CHAPTER 283 Treatment of Thoracic Disk Herniation
The incidence of thoracic disk herniation ranges from 7% to 37%.1,2 However, only 0.25% to 0.57% of all disk herniations are symptomatic.3 Thoracic disk herniation may present with neurological manifestations that include pain; sensory loss; bowel, bladder, or sexual dysfunction; paraparesis; and paraplegia. In this chapter we review the evolution of surgical techniques that can be used to perform thoracic diskectomies.
History and Epidemiology
Middleton and Teacher4 performed the first thoracic diskectomy in 1911 on a paraplegic man who subsequently died. In those days, diagnosis was based on the identification of calcification in the disk space and clinical acumen. The limited diagnostic resources made it difficult to diagnose early disease and localize it accurately. Many patients presented with frank myelopathy and severe neurological deficits.5
The advent of computed tomography (CT) and later magnetic resonance imaging (MRI) dramatically improved the ability to diagnose and localize the level of the herniated thoracic disk.6 With the further development of MRI techniques, clinicians can now accurately diagnose and pinpoint the level of disk herniation in the thoracic spine. CT-myelography provides additional information in certain cases, especially when the disk is calcified or when reoperation is being performed at the same level to determine the extent of prior bone resection. Currently, MRI is considered the first-line modality to diagnose thoracic disk herniation. It is noninvasive and provides a precise image of the herniated disk and its relationship to the dural sac and the nerve; it provides additional information about the conformation of the cord and whether an intramedullary signal change, and hence cord injury, is present.
Most thoracic disk herniations occur in patients between the fourth and sixth decades of life, with a slight male predominance.7 A history of trauma is reported in 22% to 50% of symptomatic patients.8 It is usually associated with a fall landing on the feet or buttocks, combined with an axial spinal rotation. Thoracic disk herniations are much less common than herniations of the lumbar and cervical spine. This is because of the limited mobility of the thoracic spine, the smaller disks, and the stabilizing effect of the rib cage.9,10
Early surgical attempts to treat thoracic disks involved a posterior laminectomy, dural sac retraction, and completion of the diskectomy. These operations were associated with a high rate of neurological deterioration and death. Published series quoted neurological deterioration in 18% to 66% of patients and mortality rates of 14% to 50%.9,11–15
Clinical Presentation and Differential Diagnosis
Pain is the most common symptom associated with thoracic disks. The pain is dorsal and midline in 57% to 88% of patients but may be dermatomal in 9% to 57%. When dermatomal, the pain is lancinating and often unilateral, but it may be bilateral in some cases. The next most common complaint is sensory changes in a radicular pattern, occurring in 39% to 100% of patients. Dermatomal sensory loss is quite rare because of the overlap in sensation from adjacent-level nerve roots. In addition, patients may present with findings associated with spinal cord compression, including myelopathy (9% to 100% of patients), weakness (41% to 100%), and bowel and bladder dysfunction (18% to 78%).8,16–20
Unusual presentations have been reported as well. A herniated disk at the level of C7-T1 or T1-2 has been reported to cause Horner’s syndrome.21–24 Another unusual presentation is dysesthesia in the medial arm, which may erroneously be associated with myocardial infarction, angina, thoracic aortic dissection, or bronchogenic tumor.25 Also, far lateral thoracic disk herniation may present as flank pain.26
Patients may present with spinal cord syndromes associated with thoracic disk herniation. The specific presentation is dependent on the pattern of neural compression on the cord. Brown-Séquard syndrome may occur when the herniated disk is lateral and compressing one side of the spinal cord, whereas anterior spinal artery syndrome occurs when the herniated disk is central and compressing the anterior spinal artery; conus medullaris syndrome is caused by a herniated disk compressing the conus medullaris at the thoracolumbar junction.13,16,19 Other differential diagnoses include primary and metastatic neoplasm, demyelinating disease, primary motoneuron disease, neuromuscular disease, myopathy, muscular dystrophy, motor neuropathy, spinal cord infarction, and spinal cord vascular malformation. Other entities that need to be considered are those related to visceral referred pain, such as renal colic, gallbladder colic, colitis, intercostal neuritis, and costochondritis.25
Radiologic Evaluation
Magnetic Resonance Imaging
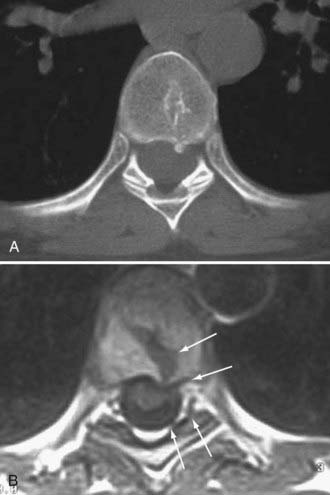
The primary care physician often performs MRI of the thoracic spine in the evaluation of back pain. It is the best screening method for thoracic disk herniation, given its noninvasive nature and high sensitivity. However, it is also associated with 14.5% false-positive rate, making it crucial to correlate the MRI information with the clinical examination.27,28 The exaggeration of disk herniation (which is not unique to the thoracic spine), especially in sagittal images, has been attributed to the edge effect, which occurs when two substances of different proton densities are next to each other. The edge effect is most pronounced on T2-weighted images between the disk substance and the adjacent cerebrospinal fluid. Axial images provide further information about the level of stenosis caused by the herniated thoracic disk. Increased signal on T2-weighted images may be seen in the spinal cord when it is significantly compressed. In addition, MRI can distinguish herniated disks in the thoracic spine from neoplastic, demyelinating, or infectious pathologies. It can also distinguish intradural versus extradural lesions. When the accuracy of MRI is in doubt, it is best to obtain a thoracic myelogram and postmyelogram CT to further delineate the extent of dural sac compression, presence of calcification in the herniated disk, and presence of posterior osteophytes and their relation to the dural sac.29,30 Thoracic myelograms and postmyelogram CT scans are most useful for extradural lesions.
Myelography and Postmyelography Computed Tomography
Some clinicians still consider the combination of myelography and postmyelography CT the “gold standard” in patients with calcified herniated disks. It typically shows an indentation caused by an extradural mass compressing the dural sac at the level of the disk. Postmyelography CT allows the distinction among bone, calcified soft tissue, soft tissue, dural sac, and spinal cord. It also allows the visualization of posterior osteophytes and disk material and their relationship to the dural sac. Twelve percent of thoracic disk herniations are associated with calcifications in the spinal canal, which suggests an intradural extension of the herniated disk.22,29,31,32 CT-myelography, like MRI, has a high false-positive rate (13.5%) in diagnosing symptomatic thoracic disk herniation.33
Management
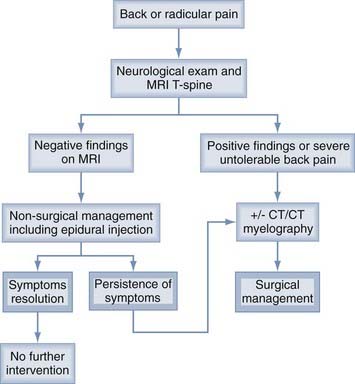
Management of symptomatic disk herniation is illustrated in Figure 283-1. Nonsurgical management should be instituted first, unless there is an associated neurological deficit or intolerable pain. Surgical intervention is indicated when there is radiographic evidence of spinal cord compression and clinical examination findings of myelopathy, weakness, or bowel, bladder, or sexual dysfunction, or when the patient is experiencing severe back or radicular pain. Patients with mild to moderate pain that is refractory to conservative management may be good surgical candidates as well. The aim of conservative therapy is to allow the herniated disk to resorb34 and the inflamed nerve root to heal.18,28,29,35
Nonsurgical Management
Nonsurgical management includes restricted activity, immobilization with a hyperextension brace, oral steroids, nonsteroidal anti-inflammatory drugs, oral pain medications, and epidural injections.18,28,29,35 Figure 283-1 summarizes the nonsurgical management protocol.
Surgical Management
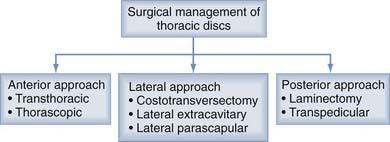
Three surgical approaches can be used: posterior, posterolateral, and anterior (Fig. 283-2). The posterior approach includes dorsal laminectomy and a transpedicular approach. The posterolateral approach includes costotransversectomy and lateral extracavitary and lateral parascapular approaches. The anterior approach includes transthoracic and thoracoscopic approaches. Table 283-1 summarizes the pros and cons of each approach.
TABLE 283-1 Pros and Cons of Surgical Approaches for Thoracic Diskectomy
| APPROACH | PROS | CONS |
|---|---|---|
| Laminectomy | Simple to perform | High morbidity and mortality Limited exposure Need to retract dural sac |
| Transpedicular | Simple to perform Minimally invasive Good for lateral disks; may be used for paracentral disks with poor visualization | Difficult to visualize ventral dural sac Difficult to dissect midline calcified disks Limited exposure for multilevel OPLL |
| Costotransversectomy | Extrapleural Good for lateral disks; may be used for paracentral disks with better visualization than transpedicular approach | Difficult to visualize ventral dural sac Difficult to dissect midline calcified disks Limited exposure for multilevel OPLL |
| Lateral extracavitary | Extrapleural Best visualization of midline structures among posterior and posterolateral approaches Access to multiple levels Adequate exposure to resect multilevel OPLL Allows fusion if needed | Limited visualization of ventral dural sac Painful Potentially higher risk for radicular artery injury leading to spinal cord infarction45 |
| Transthoracic (open) | Best visualization of large midline calcified or soft herniated disks Access to multiple levels Adequate exposure to resect multilevel OPLL Access for fusion if needed | Painful Potential morbidity Need for chest tube |
| Thoracoscopic | Best visualization of large midline calcified or soft herniated disks Access to multiple levels (up to three) Minimally invasive | Limited exposure for multilevel OPLL Need for chest tube Steep learning curve |
OPLL, ossification of the posterior longitudinal ligament.
Identification of Surgical Level
Identification of the correct surgical level may be challenging. Preoperative lumbar and thoracic films are helpful in determining the number of lumbar vertebrae and identifying the last thoracic rib in relation to the herniated disk level. Intraoperative identification of the surgical level is performed with high-quality fluoroscopy, anteroposterior and lateral films, or imaging guidance when available.36,37
Posterior Approach
Posterior thoracic laminectomy was the first approach described for thoracic diskectomies. However, it provides inadequate exposure of midline herniated disks, and significant retraction of the dural sac is almost always needed. It is estimated that 70% to 90% of thoracic disk herniations that cause spinal cord or nerve compression are central or paracentral.22,29,31,32 This explains the necessity of dural sac retraction to reach the herniated disk. There are reports that thoracic laminectomy performed for thoracic diskectomy is associated with unacceptably high rates of morbidity and mortality. It is estimated that there is at least a 45% chance of experiencing neurological deterioration or no benefit with this approach.14,38,39 Currently, this approach is completely contraindicated in the management midline calcified herniated thoracic disks,40 and surgeons should consider the other approaches discussed.
![]() Alternatively, the transpedicular approach allows better exposure of the paracentral herniated disk, with minimal dural sac retraction and sparing of the facet (Fig. 283-3). The foramen of the affected level is unroofed by drilling the medial half of the inferior facet of the above vertebra and the medial half of the superior facet along with the superior part of the pedicle of the lower vertebra. A trough is created with a high-speed diamond drill in the posterior inferior vertebrae overlying the relevant disk space; in the posterior superior vertebrae below the disk space, including the end plates; and in the lateral aspect of the disk space laterally. The resultant trough should be large enough to pull the disk material into the trough without significant manipulation of the dura. (See Video 283-1.)
Alternatively, the transpedicular approach allows better exposure of the paracentral herniated disk, with minimal dural sac retraction and sparing of the facet (Fig. 283-3). The foramen of the affected level is unroofed by drilling the medial half of the inferior facet of the above vertebra and the medial half of the superior facet along with the superior part of the pedicle of the lower vertebra. A trough is created with a high-speed diamond drill in the posterior inferior vertebrae overlying the relevant disk space; in the posterior superior vertebrae below the disk space, including the end plates; and in the lateral aspect of the disk space laterally. The resultant trough should be large enough to pull the disk material into the trough without significant manipulation of the dura. (See Video 283-1.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree