The Trigeminal Nerve
The trigeminal, or fifth cranial, nerve (CN V) has a large sensory part that innervates the face, teeth, oral and nasal cavities, the scalp back to the vertex, and the intracranial dura; and a much smaller motor part that innervates the muscles of mastication. The sensory component has 3 divisions: the first, or ophthalmic division (CN V1), the second or maxillary division (CN V2), and the third or mandibular division (CN V3). The motor and principal sensory nuclei are located in the midpons. The spinal tract and nucleus, which subserve pain and temperature, extend from the pons down into the upper cervical spinal cord. The mesencephalic root receives proprioceptive fibers.
Examination of the Motor Functions
Assessment of trigeminal motor function is accomplished by examining the muscles of mastication. Bulk and power of the masseters and pterygoids can be gauged by palpating these muscles as the patient clenches the jaw. An effective technique is to place the examining fingers along the anterior, not lateral, border of the masseters bilaterally. When the jaw is clenched the fingers will move forward; this movement should be symmetric on the two sides. Unilateral trigeminal motor weakness causes deviation of the jaw toward the weak side on opening (Figure 11.1). Subtle deviation on jaw opening is often the earliest clue to the presence of an abnormality. It is occasionally difficult to be certain whether the jaw is deviating or not. Note the relationship of the midline notch between the upper and lower incisor teeth; it is a more reliable indicator than lip movement. The tip of the nose and the interincisural notches should line up. A straightedge against the lips can help detect deviation. Another useful technique is to draw a vertical line across the midline upper and lower lips. Failure of the two vertical marks to match when the jaw is opened indicates deviation. If there is any suggestion of a problem, have the patient move the jaw from side to side. With unilateral weakness the patient is unable to move the jaw contralaterally. With facial weakness there may be apparent deviation of the jaw, and of the tongue, because of the facial asymmetry. Holding up the weak side manually will sometimes eliminate the pseudodeviation.
Other techniques for examining trigeminal motor function include having the patient protrude and retract the jaw, noting any tendency toward deviation; and having the patient bite on tongue depressors with the molar teeth, comparing the impressions on the two sides and comparing the difficulty of extracting a tongue depressor held in the molar teeth on each side.
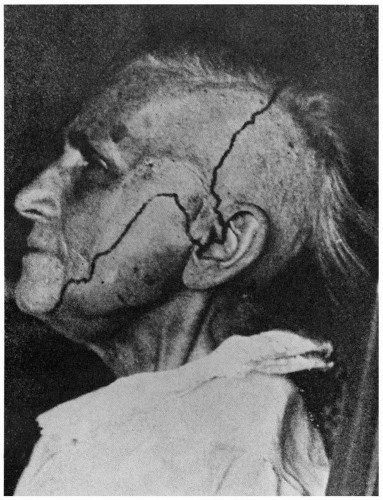
Unilateral weakness of CN V innervated muscles generally signifies a lesion involving the brainstem, Gasserian ganglion, or the motor root of CN V at the base of the skull. Severe bilateral weakness of the muscles of mastication with inability to close the mouth (dangling jaw) suggests
motor neuron disease, a neuromuscular transmission disorder, or a myopathy. With significant atrophy of one masseter, a flattening of the jowl on the involved side may be apparent (Figure 11.2). With temporalis atrophy there may be a hollowing of the temple. Rarely, fasciculations or other abnormal
involuntary movements occur. There is no reliable or realistic method for examination of the other muscles supplied by CN V. Because of bilateral innervation, unilateral upper motor neuron lesions rarely cause significant impairment of trigeminal motor function. There may be mild, transitory unilateral weakness. The amount of involvement depends on the extent of decussation. In bilateral supranuclear lesions there may be marked paresis.
motor neuron disease, a neuromuscular transmission disorder, or a myopathy. With significant atrophy of one masseter, a flattening of the jowl on the involved side may be apparent (Figure 11.2). With temporalis atrophy there may be a hollowing of the temple. Rarely, fasciculations or other abnormal
involuntary movements occur. There is no reliable or realistic method for examination of the other muscles supplied by CN V. Because of bilateral innervation, unilateral upper motor neuron lesions rarely cause significant impairment of trigeminal motor function. There may be mild, transitory unilateral weakness. The amount of involvement depends on the extent of decussation. In bilateral supranuclear lesions there may be marked paresis.
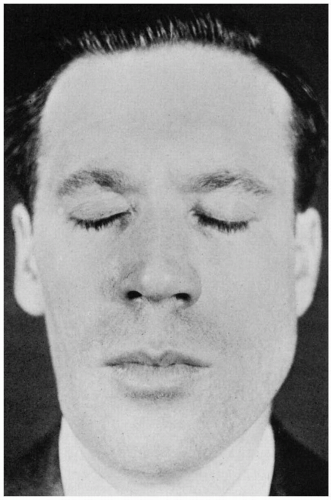
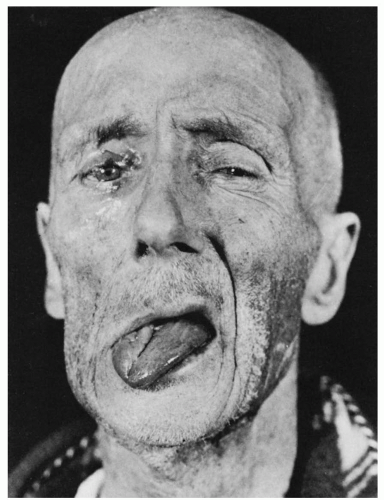 FIGURE 11.1 • Infranuclear paralysis of the right trigeminal, facial, and hypoglossal nerves in a patient with metastatic carcinoma, showing deviation of the tongue and mandible to the right. |
Examination of the Sensory Functions
In testing facial sensation, touch, pain, and occasionally temperature are examined in the same manner as elsewhere on the body, searching for areas of altered sensation. It is better to ask the patient if the stimuli feel the same on the two sides, rather than suggesting they might feel different. Sometimes it is useful to examine the nostrils, gums, tongue, and insides of the cheeks. Proprioception cannot be adequately tested, but one can test for extinction and the ability to identify figures written on the skin.
There are three common exercises in evaluating facial sensation: (a) determining whether sensory loss is organic or nonorganic, (b) determining which modalities are involved, and (c) defining the distribution. Complaints of facial numbness are common, and not all are organic. However, real facial sensory loss can be a serious finding, occasionally signifying underlying malignancy. The various methods and tricks for detecting nonorganic sensory loss are not entirely reliable, and this diagnosis should be made with caution. Patients with nonorganic sensory loss may have a demarcation of the abnormal area at the hairline rather than the scalp vertex. On the lower face functional sensory loss tends to follow the jaw line and involve the notch over the masseter muscle, which is not trigeminal innervated (Figure 11.3). On the trunk, organic sensory loss typically stops short of midline because of the overlap from the opposite side, and splitting of the midline suggests
nonorganicity. This finding is not reliable on the face because there is less midline overlap on the face, so organic facial sensory loss may extend to the midline. The corneal and sternutatory reflexes should be normal in nonorganic sensory loss. Splitting of vibration along the midline is reputedly a nonorganic sign. Because the frontal bone and mandible are single bones, there should be no difference in vibratory sensibility on either side of midline. Patients who report a difference in vibratory sensibility on testing just to either side of midline may have nonorganic sensory loss. The reliability of this sign has not been validated; it can be misleading. Other signs suggestive of nonorganicity include dissociation between pinprick and temperature, variability from trial to trial, history of hypochondriasis, secondary gain, la belle indifference, nonanatomical sensory loss, and changing boundaries of hypalgesia.
nonorganicity. This finding is not reliable on the face because there is less midline overlap on the face, so organic facial sensory loss may extend to the midline. The corneal and sternutatory reflexes should be normal in nonorganic sensory loss. Splitting of vibration along the midline is reputedly a nonorganic sign. Because the frontal bone and mandible are single bones, there should be no difference in vibratory sensibility on either side of midline. Patients who report a difference in vibratory sensibility on testing just to either side of midline may have nonorganic sensory loss. The reliability of this sign has not been validated; it can be misleading. Other signs suggestive of nonorganicity include dissociation between pinprick and temperature, variability from trial to trial, history of hypochondriasis, secondary gain, la belle indifference, nonanatomical sensory loss, and changing boundaries of hypalgesia.
Examination of the Reflexes
The corneal, sternutatory, and jaw reflexes are the reflexes most often assessed in evaluating the trigeminal nerve. Many other reflexes have been described, but they are of limited value and are seldom used. The afferent limbs of these reflexes are trigeminal mediated. In some the efferent limb is also trigeminal (e.g., the jaw jerk); in others the efferent limb is executed through connections with CN III, CN VII, or other pathways.
The Jaw, Masseter, or Mandibular Reflex
To elicit the jaw (or jaw muscle) reflex, the examiner places an index finger or thumb over the middle of the patient’s chin, holding the mouth open about midway with the jaw relaxed, then taps the finger with the reflex hammer. The response is an upward jerk of the mandible. Other methods to elicit the reflex include tapping the chin directly and placing a tongue blade over the tongue or the lower incisor teeth and tapping the protruding end. All of these cause a bilateral response. A unilateral response may sometimes be elicited by tapping the angle of the jaw or by placing a tongue blade over the lower molar teeth along one side and tapping the protruding end.
The afferent impulses of this reflex are carried through the sensory portion of the trigeminal nerve, possibly through the mesencephalic root, and the efferent impulses through its motor portion; the reflex center is in the pons. In normal individuals, the jaw jerk is minimally active or absent. Its greatest use is in distinguishing limb hyper-reflexia due to a cervical spine lesion (where the jaw jerk is normal) from a state of generalized hyper-reflexia (where the jaw jerk is increased along with all of the other reflexes). The jaw reflex is exaggerated with lesions affecting the corticobulbar pathways above the motor nucleus, especially if bilateral, as in pseudobulbar palsy or amyotrophic lateral sclerosis (ALS). It is sometimes possible to elicit extra beats or jaw clonus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree