POTENTIAL FOR PREVENTION
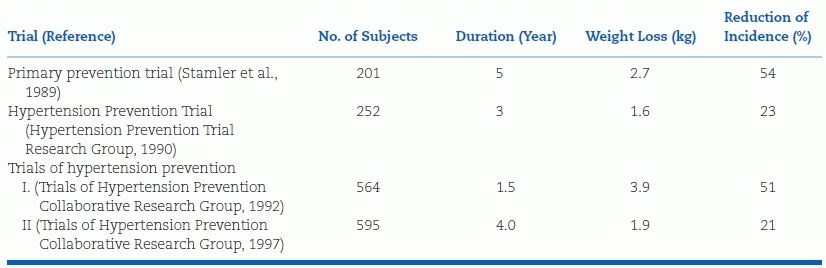
Lifestyle modifications may prevent or at least delay the onset of hypertension. Three long-term, well-controlled preventive trials involving subjects with high–normal blood pressure, i.e., prehypertension, have shown that individual and combined lifestyle changes lower blood pressure and reduce the incidence of hypertension, as summarized in Table 6-2 (Hypertension Prevention Trial Research Group, 1990; Stamler et al., 1989; Trials of Hypertension Prevention Collaborative Research Group, 1992, 1997).
TABLE 6-2 Trials of Lifestyle Modifications on the Incidence of Hypertension
The effects of multiple lifestyle changes have also been examined in two groups of patients with somewhat higher BPs. The Trial of Nonpharmacologic Interventions in the Elderly (TONE) enrolled 975 men and women aged 60 to 80 years whose hypertension was controlled on one antihypertensive drug (Whelton et al., 1998). They were randomly assigned to reduced sodium intake, weight loss, both of these, or no intervention (i.e., usual care). After 3 months, their antihypertensive drug was withdrawn. Over the ensuing 30 months, the proportion of patients who remained normotensive without antihypertensive drugs was only 16% in those on usual care, more than 35% in those on one of the two interventions, and 43.6% in those on both interventions (Fig. 6-1). These impressive effects were achieved with relatively small amounts of dietary sodium reduction (an average of 40 mmol/day) or weight reduction (an average of 4.7 kg).
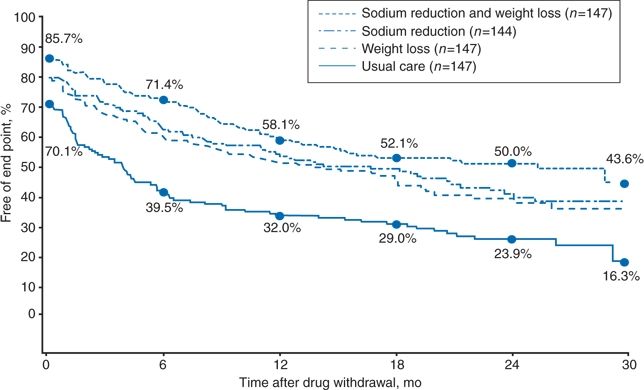
FIGURE 6-1 Percentages of the 144 participants assigned to reduced sodium intake, the 147 assigned to weight loss, the 147 assigned to reduced sodium intake and weight loss combined, and the 147 assigned to usual care (no lifestyle intervention) who remained free of cardiovascular events and high BP and in whom no antihypertensive agent was prescribed during follow-up. (Modified from Whelton PK, Appel LJ, Espeland MA, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons. JAMA 1998;279:839–846.)
Another trial involved 412 adults whose average age was 48 years and who had a BP between 120 and 159 mm Hg systolic and 80 to 95 mm Hg diastolic (Sacks et al., 2001). They were randomly given one of two already prepared diets, one typical of the U.S. diet, i.e., the controls, and the other composed of more fruits, vegetables, and low-fat dairy foods, the Dietary Approaches to Stop Hypertension (DASH) diet portrayed in Table 6-3. In addition, they were randomly given one of three levels of sodium intake: High (150 mmol/day), intermediate (100 mmol/day), or low (50 mmol/day).
TABLE 6-3 DASH Diet
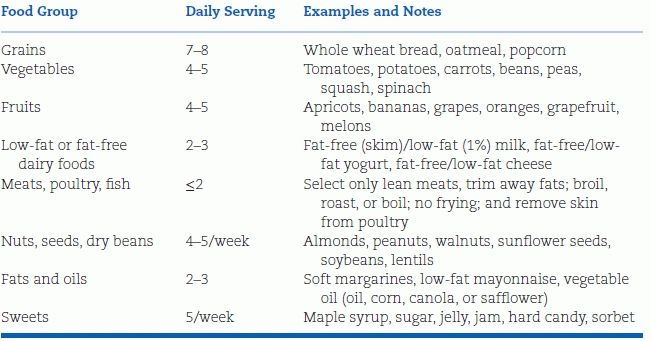
DASH eating plan available at: http://www.nhibi.nih.gov/health/public/heart/hpb/dash/new_dash.pdf
Each diet was consumed for 30 consecutive days, while weight was kept constant. Figure 6-2 shows significant falls in systolic blood pressure (SBP) noted with the DASH diet at every level of sodium intake as compared to the control diet and significant falls in SBP with progressively lower sodium intakes on either diet. The effects were seen in normotensives and hypertensives, men and women, blacks and nonblacks, and were accompanied by falls in diastolic blood pressure (DBP) as well.
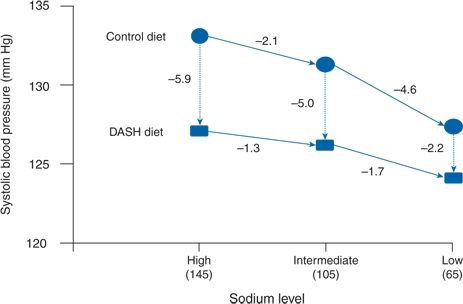
FIGURE 6-2 Reduction of SBP by Dietary Approaches to Stop Hypertension, the DASH diet, and reduced sodium intake. The mean SBP are shown for the high-sodium control diet. The three dietary sodium levels are expressed in terms of millimoles per day. The solid lines indicate changes in BP for various sodium levels, and the dotted arrows show the mean differences in BP between the two diets at each level of sodium intake. The order in which participants were given the sodium levels was random, with a crossover design. There was a significant difference in SBP between the high-sodium and low-sodium phases of the control diet (mean, −6.7 mm Hg) and the DASH diet (mean, −3.0 mm Hg). (Modified from Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. N Engl J Med 2001;344:3–10.)
As impressive as these results are, they may not be applicable to the “real” world since the latter two were short studies that were tightly controlled. A more realistic view of what can be expected comes from the PREMIER trial wherein participants were assigned to the DASH diet but prepared their own meals (Elmer et al., 2006). Not surprisingly, at the end of 18 months, neither the extent of dietary change nor the reduction in BP was as great as seen in the original DASH trial. The additional fall in BP compared to the group only given advice was −1.1/–0.9 mm Hg.
Although there is no doubt that the unhealthy lifestyle of people in most developed societies contribute to our high incidence of hypertension, diabetes, and cardiovascular disease (Moodie et al., 2013), multiple barriers make correction of these unhealthy practices difficult. As noted by Chobanian et al. (2003):
Barriers to prevention include cultural norms: Insufficient attention to health education by health care practitioners; lack of reimbursement for health education services; lack of access to places to engage in physical activity; larger servings of food in restaurants; lack of availability of healthy food choices in most schools, worksites, and restaurants; lack of exercise programs in schools; large amounts of sodium added to foods by the food industry and restaurants; and the higher cost of food products that are lower in sodium and calories. Overcoming the barriers will require a multipronged approach directed not only at high-risk populations but also to communities, schools, worksites, and the food industry.
Obviously, removal of these barriers will be difficult and will require major environmental changes, which demand a political advocacy and governmental financing that is sorely lacking.
As rational as lifestyle modifications seem to be, both for prevention and treatment of hypertension, their value must be put into perspective. As Pickering (2004) notes:
Given that healthcare practitioners have limited resources to improve hypertension control, it would seem appropriate to focus on the intervention that has the greatest chance of success; there can be little doubt that drug treatment wins hands down. This conclusion is not intended to negate the importance of lifestyle changes such as the DASH diet, and patients should certainly be encouraged to adopt them, but if behavioral medicine is to progress, practitioners need to find more cost-effective methods for instituting and maintaining behavior change. In the mean time, doctors are still going to need to take out the prescription pad.
PROTECTION AGAINST CARDIOVASCULAR DISEASE
The larger issue of whether these lifestyle modifications will, in fact, reduce morbidity and mortality in hypertensive patients may never be settled. The difficulty of demonstrating such protection in the various therapeutic trials using much more potent antihypertensive drugs was described in Chapter 5. Other than for the dramatic impact that smoking cessation and the rapid weight loss achieved by bariatric surgery (Adams et al., 2012) have had upon cardiovascular disease, it may not be possible to document the efficacy of most lifestyle modifications, which are less potent and more difficult to monitor than is drug treatment (Harrap, 2012). Lifestyle modifications must be accepted on the evidence that they will lower the BP and other risk factors without risk and with a reasonable chance of adoption by most patients.
With recognition that only societal changes will lead to major changes, the effects of individual lifestyle modifications on hypertension will now be examined. In the latter part of the chapter, some maneuvers that are not “lifestyle” are covered since they are not antihypertensive drugs as are covered in the next chapter.
AVOIDANCE OF TOBACCO
Smoking cessation is the most effective, immediate way to reduce cardiovascular risk, adding 10 years to the life span of women who quit (Pirie et al., 2013). However, an effect on BP has not been generally thought to be involved in this risk reduction because chronic smokers as a group have a lower BP than do nonsmokers (Mikkelsen et al., 1997), likely because smokers weigh less than do nonsmokers. In addition, the role of a pressor effect of smoking was missed because of the almost universal practice of having smokers abstain from smoking for some time before measuring their BP, usually because medical facilities are smoke free. Thus, the significant, immediate, and repetitive pressor effect of smoking had been missed because it lasts for only 15 to 30 minutes after each cigarette. Only with ambulatory BP monitoring has the major pressor effect of smoking been recognized (Oncken et al., 2001). Smoking exacerbates the effects of hypertension on mortality (Ge et al., 2012), increasing arterial stiffness (Jatoi et al., 2007) and impairing nitric oxide (NO) synthase (Argacha et al., 2008).
Unfortunately, the rate of cigarette smoking in the U.S. has not continued to decrease while use of other tobacco products has gone up (Centers for Disease Control and Prevention [CDC], 2012a). The use of smokeless tobacco and cigars, if their smoke is inhaled, also increases the risk of myocardial infarction (Teo et al., 2006).
Hypertensives who use tobacco must be repeatedly and unambiguously told to quit and given assistance in doing so. Nicotine replacement therapies may help even if they cause sympathetic stimulation, and the partial nicotine agonist, varenicline, may help in relieving withdrawal symptoms and blocking the desire to continue smoking (Sobieraj et al., 2013). If the patient continues to smoke, all antihypertensive drugs except nonselective β-blockers may attenuate the smoking-induced rise in BP.
WEIGHT REDUCTION
Most adults in the U.S., as many as 80% of African American women, are overweight, defined as a BMI more than 25, and more than 30% are obese, defined as a BMI more than 30 (Ogden et al., 2014). The nature of modern life, with more caloric intake and less physical activity, engenders more obesity, which is now a worldwide epidemic (Swinburn et al., 2011), particularly ominous in children (Ogden et al., 2014). Any degree of weight gain, even to a level that is not defined as overweight, is associated with an increasing incidence of hypertension (Shihab et al., 2012) and, even more strikingly, of type 2 diabetes. As more completely described in Chapter 3, the hypertensive effect of weight gain is mainly related to increased abdominal or visceral fat (Ostchega et al., 2012), usually as part of the metabolic syndrome (Safar et al., 2013), accompanied by impaired endothelial function in turn associated with sympathetic activation, reduced NO synthesis, and adipocyte-derived factors (Nguyen Dinh Cat et al., 2011).
Despite increasing awareness of the problem, dietary habits among U.S. adult hypertensives continue to worsen (Mozaffarian et al., 2011). Because the maintenance of significant weight loss is so difficult for most who are obese, physicians, patients, and society at large must do more to prevent weight gain, particularly among children in whom obesity and the metabolic syndrome are increasing so rapidly (Ogden et al., 2014). Societal changes are needed to stop the epidemic.
Clinical Data
Once achieved, obesity is extremely hard to overcome, except by bariatric surgery. Even though significant weight loss can be achieved by multiple behavioral motivations (Unick et al., 2013), most success is short-lived, at least in part by persistence of appetite-stimulating hormones in the blood (Sumithran et al., 2011). In view of the limited success of diets and appetite-suppressing drugs, bariatric surgery is being more widely practiced (Vest et al., 2013).
Real prevention will most likely require societal changes that must be based on governmental restrictions, as attempted (apparently unsuccessfully) on the sale of super-sized sugar-loaded beverages (Fairchild, 2013). As noted by Gostin (2007):
Despite the undoubted political risks, should public health agencies push for strong measures to control obesity, perhaps even banning hazardous foods? The justification lies with the epidemic rates of overweight and obesity, the preventable morbidity and mortality, and the stark health disparities based on race and socioeconomic status. If the problem were related to pathogens, tobacco, or lead paint, most would support aggressive measures to protect innocent individuals from hazards created by others. But comfort foods also have hidden hazards—it is difficult to tell if they are laden with fat and, if so, what kind. Although the public dislikes paternalism, it is at least worth considering whether such an approach is ever justified to regulate harms that are apparently self-imposed, but also are deeply socially embedded and pervasively harmful to the public.
DIETARY SODIUM REDUCTION
No food in its natural state is high in sodium. Salt was originally added to preserve foods that spoil without refrigeration. Although infants do not prefer saltier liquids, the presence of increased salt in virtually all processed food quickly leads to an acquired preference. Food processors are able to bulk up their products with water held by the salt. Soft drink and beer drinkers are enticed to consume more fluid to quench the saltiness of food and bar condiments. Of the average daily sodium intake of 4,323 mg by U.S. men and of 2,918 mg by U.S. women (Yang et al., 2011), 77% comes from that added in the processing (Centers for Disease Control and Prevention, CDC, 2012b).
Rigid restriction of dietary sodium intake was one of the first effective therapies for hypertension (Kempner, 1948). However, after thiazides were introduced during the late 1950s and their mode of action was shown to involve a mild state of sodium depletion, both physicians and patients eagerly adopted this form of therapy in place of dietary sodium reduction. In discarding rigid salt restriction, physicians disregarded the benefits of modest reduction both for its inherent antihypertensive effect and for its potential of reducing diuretic-induced potassium loss.
Moderate dietary sodium reduction is advocated by most individual experts, national and international guideline reports, governmental health agencies, and medical organizations, including the American Heart Association (Pearson et al., 2013). Unfortunately, the one official U.S. document that prevents this desired societal change is the U.S. Food and Drug Administration regulation that continues to designate salt as “an ingredient recognized as safe (GRAS),” thereby allowing food processors to add as much salt as they wish. Unlike many other countries that have begun to address dietary sodium intake (Brinsden et al., 2014), the U.S. refuses to do so. As a consequence, the amount of sodium in fast foods sold in the U.S. is often more than twice the amount in the same item in the U.K. (Roehr, 2012). The CDC (CDC, 2012b) estimate that moderate reduction of dietary sodium could prevent as many as 11 million new cases of hypertension in the U.S., and Coxson et al. (2013) estimate a decrease of mortality of 0.7 and 1.2 million over 10 years.
Evidence for Antihypertensive Effect
Moderate sodium reduction to a level of 2.4 g/day (6 g NaCl per day, 100 mmol/day) has been shown to reduce blood pressure in hypertensives by a mean of 5.4/2.8 mm Hg (He et al., 2013) and to provide a possible preventative effect (Forman et al., 2012). An earlier meta-analysis showed a significant fall in BP, greater in hypertensives than in normotensives, that correlates with the degree of sodium reduction (He & MacGregor, 2003) (Fig. 6-3). This analysis was restricted to 26 trials that lasted 4 weeks or longer, but very similar results were found in their later analysis of 34 trials (He et al., 2013).
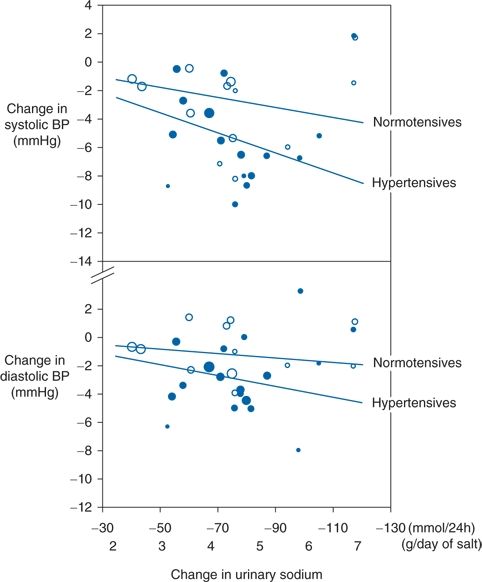
FIGURE 6-3 Relationship between the net change in 24-hour urinary sodium excretion and BP in a meta-analysis of 26 trials. Open circles, normotensive. Solid circles, hypertensives. The slope is weighted by the inverse of the variance of the net change in BP. The size of the circle is proportional to the weight of the trial. (Modified from He FJ, MacGregor GA. How far should salt intake be reduced? Hypertension 2003;42:1093–1099.)
In another meta-analysis of data from both normotensive and hypertensive subjects, Aburto et al. (2013a) showed an overall reduction of 3.4/1.5 mm Hg. In neither of the 2013 meta-analyses were any significant adverse effects seen in blood lipids, catecholamines, or renal function.
The likely inability to maintain enough dietary sodium reduction to achieve a meaningful effect on BP by most people over a long period of time has led to a concerted effort to convince food processors to reduce the amount of sodium added to processed foods and drinks, the source of about three-fourths of current sodium consumption (Frisoli et al., 2012). In the meantime, patients should be advised to read the label on processed products, avoiding those with more than 300 mg per portion. In addition, a number of books and Web sites, such as the American Heart Association Heart (heart.org), provide advice and recipes for lower-sodium diets.
Mechanisms of Antihypertensive Effect
Despite considerable research, neither the mechanisms by which excessive sodium intake raises BP nor the mechanisms by which moderate sodium restriction lowers BP are completely characterized (Kotchen et al., 2013). However, the structure and function of the heart and kidneys may be improved after prolonged, moderate sodium reduction: Left ventricular hypertrophy decreases (Rodriguez et al., 2011), glomerular hyperfiltration and proteinuria are reduced (Agarwal, 2012), arterial stiffness and oxidative stress are lessened (Hummel et al., 2012), and endothelial function improves (Jablonski et al., 2013).
Sodium Sensitivity
The fall in BP with reduced sodium intake tends to be greater in those with lower plasma renin and higher atrial natriuretic peptide levels (Melander et al., 2007). The BP sensitivity to sodium tends to be enhanced in hypertensives, blacks, and older people, all associated with lower renin, so that these patients tend to respond more to sodium reduction presumably because they have a lesser reactive increase in renin (Weinberger, 1996). In addition, this sensitivity is greater in adults who had a low birth weight (de Boer et al., 2008). Blacks, who are more likely to have been of low birth weight and therefore have impaired nephrogenesis, tend to be more sodium sensitive (Schmidlin et al., 2007). Compared to those who are salt resistant, more sodium-sensitive people developed hypertension over a 15-year follow-up (Barba et al., 2007), and they have more cardiovascular disease and shorter survival (Franco & Oparil, 2006), associated with less insulin resistance (Laffer & Elijovich, 2013).
Sodium sensitivity may have a genetic mechanism. In a study of 185 subjects, 55 of whom were hypertensive and 34 sodium sensitive, Carey et al. (2012) found polymorphisms in the sodium bicarbonate cotransporter gene that were closely associated with sodium sensitivity. An association with multiple genetic variants in the endothelial system was reported in a study of Chinese men (Defago et al., 2013).
Despite these associations, there seems to be no need to ascertain the individual patient’s degree of sodium sensitivity before recommending moderate sodium reduction, particularly as testing may not be reliable or reproducible (Gerdts et al., 1999). Those who respond more to sodium reduction likely are more sodium sensitive, but there is no harm, and as noted in Table 6-4, there are other potential benefits of moderate sodium reduction in all hypertensives. All should be encouraged to reduce their levels to the 100 mmol/day goal, particularly since there is no certain way to predict who will develop hypertension.
TABLE 6-4 Additional Benefits of Moderate Sodium Reduction
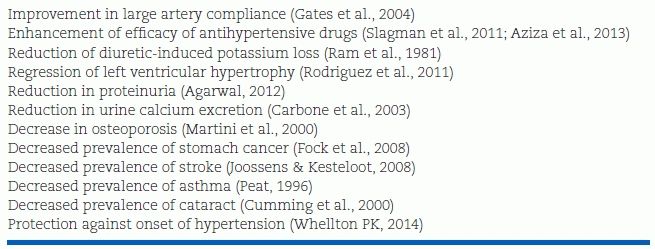
Additional Benefits of Sodium Reduction
In addition to lowering BP, other benefits have been observed with moderate sodium reduction, as summarized in Table 6-4.
Enhancement of Efficacy of Antihypertensive Drugs
Moderate sodium reduction clearly increases the antihypertensive efficacy of all classes of antihypertensive drugs, with the possible exception of calcium channel blockers, which have a mild natriuretic effect (Chrysant et al., 2000). Lower sodium intake improves the kinetic and dynamic effects of ARBs and β-blockers (Azizi et al., 2013). This potentiation was nicely documented in a randomized controlled trial (RCT) in 52 nondiabetic patients with nephropathy on an ACE inhibitor (Slagman et al., 2011). A lowering of dietary sodium intake from 186 to 106 mmol/day provided a greater reduction in blood pressure and proteinuria than did addition of an ARB.
Protection from Diuretic-Induced Potassium Loss
High levels of dietary sodium make patients more vulnerable to the major side effect of diuretic therapy, potassium loss. The diuretic inhibits sodium reabsorption proximal to that part of the distal convoluted tubule where secretion of potassium is coupled with sodium reabsorption under the influence of aldosterone. When a diuretic is given daily while the patient ingests large amounts of sodium, the initial diuretic-induced sodium depletion shrinks plasma volume, activating renin release and secondarily increasing aldosterone secretion. As the diuretic continues to inhibit sodium reabsorption, more sodium is delivered to this distal site. The increased amounts of aldosterone act to increase sodium reabsorption, thereby increasing potassium secretion; the potassium is swept into the urine.
With modest sodium reduction, less sodium is delivered to the distal exchange site, and therefore, less potassium is swept into the urine. This modest restriction should not further activate the renin–angiotensin–aldosterone mechanism to cause more distal sodium-for-potassium exchange, because that usually occurs only with more rigid sodium restriction.
Dissenting Views
There are a few dissenters to the value of such moderate sodium reduction. Their dissent is based on the possibility that such reduction may cause hazards that outweigh its benefits. These putative dangers include the following:
- Sodium reduction has not been shown to reduce cardiovascular morbidity or mortality in properly performed, controlled trials even if it lowers blood pressure. This complaint is valid, but it must be understood to pose an impossible burden. It is obvious that it is impossible to perform an RCT in 20,000 free-living subjects over 10 years as would be needed, as projected from studies on treatment of hypertensive patients with drugs. John Snow was correct to close the Broad Street pump on purely observational evidence. There are at least 40 studies showing increased cardiovascular events with higher sodium intake and reduced events with lower sodium intake (Aburto et al., 2013b; He et al., 2013).
- With severe sodium restriction, down to a level as low as 30 mmol/day, plasma levels of renin, aldosterone, and lipids increase (Graudal et al., 2012). Such rigid reductions are simply impossible for free-living people to maintain, even those on dialysis who are acutely aware of the dangers of sodium intake. Moreover, maintaining a dietary intake of sodium below 66 mmol/day precludes a nutritionally adequate diet in the U.S. (Maillot & Drewnowski, 2012).
- In patients with end-stage renal disease (Thomas et al., 2011) or type 2 diabetes (Ekinci et al., 2011), an increase in mortality was seen with lower sodium intake, but the contribution of the lower intake contributed to only 7% of the difference.
- In the ONTARGET trial, the rate of cardiovascular disease showed a U curve, with increases above 8 g/day or below 3 g/day (O’Donnell et al., 2011). However, the estimate of 24-hour levels was based on a single voided specimen, which is known to be inaccurate (Whelton, 2011).
- In a meta-analysis of seven RCTs on sodium reduction, more cardiovascular events were reported in those on a lower sodium intake (Taylor et al., 2011). In fact, all of the increase came from one trial of patients with severe heart failure who were taking massive doses of diuretic (He & MacGregor, 2011). The other six studies showed a 20% lower risk of cardiovascular disease in those on a lower sodium intake.
- In a largely normotensive population followed for 7.9 years, those with initially lower sodium excretion had higher cardiovascular mortality (Stolarz-Skrzypek et al., 2011). However, the small number of deaths in the high-sodium tertile (10) was too small for statistical analysis, and only one urine collection at the start of the trial was used to estimate the 7.9-year level of intake.
These five observational studies all have serious faults, which make their conclusions suspect. Nonetheless, even if they were valid, these five (all that were found in a search of the literature from 2000 to 2013) do not come close to countering the data from over 40 studies that have shown a decrease in cardiovascular events with lower sodium intake.
Conclusions
High sodium intake is harmful, and moderate sodium reduction is worthwhile and feasible. The reduction of BP possible with a universal reduction in sodium intake of 50 mmol/day down to the recommended level of 100 mmol/day has been estimated to translate into a decrease of 0.7 to 1.2 million deaths over a 10-year interval (Coxson et al., 2013). Such estimates may be valid: Repeated surveys from 1966 to 1986 in Belgium showed a progressive decrease in average sodium intake from 203 to 144 mmol/day; these falls correlated closely with lesser rises in BP with increasing age and decreased stroke mortality in the population (Joossens & Kesteloot, 1991). In a 10-year follow-up of 2,657 subjects, a 17% increase in strokes was found with each 500 mg/d increase in sodium intake (Gardener et al., 2012). Therefore, population-wide reductions in sodium intake are likely to both improve health and reduce costs to society. The documented potential for benefit, with the remote possibility of harm, makes moderate sodium reduction a desirable goal both for the individual hypertensive patient and for the population at large (Whelton, 2014).
POTASSIUM SUPPLEMENTATION
Some of the benefits of reduced sodium intake could reflect an increased potassium intake (Aburto et al., 2013a; Yang et al., 2011), although in the TONE study, the antihypertensive effects of the two were independent of each other (Appel et al., 2001).
Clinical Data
Aburto et al. (2013a) identified 22 RCTs and 11 cohort studies on the effects of potassium supplementation on BP, 16 in hypertensive patients. A pooled analysis of the 33 trials showed an overall reduction in BP of 3.5/2.0 mm Hg with greater effects in the 16 trials of hypertensives (5.3/3.1 mm Hg) or when the intake of potassium was as high as 90 to 120 mmol/day (7.2/4.0). In addition, the response was greater when the sodium intake was above 176 mmol/day. No significant adverse effects on blood lipids, catecholamines, or renal function were noted.
Protection Against Strokes
In the analysis of nine cohort studies, Aburto et al. (2013b) found that increased potassium intake was associated with a 24% reduction in the incidence of strokes (Fig. 6-4). In another meta-analysis of data from 15 cohort studies covering over 240,000 subjects, a 42 mmol/day increase in potassium intake was associated with a 21% lower risk of stroke (D’Elia et al., 2011).
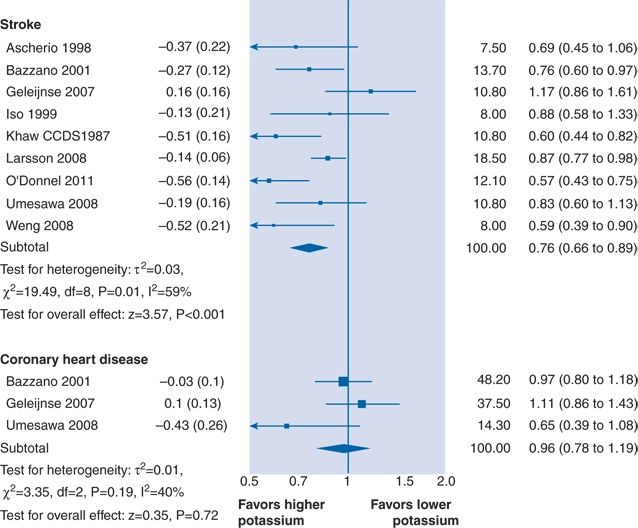
FIGURE 6-4 Association between higher potassium intake and risk of incident cardiovascular disease, stroke, and coronary heart disease in adults. (Modified from Aburto NJ, Hanson S, Gutierrez H, et al. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ 2013a;346:f1378).
Recommendations
Though potassium supplements may lower the BP, they are too costly and potentially hazardous for routine use in the treatment of hypertension in normokalemic patients. They are indicated for diuretic-induced hypokalemia and, in the form of potassium-containing salt substitutes, will add little expense. For the larger population, a reduction of high-sodium/low-potassium processed foods with an increase of low-sodium/high-potassium natural foods is likely all that is needed to achieve the potential benefits (Kelly et al., 2012). Fruits and beans provide the largest quantity of potassium per serving.
CALCIUM SUPPLEMENTATION
More milk or, in blacks, supplements of vitamin D may lower blood pressure, but calcium supplements or even high levels of dietary calcium intake will increase the risk of CVD mortality in men (Xiao et al., 2013) and women (Michaelsson et al., 2013). Although the effects of increased calcium on BP were not reported in these two reports, increases in calcium excretion were associated with higher BP in two large cross-sectional studies (Kesteloot et al., 2011). Furthermore, increased calcium intake was directly associated with the risk of stroke in 34,670 women over a 10.4-year follow-up (Larsson et al., 2011).
Recommendations
In the presence of such data showing a significant adverse effect on cardiovascular disease, calcium supplements are not recommended for treatment of hypertension, an example of the critical need for evidence to base recommendations despite repeated claims of a beneficial effect (McCarron & Morris, 1985). The best course is to ensure an adequate dietary calcium intake but not to give calcium supplements to either prevent or treat hypertension.
MAGNESIUM SUPPLEMENTATION
Whereas serum and intracellular magnesium levels are normal in most untreated hypertensives, low muscle magnesium concentration has been found in half of patients on chronic high-dose diuretic therapy (Drup et al., 1993) and low serum levels in patients on long-term proton pump inhibitors (Furlanetto & Faulhaber, 2011). Moreover, in a 7.6-year follow-up of 5,511 people, low urinary magnesium levels were associated with an increased risk of hypertension (Joosten et al., 2013).
However, in a review of 12 high-quality trials of magnesium supplements covering 545 hypertensives, Dickinson et al. (2006) found that SBP fell by an insignificant −1.3 mm Hg, whereas DBP fell by a significant −2.2 mm Hg. The conclusion was: “In view of the poor quality of included trials and the heterogeneity between trials, the evidence in favor of a causal association between magnesium supplementation and BP reduction is weak and is probably due to bias….”
Therefore, rather than giving magnesium supplements, increasing dietary consumption with fresh fruits and vegetables that provide magnesium seems preferable (Larsson et al., 2008).
INCREASED PHYSICAL ACTIVITY
The evidence for protection from both the development of hypertension and CVD and all-cause mortality by regular physical activity is incontrovertible. Nonetheless, most people in all industrialized societies are becoming less physically active in their daily lives, spending more and more time in sedentary activities (Kohl et al., 2012). Not only will increased physical activity and higher levels of exercise capacity reduce mortality (Wen et al., 2011) but they will also likely prevent the development of hypertension (Shook et al., 2012). In a prospective 4.7-year follow-up of 6,000 people, the incidence of hypertension was reduced by 42% in those who engaged in high levels of physical activity even if they had a parental history of hypertension (Shook et al., 2012). A mortality benefit extends to those with hypertension (Rossi et al., 2012) or even hypertension resistant to medical therapy (Dimeo et al., 2012). In a cohort study covering 400,000 people, as little as 15 minutes of exercise a day was associated with reduced mortality (Wen et al., 2011).
Clinical Data
BP is lowered by exercise whether aerobic (Cornelissen et al., 2013) or resistance (Figueroa et al., 2013), even without weight loss (Lee et al., 2011). The benefit extends even to children as young as 5 years (Knowles et al., 2013) and the elderly with prevention of cognitive impairment (Verdelho et al., 2012). Moreover, patients with orthostatic hypotension may have less of a postural fall after performing regular exercise (Moraes et al., 2012).
Because the SBP rises during exercise and because the abrupt rise in BP after arising from sleep may be associated with an increased incidence of cardiovascular events, concerns about exercise in the morning have been raised. However, even in patients with known coronary disease, no increase in events was noted with exercise performed in the morning versus the afternoon (Murray et al., 1993). On the other hand, strenuous physical exertion in patients who are habitually sedentary may, on occasion, precipitate an acute myocardial infarction (Dahabreh & Paulus, 2011). Therefore, sedentary patients should be advised to increase their level of activity slowly.
Hypertensives may experience difficulty if they take β-blockers, which blunt exercise-mediated increases in heart rate and cardiac output (Vanhees et al., 2000). Other antihypertensive agents should not interfere with exercise ability.
There may be concerns about another activity that involves exercise—sexual intercourse, which is accompanied by significant rises in pulse and BP that are equivalent to stage II of the standardized Bruce treadmill test for men and stage I for women (Palmieri et al., 2007). Although actually quite rare even among patients with coronary disease, the triggering of myocardial infarction during sexual activity likely can be prevented by regular exercise (Dahabreh & Paulus, 2011). Moreover, erectile dysfunction in obese men may be overcome by a program of physical activity and weight loss (Gupta et al., 2011).
Recommendations
Increased levels of physical activity, either during ordinary life or with structured exercise, may lower BP and prevent the onset of hypertension (Faselis et al., 2012). As little as 15 minutes of walking or its equivalent per day provides a reduction in mortality (Wen et al., 2011), and as little as 30 minutes a day three times a week slows the decline in cognitive function in the elderly (Verdelho et al., 2012). Despite the proven benefits, few physicians counsel their patients about exercise, even though counseling has been shown to be effective in increasing patients’ level of physical activity (Hallal & Lee, 2013). Other than for cessation of smoking, this advice can have the most immediate acceptance and greatest overall benefit.
MODERATION OF ALCOHOL
Alcohol is a two-sided issue: Up to one portion a day for women and two for men are protective against heart attacks and stroke (Ronksley et al., 2011), but consumption of more than one usual portions per day may raise BP (Briasoulis et al., 2012). (A usual portion of alcohol-containing beverage is 12 oz of beer, 4 oz of wine, or 1.5 oz of whiskey, each containing 10 to 12 mL of alcohol.)
Effects on Blood Pressure
Acutely, the drinking of 60 g of ethanol, the amount contained in five usual portions, induces an immediate fall in BP averaging 4/4 mm Hg followed, after 6 hours, by a rise averaging 7/4 mm Hg (Rosito et al., 1999). Three or more portions per day is associated with a significant increased risk of hypertension (Briasoulis et al., 2012), and binge drinking is associated with increased blood pressure and cardiovascular mortality (Sull et al., 2010). When heavy drinkers abstain, their BP usually goes down (Xin et al., 2001). An analysis of the relation between the risk of hypertension and the pattern of drinking found a slightly lower incidence among those who drank daily with meals but a 41% increased incidence in those who drank without food (Stranges et al., 2004).
Studies on the effects of alcohol may be confounded by a number of factors including a healthier lifestyle in those who drink in moderation and the inclusion of former heavy drinkers into current nondrinkers.
Beneficial Effects
Nonetheless, there is impressive evidence for a protective effect of moderate, regular alcohol consumption of one-half to two portions per day on a host of cardiovascular and other diseases when compared to similar outcomes in nondrinkers or heavy drinkers. In an analysis of data from 84 high-quality studies, Ronksley et al. (2011) found a 25% lower risk for cardiovascular mortality and a 29% reduction in the incidence of coronary disease but no effect on stroke. In addition, moderate drinking has been associated with less heart failure (Djoussé & Gaziano, 2007), the incidence of type 2 diabetes (Wei et al., 2000), osteoporosis (Berg et al., 2008), and cognitive impairment (Stampfer et al., 2005). Beneficial effects have been attributed to improvements in the lipid profile, in hemostatic factors, insulin sensitivity (Avogaro et al., 2002), and antioxidant activity (Vasdev et al., 2006).
However, no mortality benefit is seen in young people, and a 15% increased incidence of breast cancer has been reported in women who drink more than one portion per day (Chen et al., 2011) and of colon cancer in those who drink more than two portions per day (Cho et al., 2004). Beyond the apparently proved association between even small amounts of alcohol and breast cancer, claims have been made for an association with multiple others cancers (Nelson et al., 2013). However, when the data are examined, all of these associations (save for the extremely rare cancer of the larynx) are shown to be lower in those who drink >20 to 40 g/day (equivalent to 2 to 3 usual portions) compared to those who drink 0 to 20 g/day (equivalent to none to 1 and a half usual portion). No explanation is offered for this inverse relationship, but it adds to the evidence for the safety of moderate drinking. As of now, the associations of moderate regular alcohol consumption with multiple benefits support current guidelines, which allow for moderate drinking.
Wine may be more protective than beer or whiskey (Renaud et al., 2004), but wine drinkers tend to have a healthier lifestyle, so this apparent benefit may be exaggerated. Although there is some evidence that red wine is more protective than white wine because of its increased levels of polyphenols (Botden et al., 2011), the same investigators later reported no lowering of blood pressure with red wine (Botden et al., 2012). To add to the confusion, red wine with the alcohol removed lowered blood pressure and increased plasma NO (Chiva-Blanch et al., 2012).
Recommendations
The following guidelines seem appropriate:
- Carefully assess alcohol intake, as some people drink well beyond moderate amounts without being aware of their excessive consumption or its deleterious effects.
- If intake is more than one portion per day in women or two per day in men, advise a reduction to that level.
- Strongly advise against binge drinking.
- Drink along with food.
- For most people who consume moderate amounts of alcohol, no change is needed. If middle-aged (45- to 64-year-old) people start to drink, they rarely go beyond recommended amounts while properly benefiting from lower rates of cardiovascular morbidity (King et al., 2008).
OTHER DIETARY FACTORS
The impressive results of the DASH diet shown in Figure 6-2 strongly support an antihypertensive effect of a diet low in saturated fat and high in fiber and minerals from fresh fruits and vegetables (Sacks et al., 2001). Moreover, among 1,710 middle-aged men followed up for 7 years, the rise in SBP was significantly less with diets higher in fruits and vegetables and lower in red meats (Miura et al., 2004). Vegetarians likely have less hypertension than non-vegetarians. Compared to those eating a non-vegetarian diet, those consuming a vegetarian diet under controlled conditions had a lower BP in 7 clinical trials and 32 observational studies (Yokoyama et al., 2014).
Responses of BP to dietary ingredients may be genetically determined: Only the 10% of hypertensives with a specific genotype had a lowering of BP with supplemental riboflavin (Wilson et al., 2013).
Dietary Nitrate
Certain green leafy vegetables, such as spinach, lettuce, and beetroot have high inorganic nitrate (NO3) content. In an intriguing rediscovery of the antihypertensive effect of nitrate via its endogenous bioconversion to nitrite (NO2), partially on the tongue, Webb et al. (2008) and Kapil et al. (2010) found a significant acute BP lowering, vasoprotective and antiplatelet effect of dietary nitrate contained in beetroot juice. After bioconversion from nitrate, the nitrite is reduced to NO when ischemia or injury induces a more acidic environment within tissues. The NO generated from nitrite induces vasodilation, thereby lowering BP.
Fiber
One feature of a vegetarian diet is the increased amount of fiber. A meta-analysis of 24 randomized, placebo-controlled clinical trials published from 1966 to 2003 on the effect on BP of supplements of dietary fiber averaging 11.5 g/day found an average fall of 1.1/1.3 mm Hg (Streppel et al., 2005). Greater intake of fiber is associated with a significantly lower incidence of initial stroke (Threapleton et al., 2013) and reduce mortality after a MI (Li et al., 2014).
Dietary Fat
In keeping with the potential contribution of the low saturated fat content of the DASH diet, increased consumption of low-fat dairy food was reported to reduce the incidence of hypertension (Soedamah-Muthu et al., 2012). The type of fat may be important. As a component of the cardiovascularly beneficial Mediterranean diet, olive oil may lower BP because of its high content of monounsaturated fatty acids or antioxidant polyphenols (Moreno-Luna et al., 2012), and increased consumption of monounsaturated fatty acids was associated with lower diastolic BP (Miura et al., 2013). Increased intake of linoleic acid, the main dietary polyunsaturated fatty acid, was associated with a significant fall in BP (Miura et al., 2008). Omega-3 fatty acid in flaxseed has been shown to lower BP significantly (Rodriguez-Levya et al., 2013), but overall, antioxidant supplements have been found to have no effect on cardiovascular events (Myung et al., 2013).
On the other hand, flavonoid-rich dark chocolate may be beneficial: Consumption of 100 g/day provided an improvement in endothelial function (Grassi et al., 2012), and in seven high-quality studies, higher intake of chocolate was associated with a 37% reduction in cardiovascular events and a 29% reduction in strokes (Buitrago-Lopez et al., 2011). Cocoa flavanol was reported to lower BP and improve cognitive function in elderly subjects (Desideri et al., 2012).
Lipid-Lowering Diet and Drugs
Lipid-lowering drugs, in particular statins, improve the endothelial dysfunction associated with dyslipidemia, thereby lowering BP (Kanaki et al., 2012). Protection against atherosclerotic complications, including stroke, has been seen with statins in both normotensives and hypertensives (Taylor et al., 2013).
Uric Acid Reduction
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








