terminal ventricle [24]. True hydromyelia does not have a progressive clinical-neurological course and does not change on serial imaging and hence does not constitute a pathological finding.
43.2 Clinical Course
In the pre-MRI era, the prevalence of syringomyelia was estimated to be about 8.4 per 100,000 [28] patients treated in a neurological clinic, but since the introduction and widespread use of MRI, this estimate has risen to 24.5 per 100,000 [16]. In those forms of syringomyelia associated with cerebral malformations, symptoms are often quite delayed and typically occur in the third to the fifth decades of life (the most frequently associated cerebral defect: Chiari I malformation). Frequently, the initial symptom is pain and paraesthesia in the arms [34] and, subsequently, nuclear atrophy. Spasticity primarily occurs in the lower extremities. With a progressive course, the expansion of the cavities results in paresis and atrophy, often unilateral at first, and scoliosis due to paresis of the paravertebral musculature. In children, scoliosis is often the predominant initial clinical symptom of an underlying syringomyelia. Neurological abnormalities only develop after certain period has elapsed. In these cases, one clinical sign indicating the presence of a syrinx may be unilaterally diminished or absent abdominal skin reflexes [35]. The syrinx is predominantly located in the cervical or upper thoracic spinal segments. However, rostral extensions to the brainstem (syringobulbia) or caudal extension to the sacral segments is not unusual.
The spontaneous course of the illness depends upon the underlying pathology. In cases with tonsillar herniation or a mass in the area of the posterior cranial fossa, persistent disturbances in cerebrospinal fluid circulation may result in progressive syringomyelia, which can only be alleviated by relieving the disturbed CSF drainage in the posterior fossa. Likewise, in the case of spinal tumours, the clinical course of the secondary syrinx arising from the tumour depends upon treatment of the mass. Post-traumatic, post-inflammatory and post-chemical syrinxes frequently show an unpredictable course. Overall, approx. 60 % of patients with syringomyelia have a chronic and progressive course, while 25 % have a fluctuating course with periods of progression and periods when symptoms remain stable. Only approx. 15 % of patients have no progression in their deficits [31]. Generally, it is not possible to predict the course of the illness without knowing the individual aetiology. Case reports repeatedly remind us that any physical manoeuvres involving a sudden increase in intraspinal or intracerebral pressure may precipitate sudden deterioration. These would include vigorous sneezing or straining. Clinically, this often results in increased pain or the initial occurrence of pain. Secondary problems may also occur from infections, autonomic dysregulation and trophic disturbances. In most cases restoration of free cerebrospinal fluid flow leads to stabilisation of existing neurologic symptoms. In some cases, existing neurological deficits may even improve, although once neuropathy has been present for a long time, it will tend to persist. In cases of the Chiari malformation, symptoms caused by brainstem compression will often regress, whereas symptoms directly caused by the syrinx may remain unchanged.
43.2.1 Therapeutic Principles
Syringomyelia should be regarded as a symptom of increasing arachnoid scarring from different possible aetiologies, with resultant disturbances in spinal fluid circulation. In many cases neurosurgical intervention to restore free cerebrospinal fluid flow leads not only to a collapse of the syrinx but can also stop progression of the clinical symptoms of syringomyelia, while in favourable cases, this may even result in clinical improvement. In this regard, the size of a syringomyelia does not correlate directly with the intensity of clinical symptoms. For tumours compressing the spinal cord, neurosurgical intervention or radiotherapy may sometimes become necessary. Conservative treatment primarily includes physical therapy and the symptomatic treatment of spasticity as well as pain management.
Since syringomyelia almost always has a very slowly progressive although chronic course, initial treatment is with symptomatic, medical and physical therapies. However, younger patients with post-traumatic syringomyelia without neurological deficit (e.g. secondary to whiplash injury) may benefit from early surgical intervention to prevent neurological deficits from ever having a chance to develop. A longer course of the illness (more than 2 years) is generally regarded as an adverse predictor for symptomatic improvement following neurosurgical intervention. The paresis and atrophy that may be present following a longer course generally do not regress, even after successful microsurgical arachnolysis. Neurosurgical intervention is indicated even if other symptoms have been chronically present for many years, if clinical or neuroradiological follow-up shows progression of the syrinx, especially in the cervical area, with increasing loss of sensorimotor function or distinct dissociative sensory disturbances in the upper extremities. In addition, surgical intervention with decompression of the cysts may partially relieve the accompanying pain and may halt progression. However, there have been no controlled prospective studies regarding the various forms of surgical treatment for syringomyelia. Larger case report series and retrospective studies have typically included a range of different neurosurgical interventions.
Relatively good evidence exists for both the pathophysiological mechanisms and clinical improvement after surgical treatment of the Chiari malformation with depressed tonsillar position by means of suboccipital decompression and, if necessary, reconstruction of the posterior cranial fossa with expansile duraplasty [3, 15, 18]. The question whether bony decompression of the posterior cranial fossa is an adequate treatment for tonsillar herniation or whether it is necessary to perform tonsillar coagulation remains a matter of dispute. Excessive expansion of the foramen magnum can lead to recurrence with herniation of larger portions of the cerebellum. During decompression it is important to be careful that a sufficient opening is created in the scarred arachnoid membranes to assure free passage of cerebrospinal fluid from the fourth ventricle. When treating patients with a Chiari malformation, it is important to be aware of the frequent coexistence of a bony anomaly affecting the cranio-cervical junction such as the Klippel-Feil malformation, basilar invagination or C1 subluxation. These congenital abnormalities may result in cranio-cervical instability after standard surgical treatment that may necessitate further surgical intervention.
After adequate neuroradiological demonstration of a focal arachnopathy, confirmed post-traumatic syringomyelia should be treated by surgical exploration. Preoperatively, the patients should be told clearly that the planned microsurgical arachnolysis is intended to stop the clinical-neurological progression of the condition, but that they should not anticipate regression of already existing deficits. After performing a laminectomy and opening the dura, the surgeon performs a microsurgical inspection with lysis of the arachnoid adhesions and, electively, may transect the denticulate ligament. Next, an allogeneic expansion duraplasty is performed to prevent recurrent adhesions in this area. In many cases, restoring free circulation of the cerebrospinal fluid results in the extensive collapse of the syrinx associated with clinical stabilisation [25].
Spinal cordectomy may be indicated following trauma with complete transection of the spinal cord if tension on the cord caused by scarring results in the cranial extension of the syringomyelia (traumatic tethered cord). This procedure may serve to prevent ascending tetraplegic symptoms that can result from such extension.
If no focal arachnopathy can be demonstrated after intensive neuroradiological workup (MRI with FLAIR, T1/T2 ± gadolinium-weighted images, cardiac-gated CINE-MRI for revealing CSF pulsation with additional 3D-CISS sequences) [22] but the syringomyelia appears to be clinically and neurologically progressive, the placement of a cysto-subarachnoid shunt may be indicated as a measure of last resort [16]. Multiple drainage procedures of various kinds performed in the past often resulted in only short-term success. Long-term results with clinical improvement of symptoms over time had been reported in up to 80 % of patients [20]. Based upon later reports suggesting the frequent occurrence of shunt dysfunction with recurrence of the syrinx in up to 50 % of surgically treated cases, as well as major scarring of the spinal cord at the insertion site, this therapeutic procedure could no longer be justified [8, 27, 29, 30].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








