24 Tarsal Tunnel Syndrome
Anatomy
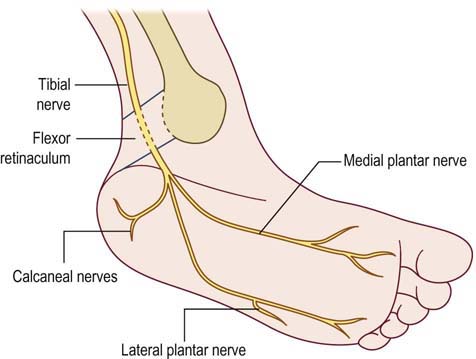
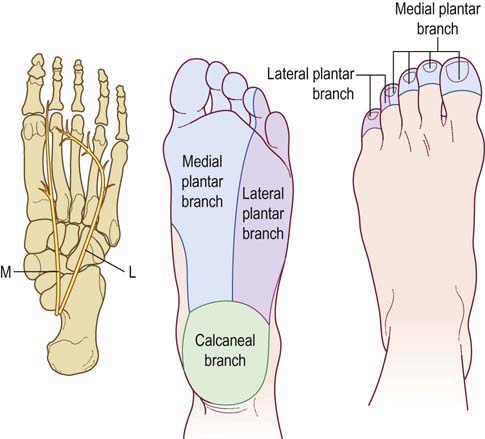
As the tibial nerve descends distal to the medial malleolus, it runs beneath the flexor retinaculum on the medial side of the ankle, through the tarsal tunnel (Figure 24–1). The tarsal tunnel is a fibro-osseous tunnel below the medial malleolus with a bony floor and a roof formed by the flexor retinaculum. In addition to the tibial nerve, the tibial artery and tendons of the flexor hallucis longus, flexor digitorum longus, and tibialis posterior pass through the tarsal tunnel. The distal tibial nerve then divides into three or four branches. One or two branches (medial and lateral calcaneal sensory nerves) are purely sensory and provide sensation to the heel of the sole (Figure 24–2). The other two branches, the medial and lateral plantar nerves, contain both motor and sensory fibers that supply the medial and lateral sole of the foot, respectively. Typically, the medial plantar nerve supplies the first three and a half toes (including the great toe), whereas the lateral plantar nerve supplies the little toe and the lateral fourth toe. Both plantar nerves innervate the intrinsic muscles of the foot. The muscles that are most accessible to study using needle EMG are the abductor hallucis brevis (AHB), flexor hallucis brevis (FHB), and flexor digitorum brevis (FDB) for the medial plantar nerve, and the abductor digiti quinti pedis (ADQP) for the lateral plantar nerve.
Clinical
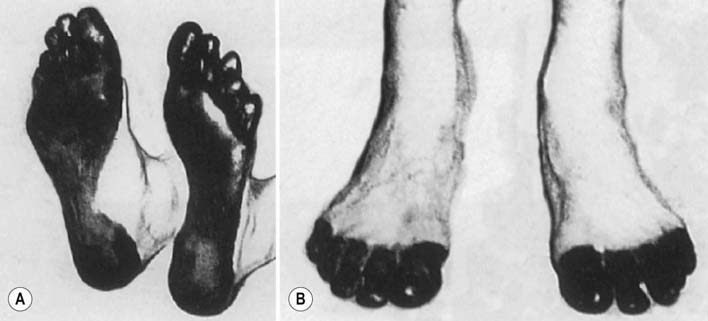
The most frequent symptom in patients with TTS is perimalleolar pain. Ankle and sole pain often is described as burning and often is worse with weight bearing or at night. Paresthesias and sensory loss involving the sole of the foot may occur due to compression of the plantar or calcaneal nerves (Figure 24–3). There are few other reliable clinical signs. Intrinsic foot muscle atrophy may occur but is not specific to TTS. For example, atrophy of intrinsic foot muscles may occur in L5–S1 radiculopathy, proximal tibial neuropathy, or polyneuropathy. It is extremely difficult to assess strength of the intrinsic foot musculature, because most of the important toe and ankle functions are subserved by the long extensors and flexors in the lower leg, which are innervated by the proximal peroneal and tibial nerves. Finally, many consider a Tinel’s sign over the tarsal tunnel to be suggestive of TTS. Unfortunately, like Tinel’s signs elsewhere, this is a nonspecific sign and may occur in some normal subjects. Significantly, the ankle tendon reflex, which is mediated by the tibial nerve proximal to the tarsal tunnel, is normal in TTS, as is sensation over the lateral foot (sural nerve) and the dorsum of the foot (superficial peroneal nerve).
Electrophysiologic Evaluation
Nerve Conduction Studies
Evaluation of suspected TTS is greatly simplified if one side is symptomatic and the other side is normal. This situation allows for side-to-side comparison studies (Box 24–1). The important nerve conduction studies to perform include bilateral tibial distal motor latencies to both the AHB and ADQP, for the medial and lateral plantar nerves, respectively, stimulating the tibial nerve proximal to the tarsal tunnel at the medial malleolus (Figure 24–4). Compound muscle action potential (CMAP) amplitudes and distal latencies are compared from side to side. Theoretically, if there is demyelination across the tarsal tunnel, the distal latencies on the involved side should be markedly prolonged. In axonal loss lesions, the CMAP amplitudes will be reduced, and the latencies will be normal or only slightly prolonged.
Box 24–1
Recommended Nerve Conduction Study Protocol for Tarsal Tunnel Syndrome
1. Distal tibial motor (medial and lateral plantar) studies, stimulating tibial nerve at medial malleolus and recording abductor hallucis brevis (medial plantar) and abductor digiti quinti pedis (lateral plantar). Comparison with contralateral side is required
2. Routine tibial motor study, recording abductor hallucis brevis, stimulating medial ankle and popliteal fossa
3. Routine peroneal motor study, recording extensor digitorum brevis and stimulating ankle, below fibular neck, and lateral popliteal fossa
4. Medial and lateral plantar mixed or sensory studies (plantar mixed and sensory responses usually require averaging several potentials). For mixed studies, stimulate medial sole and record medial ankle (medial plantar mixed); stimulate lateral sole and record medial ankle (lateral plantar mixed). For sensory studies, stimulate great toe and record medial ankle (medial plantar sensory); stimulate little toe and record medial ankle (lateral plantar sensory). Comparison with the contralateral side is required, using identical distances between the stimulating and recording sites
5. Sural sensory response, stimulating posterior calf, recording posterior ankle
6. Tibial and peroneal F responses
7. H reflexes, bilateral studies (may be abnormal in S1 radiculopathy or polyneuropathy but not in tarsal tunnel syndrome)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree