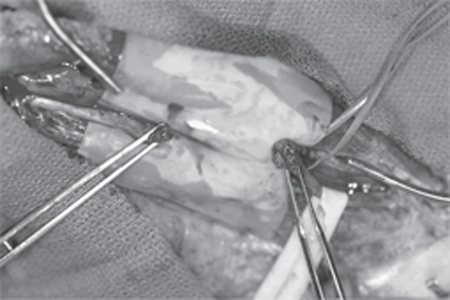
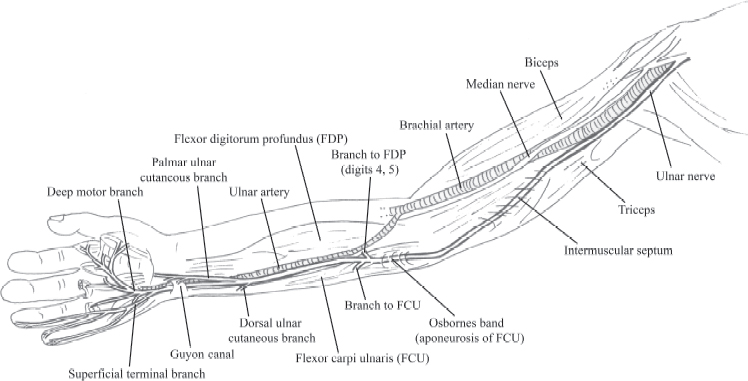
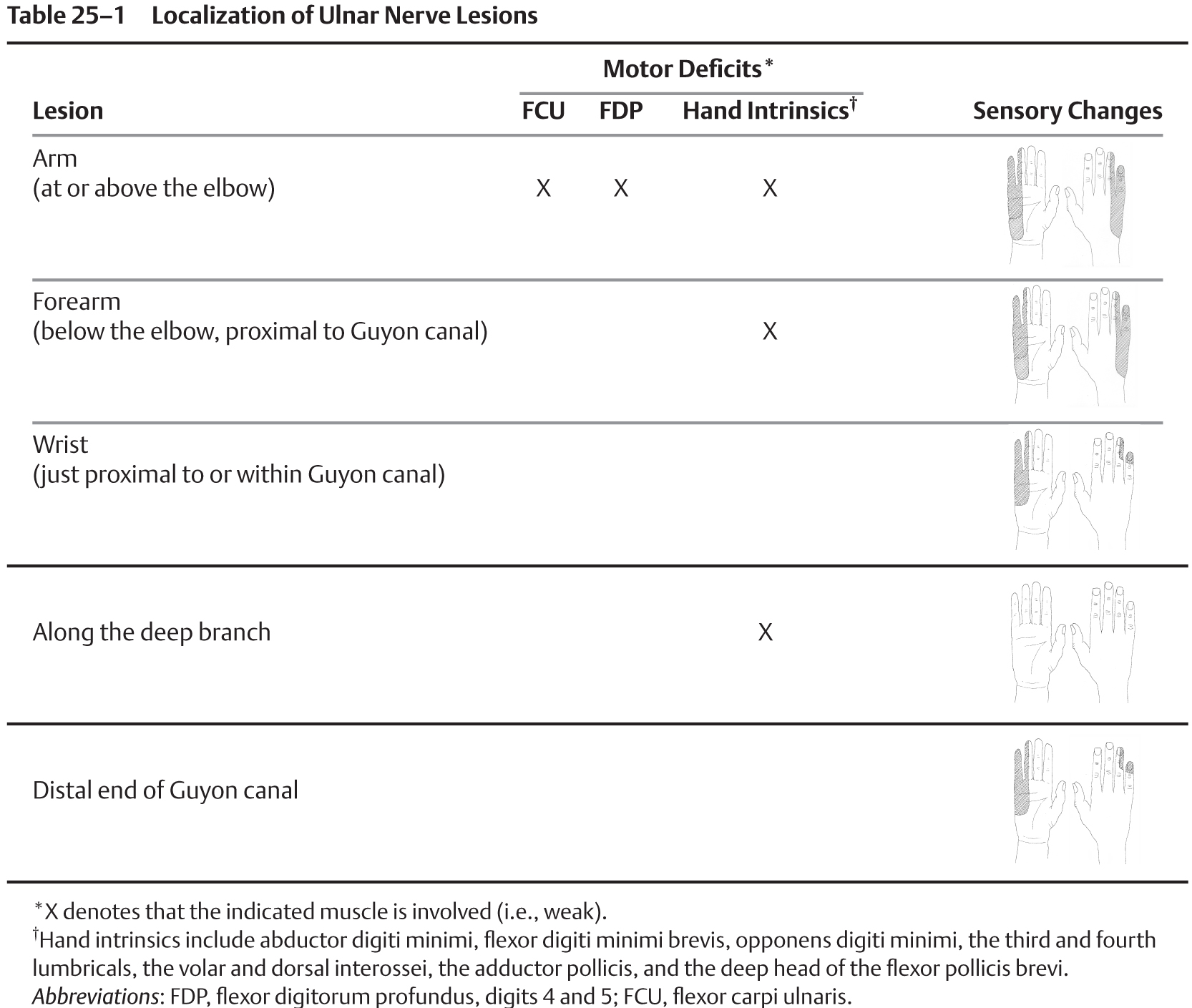
25 Ulnar Nerve Injury A 39-year-old previously healthy butcher was cutting ham on an automatic slicer. He was suddenly distracted and suffered a deep laceration of his arm. He went directly to the hospital. On examination, he had a deep laceration at the medial distal third of his right arm. There was no massive bleeding from the wound and the distal pulses were present. The grip and pinch strength was diminished. All ulnar-innervated muscles, namely, the first dorsal interosseous, abductor digiti minimi, flexor digiti minimi, opponens digiti minimi, flexor digitorum profundus (FDP) of the small and ring fingers, third and fourth lumbricals, adductor pollicis, and flexor carpi ulnaris (FCU), were 0/5. The radial and median innervated muscles were unaffected. The patient had complete loss of sensation of the ulnar palmar and dorsal surface of his hand and fingers (ulnar portion of the fourth and fifth fingers). Tetanus vaccine booster was given. X-rays did not show associated bony fracture. In view of the acute open ulnar nerve injury, the patient was taken immediately to the operating room for exploration and repair. After thorough irrigation of the wound, situated just above the elbow, exploration revealed a lacerated ulnar nerve. However, due to the saw, a small portion of the proximal and distal ends of the nerve had to be excised to have edges with normal fascicular structure for reconstruction. After excision of the damaged nerve edges, direct repair could not be done without tension (Fig. 25–1). The incision was extended to expose the ulnar nerve at the elbow and proximal forearm. The ulnar nerve was mobilized and transposed anteriorly in a subcutaneous location to gain additional length. Direct end-to-end epineurial suture repair was then possible without tension. Postoperatively, no activity restrictions were imposed and the patient was instructed to maintain full range of motion. The patient had no complications related to his surgery. After 4 weeks, he started intensive physiotherapy. He will be followed in 6 months with electromyographic studies. Acute laceration of the ulnar nerve Figure 25–1 Intraoperative picture of lacerated ulnar nerve. The ulnar nerve (Fig. 25–2) is an extension of the medial cord of the brachial plexus and contains fibers from C8, T1, and, infrequently C7, nerve roots. This mixed nerve sup plies muscles of the forearm and hand and provides sensation over the fourth and fifth digits of the hand, palm (ulnar side), and dorsal (ulnar side) portion of the hand. Initially, the ulnar nerve lies medial to the axillary artery. It continues medial to the brachial artery, between the triceps and biceps muscles, to the middle of the arm. It then pierces the intermuscular septum and courses anteriorly along the medial head of the triceps muscle. At the elbow, it enters the postcondylar groove, situated between the medial epicondyle and olecranon. Distal to the postcondylar groove, the ulnar nerve courses deep to the aponeurosis between the two heads of the FCU muscle (Osborne band) and continues into the forearm between this muscle and the FDP. Near the wrist, the ulnar nerve runs medial to the ulnar artery, both being lateral to the FCU tendon. They both continue into the hand via the Guyon canal. This canal consists of the volar carpal ligament (roof), the flexor retinaculum (floor), the hamate (laterally), and the pisiform (medially). Figure 25–2 Anterior aspect of the right arm showing the course and important branches of the ulnar nerve. The ulnar nerve does not branch in the arm. The first branches occur just distal to the elbow and supply the FCU and ulnar portion of the FDP digits 4 and 5. The palmar and dorsal ulnar cutaneous branches are the other forearm branches of the ulnar nerve, taking off proximal to the Guyon canal. The origins of the ulnar sensory branches are the most valuable in localizing an ulnar nerve lesion. Sensory loss that includes the palmar or dorsal aspect of the hand implies a lesion proximal to the Guyon canal. Distal to the Guyon canal, the ulnar nerve divides into the superficial and deep branches. The superficial (sensory) branch supplies the skin of the hypothenar eminence and the digital nerves to the small and ulnar side of the ring finger. The deep (motor) branch supplies all ulnar-innervated muscles in the hand. With the deep branch of the ulnar artery, it passes between the abductor digiti minimi and the flexor digiti minimi brevis. It perforates the opponens digiti minimi and follows the deep volar arch across the interossei. It supplies the three muscles of the small finger, the third and fourth lumbricals, the volar and dorsal interossei, the adductor pollicis, and the deep head of the flexor pollicis brevis. Anatomical variants may confuse the diagnosis. Martin-Gruber anastomoses, present in 10 to 44% of individuals, consist of branches of the median nerve to the ulnar nerve in the forearm. Connections between the deep ulnar and median nerves in the hand are called Riche-Cannieu anastomoses. In these variants, unexpected functioning intrinsic muscles can be observed with ulnar nerve injury. Nerve injury may be secondary to blunt trauma (crush and stretch injuries), penetrating injury (stab wound, lacerations, gunshot, etc.), iatrogenic injury (orthopedic procedure, compression, etc.), or medical conditions (diabetes, inflammation, etc.). For the ulnar nerve, traction injuries occur from violent valgus injuries to the elbow as in avulsion fracture of the medial epicondyle and lateral dislocation of the elbow. The most common injury resulting from these dislocations or fracture-dislocations seems to be ulnar nerve neurapraxia, which spontaneously resolves after a closed reduction. Supracondylar fracture of the humerus can directly damage the ulnar nerve. Increasing valgus deformity due to nonunion of a fracture of the humerus lateral condyle may cause tardy (late) ulnar neuritis and palsy. Fracture fragments or arthritic spurs in or around the groove impinging on the nerve and recurrent dislocation of the ulnar nerve also cause ulnar neuritis. At the wrist, fracture of the hook of the hamate and lacerations are common causes of ulnar nerve traumatic injury. The exam for ulnar nerve injury includes testing the strength of individual muscles, the grip and pinch strength, and sensation. The exam can define the level of injury (Table 25–1). A lesion above the elbow will involve all ulnar-innervated muscles and sensation of the palm, dorsum of the hand, and fourth and fifth fingers. A lesion in the forearm will spare the FCU and FDP, whose branches originate just distal to the elbow. A lesion at the wrist will also spare the sensation of the palm and dorsum of the hand. The hand intrinsic muscles may be intact in some patients with Martin-Gruber or Riche-Cannieu anastomoses. In long-standing lesions, muscle bulk is decreased, especially seen in the hypothenar and first dorsal inter-osseous area. Known deformities may be present, such as Wartenberg sign (abducted little finger), clawing of the ring and small finger, and Froment paper sign (distal thumb flexion when holding a piece of paper between the index finger and thumb) (i.e., substitution of the median nerve–innervated flexor pollicis longus for the denervated adductor pollicis). In ulnar nerve entrapment at the elbow, from a remote trauma, paresthesias of the fourth and fifth fingers, variable weakness, and pain are present. The pain, which may be extensive and include the elbow, arm, and shoulder, is less localizing than the paresthesias. A discrepancy between the magnitude of trauma and the degree of ulnar nerve dysfunction should prompt investigations for concurrent pathology. Diabetic ulnar mono-neuropathy is infrequent but may occur and may present acutely. Ulnar neuropathy mimics may present after a trivial trauma that may not be related. A complete neurological exam should be performed to exclude causes such as amyotrophic lateral sclerosis, cervical radiculopathy, brachial plexopathy, and polyneuropathy.
 Case Presentation
Case Presentation
 Diagnosis
Diagnosis
 Anatomy
Anatomy
 Etiologies
Etiologies
 Characteristic Clinical Presentation
Characteristic Clinical Presentation
 Differential Diagnosis
Differential Diagnosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


