Chapter 9 The Abnormal EEG
An EEG is considered abnormal if it has findings known to be associated with a pathologic or disease state. As discussed in Chapter 8, “The Structure and Philosophy of the EEG Report,” this distinction is designed to prevent the interpreter from calling an EEG abnormal simply because it includes a finding that “looks unusual” or is uncommon, because uncommon findings may not be abnormal.
EEG abnormalities can be categorized in a variety of ways. Abnormalities may fall into the categories of 1) abnormal expressions of normally occurring rhythms (e.g., asymmetries of normal rhythms), 2) inherently abnormal rhythms (e.g., “slow” delta and theta rhythms in an adult who is awake), 3) certain repetitive or periodic patterns (e.g., burst-suppression patterns), 4) epileptiform abnormalities (spikes, sharp waves, etc.), and 5) abnormal “super-architecture” (e.g., abnormal sleep state cycling). These various abnormality types are discussed in the following sections. The first two abnormality families, abnormalities of normal rhythms and abnormal rhythms, are discussed by frequency range, starting with slow activity. Basic epileptiform abnormalities are discussed in this chapter. Various epilepsy syndromes and the EEG findings associated with them are discussed in Chapter 10, “The EEG in Epilepsy.”
ABNORMALITIES OF SLOW-WAVE (DELTA AND THETA) ACTIVITY
Descriptive Parameters for Slow Waves
Slow-wave abnormalities can be defined in multiple domains. The most obvious descriptor of a slow wave is its location. A slow wave may occur focally, such as in the left anterior temporal area or the right occipital area. Slowing may occur in broader regions, such as in the right posterior quadrant, in “anterior brain regions,” or over a whole hemisphere (see Figures 9-1 and 9-2). Such regional slowing can be considered a subset of focal slowing. Finally, slowing may also be diffuse or generalized.
Slow waves may be rhythmic or irregular (nonrhythmic). When there is a tendency to rhythmicity but the waves cannot be considered truly rhythmic, the intermediate term “semirhythmic” may be used (see Figure 9-3). Slow waves can be of varying amplitude. If slowing is only observed in a certain sleep stage, such as drowsiness or slow-wave sleep, this fact should be described. Slow waves may occur intermittently (in brief runs or bursts) or continuously (in long, continuous runs with few pauses). These different parameters are worth remembering and should usually be included in the written description of slow-wave activity.
| Parameter | Examples |
| Rhythmicity: | Irregular versus semirhythmic versus rhythmic |
| Amplitude: | High voltage versus low voltage |
| Sleep Stage Specificity: | Seen in wakefulness versus drowsiness versus sleep |
| Continuity: | Intermittent versus continuous |
| Localization: | Focal versus regional versus generalized |
Focal Slowing
Focal slow waves are the classic sign of a lesion in the cerebral hemispheres. Before the era of modern neuroimaging, the electroencephalogram was an important tool for the localization of cerebral tumors. Today the magnetic resonance imaging (MRI) scanner has moved to the forefront in localizing tumors, but the EEG may still play an important role in identifying certain types of focal lesions that may or may not be evident on neuroimaging. The EEG has the advantage over imaging studies of identifying areas of electrical abnormality which may be “nonanatomical,” that is, functional abnormalities of the brain that may not be visible on an MRI or computed tomography (CT) scan. Examples of “nonanatomical” slowing may include postictal slowing (see Figure 9-4), slowing from trauma that has not caused an MRI lesion (see Figure 9-5), or even migraine (discussed subsequently).
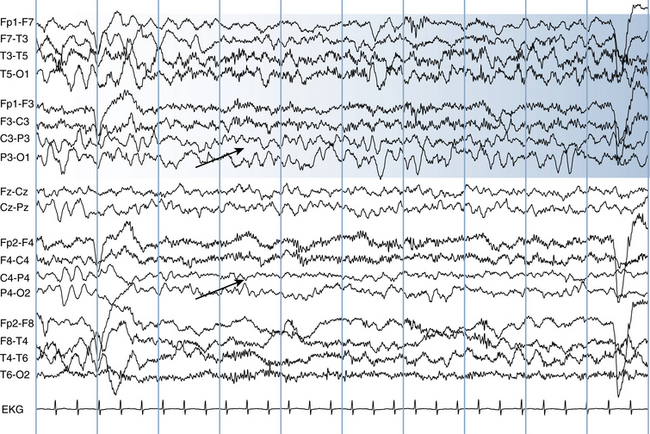
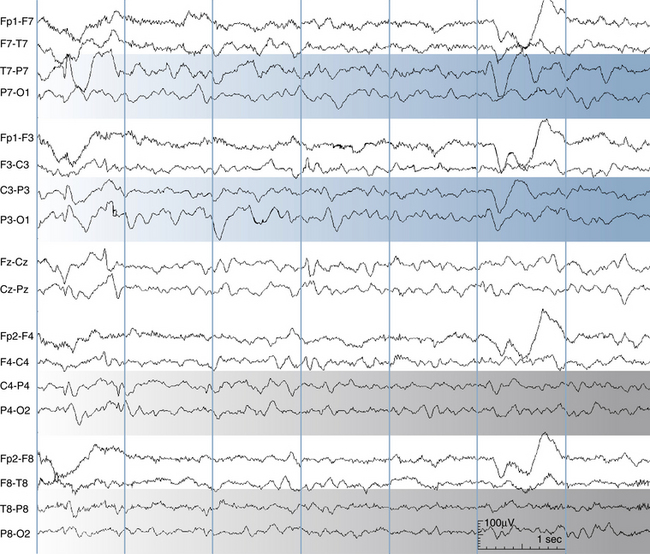
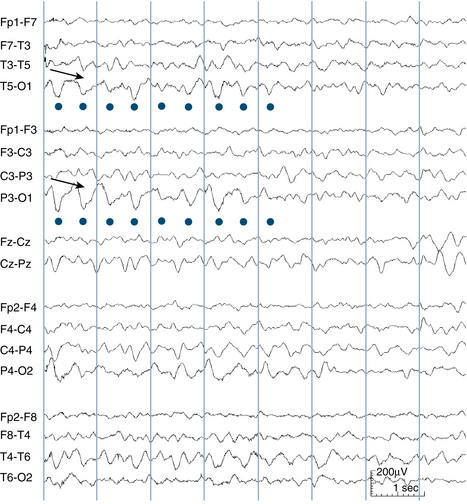
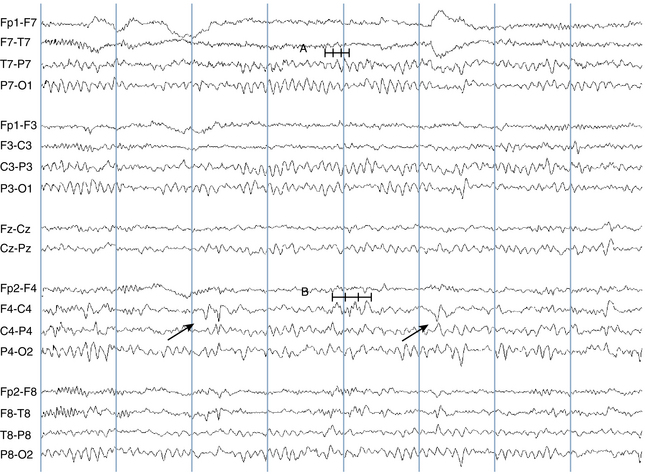
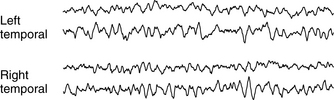
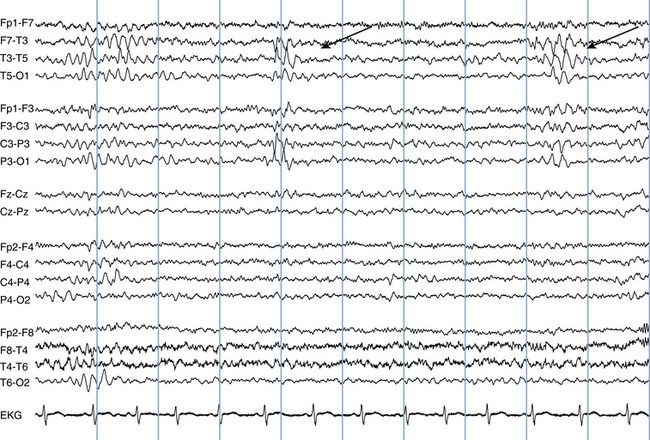
Focal slow waves may mark an area of previous, rather than acute, injury. Brain lesions that cause focal slowing in the absence of epileptiform activity may not necessarily be prone to seizures. Figures 9-6 and 9-7 show a left temporal slow wave abnormality; the perinatally acquired lesion causing the slow wave is shown in Figure 9-8. Figure 9-9 shows a subtle right occipital slow wave brought on by hyperventilation. If asymmetric slowing is only seen during hyperventilation, especially when the asymmetry is relatively mild as seen in this example, it is less likely to be associated with pathology than spontaneously occurring slow-wave asymmetries. Slow-wave asymmetries that alternate sides, whether spontaneous or elicited by hyperventilation, are much less likely to be clinically significant.
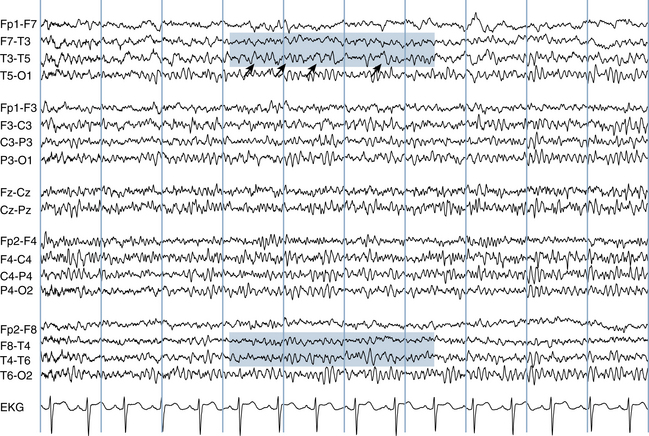
Figure 9-6 Close comparison of the temporal areas (shaded areas) shows an asymmetry of slow activity with increased theta waves on the left as a result of an old perinatal injury to the left temporal lobe tip in a 17-year-old girl. The arrows indicate individual theta waves in the left temporal area. The patient’s scan is shown in Figure 9-8. The lesion resulted in complex partial seizures.
Focal slow-wave abnormalities have generally been associated with deeper lesions located at the level of the deep white matter (as opposed to more superficial gray matter lesions), although exceptions to this rule do occur. As discussed next, more superficial abnormalities of cerebral cortex are classically associated with decreases in beta activity.
Intermittent Rhythmic Delta Activity
Frontal Intermittent Rhythmic Delta Activity and Occipital Intermittent Rhythmic Delta Activity
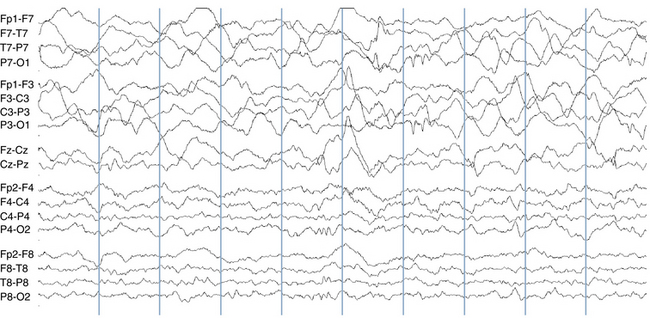
The term intermittent rhythmic delta activity (IRDA) refers to rhythmic delta activity occurring in brief bursts, usually lasting no longer than a few seconds, typically located either frontally or occipitally (see Figure 9-10). In some examples the bursts can be more generalized (see Figure 9-11), and occasionally they can be asymmetrical. IRDA is a pattern typically seen in wakefulness and is usually associated with processes of mild to moderate severity. Keeping in mind that the patient generally must attain some level of wakefulness to manifest frontal (FIRDA) or occipital (OIRDA) IRDA, these patterns would not be expected in patients whose recordings are restricted to more deeply sedated or comatose states.
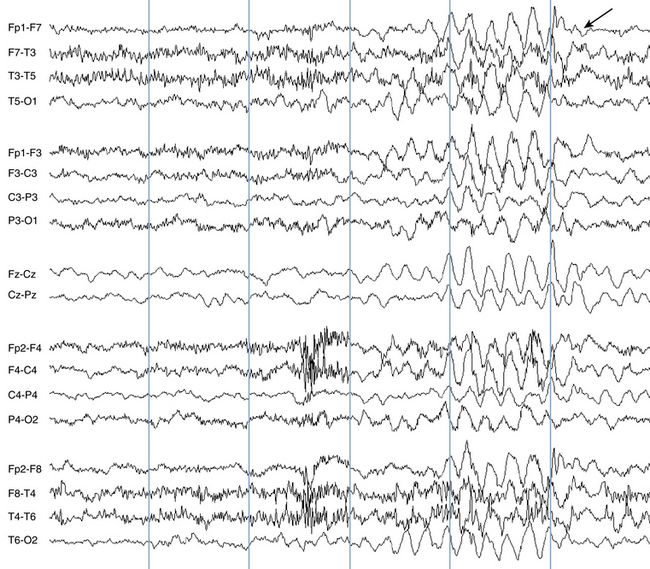
Figure 9-11 Compared with Figure 9-10, this burst of intermittent rhythmic slow (arrow) has a more diffuse (rather than frontal) distribution. It is seen equally well in the anterior and posterior channels.
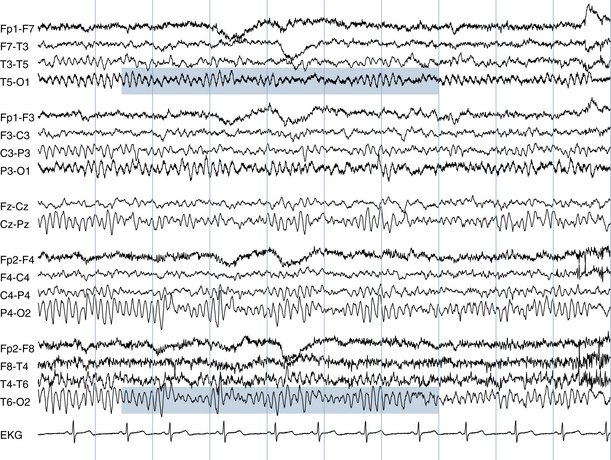
Temporal Intermittent Rhythmic Delta Activity
Temporal IRDA (TIRDA) should be considered separately from FIRDA and OIRDA. The presence of intermittent, rhythmic trains of delta activity in either temporal lobe has been associated with temporal lobe epilepsy (see Figure 9-12). Furthermore, the side of the TIRDA, which is usually unilateral, indicates the side of the lesion if one is present. This localizing property of TIRDA distinguishes it from the major types of IRDA (FIRDA and OIRDA). Thus, unlike FIRDA and OIRDA, TIRDA is considered a potentially epileptogenic abnormality and has localizing value.
Occipital Intermittent Rhythmic Delta Activity in Childhood Absence Epilepsy
A specific type of occipital intermittent rhythmic delta activity is seen in children with childhood absence epilepsy. Intermittent rhythmic 3-Hz delta activity, similar to OIRDA, can be seen in what can be either brief or prolonged runs in the occipital area in children who have childhood absence epilepsy. This type of rhythmic delta activity distinguishes itself from typical examples of OIRDA in that the runs can be quite prolonged, lasting many seconds.
Generalized or Diffuse Slowing
In general, theta and delta rhythms are not expected in the waking adult EEG. In younger patients; however, theta waves may be seen in the normal waking EEG. The range of normal posterior rhythms in childhood may serve as a useful reminder that theta frequencies are commonplace in the EEG of the awake child (see Table 2-2 in Chapter 2, “Visual Analysis of the EEG).” For instance, in individuals young enough that a posterior rhythm of 7 Hz is considered normal, other 7-Hz rhythms may also be seen elsewhere in the normal waking EEG.
The list of pathologic states that can cause diffuse slow-wave activity is long and includes almost any abnormal state that can cause a diffuse cerebral disturbance. The most common causes are postictal (postseizure) states, postanoxic states, diffuse traumatic injuries, infectious or inflammatory processes of the nervous system, toxic states related to drugs or other metabolic derangements (hepatic, renal, etc.), and a large number of other processes that have the potential to affect large portions of the cerebrum. Most of the many possible causes of coma are also on the list of possible causes of diffuse slowing in the EEG. For this reason, it is not feasible for the electroencephalographer to give a specific differential diagnosis for this pattern in the report. Often the interpretation will summarize the possible etiologies as a “diffuse cerebral disturbance” or a “diffuse encephalopathy.” The interpretation may also specifically discuss any clinical entities that have been questioned in the clinical history. EEG patterns in coma, many of which consist of slow-wave patterns, are discussed in further detail in Chapter 12, “Electroencephalographic Patterns in Stupor and Coma.”
Migraine
Because it is such a common disorder, the role of the EEG in migraine merits a separate discussion. A large number of abnormalities have been described in patients with common forms of migraine (“common” or “classic” migraine) between migraine attacks, so-called interictal EEG abnormalities in migraine. Many of these claims have been challenged because of the lack of well-controlled studies. The main problem is that the high frequency of migraine in the general population increases the chance that an individual who has any particular EEG abnormality may also incidentally have migraine. Some authors have claimed that focal slowing, and even epileptiform activity, are seen with increased frequency interictally in migraine patients. The “high-frequency photic response” (the ability to maintain a photic driving response at particularly high flash stimulation frequencies) has also been described in migraine patients. None of these phenomena, however, has been clearly proved to have an incidence in migraine patients above that seen in the general population. Because there are no EEG abnormalities that have proved to be useful in helping to diagnose uncomplicated migraine patients between attacks, EEG is not recommended as part of the routine evaluation of migraine patients. The EEG may be indicated, however, in the rare cases in which there is a question that a headache symptom may represent an epileptic seizure phenomenon.
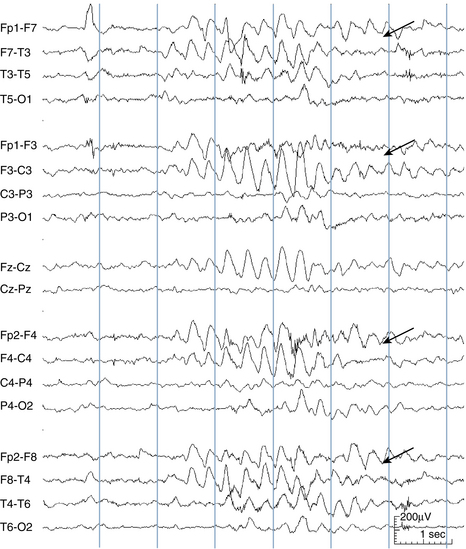
Complicated Migraine
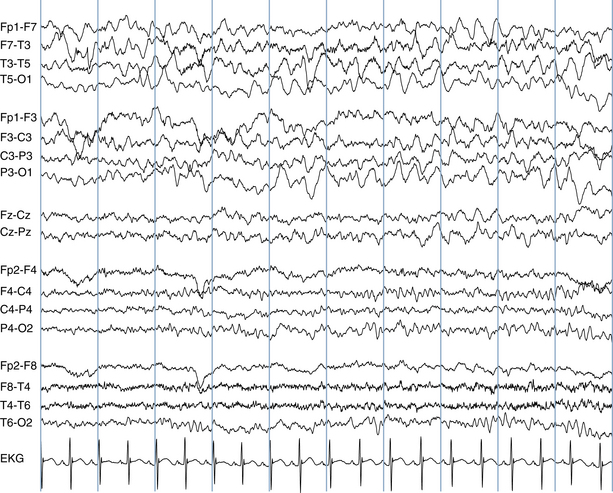
Focal slowing, either rhythmic or irregular, may be seen during the course of complicated migraine attacks. Figure 9-13 shows an example of high-voltage irregular slowing over the left hemisphere during an attack of hemiplegic migraine (a rare type of complicated migraine) in a 12-year-old girl. Confusional migraine, another rare type of complicated migraine that occurs predominantly in children, may cause bilateral slowing in the EEG. In some cases, migraine with visual aura can cause slowing during an attack, particularly in the posterior quadrants, although in many cases the EEG is not particularly remarkable during attacks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree