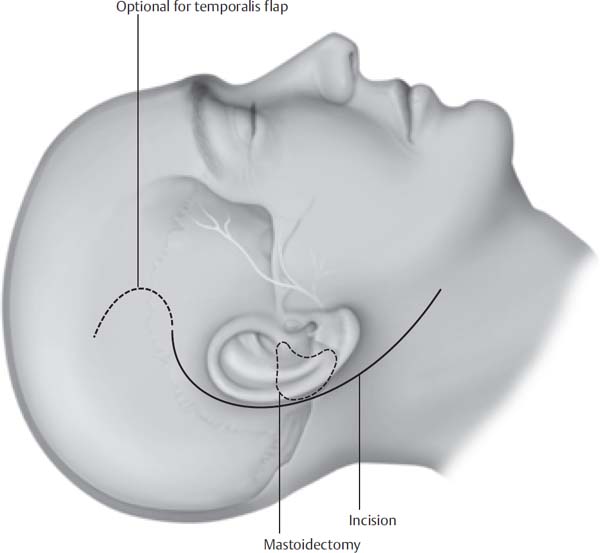
10 The infratemporal fossa type A approach allows safe access to the infralabyrinthine temporal bone, petrous apex, mandibular fossa, and posterior infratemporal fossa. It is a combination craniotemporal-cervical approach and requires anterior transposition of the facial nerve. This approach is used primarily for removal of glomus jugulare tumors; however, extensive cholesteatomas involving the internal auditory canal and petrous apex, lower cranial nerve neuromas, and carotid artery aneurysms may be approached in a similar manner. Ugo Fisch initial proposed a classification system for categorization of these tumors (Table 10.1). This classification system is based on the extent of temporal bone involvement and intracranial extension of the tumor. Other classification systems have been proposed (Tables 10.2 and 10.3), but the Fisch system is still the most commonly used system. Fisch first described the infratemporal approach to the infratemporal fossa and petrous apex in 1978. He subsequently reported the results of this technique in the management of 74 glomus jugulare tumors. The authors have made minor variations in the originally described technique. The basic steps are as follows: 1. Closure of the external auditory canal and removal of middle ear contents 2. Mastoidectomy with identification of the entire mastoid and tympanic segments of the facial nerve 3. Ligation of the jugular vein and identification of the internal carotid artery in the neck 4. Identification of the lower cranial nerves 5. Ligation or packing of the proximal sigmoid sinus 6. Transposition of the facial nerve from the geniculate ganglion to the parotid facial nerve 7. Removal of the tumor 8. Meticulous closure of the defect to prevent cerebrospinal fluid (CSF) leak With careful surgical planning, gross tumor removal is often attainable with minimal morbidity. Persistent mild facial nerve paresis may occur (House-Brackmann grade 2 to 3); however, grade 1 facial nerve function can be achieved after facial nerve transposition. The risk of lower cranial nerve dysfunction is correlated with the size of the tumor and may present with postoperative dysphasia, hoarseness, or aspiration. Carotid artery involvement should prompt preoperative investigation of cerebral blood flow using balloon occlusion angiography. A thorough history and physical examination are essential. A history of flushing, palpitations, and hypertension may suggest a secreting paraganglioma. Approximately 1% of glomus jugulare tumors actively secrete catecholamines. We routinely perform a 24-hour collection of urine to test for vanillylmandelic acid, norepinephrines, or metanephrines. If the 24-hour urine test is positive, a workup for multiple paragangliomas is warranted because glomus jugulare tumors rarely secrete catecholamines. In addition, careful perioperative planning with secreting tumors is necessary to prevent potentially devastating complications during surgery from the sudden secretion of catecholamines. Table 10.1 Fisch Classification of Glomus Tumors Class A Limited to promontory of middle ear Class B Involves hypotympanum and mastoid, but cortical bone over the jugular bulb is intact Class C1 Tumor erodes carotid foramen, but does not involve the carotid artery Class C2 Tumor involves the vertical petrous carotid artery between the carotid canal and the carotid bend Class C3 Tumor extends along the horizontal petrous carotid artery but does not involve the foramen lacerum Class C4 Tumors extends across the foramen lacerum and the cavernous sinus Class De1 Displace posterior fossa dura <2 cm Class De2 Displace posterior fossa dura ≥2 cm Class Di1 Intradural extension <2 cm Class Di2 Intradural extension ≥2 cm Class Di3 Neurosurgically unresectable Both computed tomography (CT) and magnetic resonance imaging (MRI) with gadolinium should be utilized to fully evaluate the lesion. Bony architecture can be best appreciated in detail with CT, and involvement of the fallopian canal, petrous carotid artery, and the caroticojugular spine can be accurately evaluated. MRI with gadolinium contrast can best define soft tissue involvement and any intracranial involvement. In addition, MRI is extremely helpful in determining the status of the carotid artery in relationship to the tumor as well as the involvement of the cavernous sinus, infratemporal fossa, and sigmoid sinus. Cerebral angiography with embolization is recommended for all tumors greater than Fisch class C1. Embolization can decrease intraoperative blood loss considerably and entail less blood in the operative field. Balloon occlusion of the internal carotid artery should be considered if preoperative imaging demonstrated possible involvement of the carotid artery. A slight risk of cerebrovascular accident is associated with balloon occlusion and should be taken into account. Table 10.2 De la Cruz Classification Scheme for Glomus Tumors Anatomic Classification Surgical Approach Tympanic Transcanal Hypotympanic Mastoid-extended facial recess Jugular bulb Mastoid-neck (fallopian bridge technique or partial facial nerve rerouting) Carotid artery Infratemporal fossa Transdural Infratemporal fossa/intradural Table 10.3 Glasscock and Jackson Classification of Glomus Jugulare Tumors Type I Small tumor involving the jugular bulb, middle ear, and mastoid Type II Tumor extending under the internal auditory canal; may have intracranial extension Type III Tumor extending into petrous apex; may have intracranial extension Type IV Tumor extending beyond the petrous apex into the clivus or infratemporal fossa; may have intracranial extension Approximately 10% of patients present with multiple tumors. If multiple tumors are suspected, a whole-body octreotide scan is a useful screening tool. Although exceedingly rare, metastasis will be appreciated with an octreotide scan. Preoperative antibiotics are administered and continued for 24 hours. Facial nerve and lower cranial nerve monitoring is performed on all cases. Glossopharyngeal electromyography (EMG) monitoring electrodes are placed. Long-acting muscle relaxants are avoided to prevent interference with cranial nerve monitoring. A lumbar drain may be placed in tumors with intracranial extension to decrease the incidence of postoperative CSF leak. The patient should be typed and screened for at least 4 units of blood. Autologous blood and the use of a cell-saver can reduce the amount of donor blood used. A thorough knowledge of temporal bone, jugular foramen, and cervical anatomy are essential to safely perform an infratemporal craniotomy. The anatomy of the temporal bone may be distorted due to tumor involvement. For instance, the vertical facial nerve may be displaced more laterally than usual due to lateral tumor extension. The middle ear space is often filled with tumor and covers the typical landmarks. Adequate preoperative imaging and preoperative planning can prevent complications in these incidences. The internal carotid artery is usually intimately involved with tumor, requiring a familiarity with the anatomy. The internal carotid artery is initially identified in the neck and can be differentiated from the external carotid artery due to the lack of cervical arterial branches. Superiorly, the genu of the petrous internal carotid artery is medial and superior to the orifice of the eustachian tube. The caroticotympanic branch originates from the ascending petrous internal carotid artery and should not be avulsed during dissection. The lower cranial nerves exit through the pars nervosa of the jugular foramen. The medial jugular bulb is preserved to create a safe plane between the lower cranial nerves and the tumor. The lower cranial nerves may be injured with overzealous packing of the inferior petrosal sinus opening into the medial wall of the jugular bulb. When packing or ligating the sigmoid sinus, the vein of Labbé should not be occluded. This can be prevented by packing the sinus distal to the superior petrosal sinus. The patient is placed in the supine position with the head turned away from the operative site. Facial nerve and glossopharyngeal EMG electrodes are placed for intraoperative monitoring. A C-shaped incision is performed two fingerbreadths from the postauricular sulcus, down to the mastoid tip, and continuing into the neck two fingerbreadths below the angle of the mandible (Fig. 10.1). An incision is then made through the periosteum posterior along the linea temporalis and then inferior to the mastoid tip. The periosteum is elevated anteriorly and the external auditory canal is transected just medial to the bony-cartilaginous junction. The skin of the external auditory canal is then elevated away from the underlying cartilage. The skin of the canal is then everted and closed with interrupted 4–0 nylon sutures. The anterior-based periosteal flap is then closed over the canal to provide an extra layer of closure (Fig. 10.2). This results in a blind sac closure of the external auditory canal. The skin of the canal, tympanic membrane, malleus, and incus are now removed after the incudostapedial joint has been disarticulated. Fig. 10.1 The incision is made 4 cm postauricular. The apex of the incision is at the mastoid tip. The incision extends into the neck, two fingerbreadths below the mandible. An optional superior extension can be done if a temporalis flap is needed.
The Fisch Infratemporal Fossa Approach: Type A
 Preoperative Workup
Preoperative Workup
 Surgical Anatomy
Surgical Anatomy
 Surgical Technique
Surgical Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


