63 Vertebral Body Augmentation
I. Key Points
– Vertebral augmentation is commonly employed in treating compression fractures in patients with osteoporosis or spine tumors.
– Two different percutaneous vertebral augmentation methods for cement application into the vertebral body have been documented: vertebroplasty and kyphoplasty.
– In vertebroplasty, polymethylmethacrylate (PMMA) cement is injected percutaneously into the collapsed vertebral body.
– Kyphoplasty involves placing inflatable bone tamps percutaneously into a vertebral body. The inflation of the bone tamp allows some restoration of vertebral height. After deflation, the cavity that has been produced is filled by injection of PMMA.
– Two randomized clinical trials showed that improvement in patients with painful osteoporotic vertebral fractures was similar between those treated with vertebroplasty and those treated with a simulated procedure, at one month follow-up.1,2
– Compared with nonsurgical management, balloon kyphoplasty resulted in improvements in quality of life and disability measures and reduction of back pain in patients with acute painful vertebral fractures.2
II. Indications
– Severe pain or progressive collapse due to vertebral body compression fractures in patients with osteoporosis (primary or secondary).
– Severe pain or progressive collapse due to vertebral body metastasis or multiple myeloma. Treatment algorithm for painful thoracic or lumbar vertebral body fractures in cancer patients (Fig. 63.1).
– Contraindications to vertebral augmentation include asymptomatic lesions, patients who are improving on conservative care, ongoing local or systemic infection, retropulsed bone fragment or epidural tumor causing myelopathy, and allergy to bone cement.
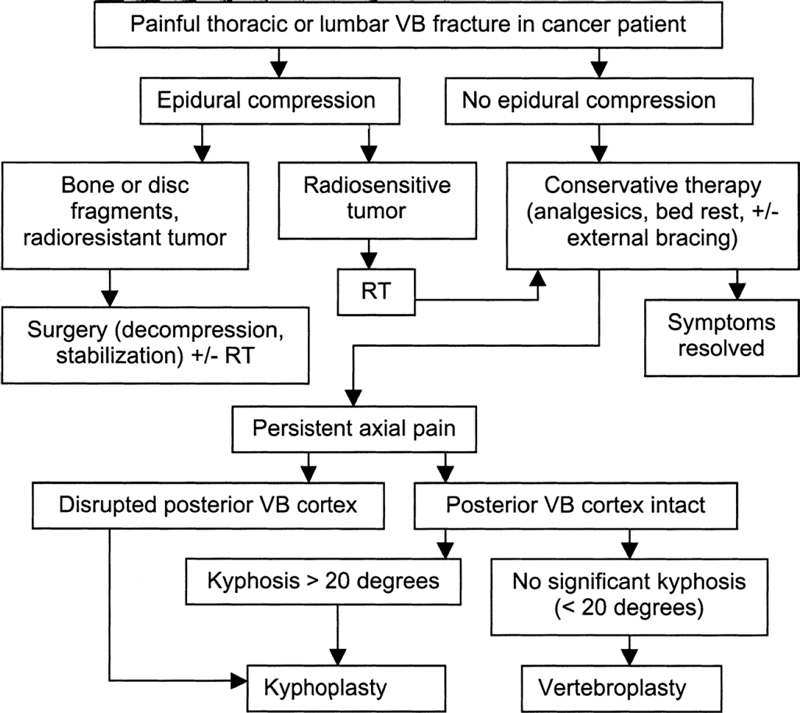
Fig. 63.1 Treatment algorithm for painful thoracic or lumbar vertebral body fractures in cancer patients. See text for details. VB = vertebral body; RT = radiation therapy. (Reproduced with permission from Fourney DR, Schomer DF, Nader R, Chlan-Fourney J, Suki D, Rhines LD, Ahrar K, Gokaslan ZL. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. SCSCT; pg. 624, Fig. 43-3.)
Diagnosis
– Magnetic resonance imaging (MRI) scan of the spine (T1 and short T1 inversion recovery [STIR] sequences) to detect vertebral body edema and associated impending fractures
– Computed tomography (CT) scan of the fractured vertebral body with sagittal reconstruction to evaluate posterior vertebral wall integrity
– Bone scan in some cases to assess acuity of fracture and exclude metastasis in different levels
III. Technique
– Procedures can be performed under general or local anesthesia.
– Patient is placed in prone position on Jackson radiolucent table, with postural reduction of kyphosis if present.
– Biplanar fluoroscopy is used.
– Both techniques start with the percutaneous insertion of (11 gauge) Jamshidi needle or guide pin into the fractured vertebra and end with the injection of PMMA.
– This can be achieved through a transpedicular approach in nearly every case.
– In the thoracic spine the needle can be inserted extrapedicularly, between the rib head and lateral aspect of the pedicle (Fig. 63.2).
– Single or bilateral injection can be performed (it is important to fill the center of the vertebral body).
Vertebroplasty
– After correct positioning of the needle, the inner stylet is removed.
– Contrast material is then injected to ensure that the needle is not positioned in the venous flow path (optional).
– Cement, in thin liquid form, is injected into the vertebra using multiple small syringes.
– The flow of the cement should be followed on the image intensifier.
Kyphoplasty
– After proper needle positioning, a series of tools (drill, curette) are used to create a working channel. Once inserted, the balloons are inflated using volume and pressure controls (digital manometer) to create a cavity within the vertebra.
– Once this has been achieved, the balloons are deflated and removed.
– Thick cement can be fed through the cannula under low pressure to fill the cavity created by the balloon tamp.
– In cases involving the upper thoracic spine, the shoulders can interfere with the lateral view, so a stack of pillows of appropriate height should be placed under the chest to lower both shoulders. Alternatively, the arm and the shoulder are left hanging down parallel to the trunk.
IV. Complications
– Procedure-related: cement leakage can result from fracture clefts or improper instrument position and can occur in the spinal canal, neuroforamen, or disc space.
– Medical: pulmonary embolism, hemo- or pneumothorax, softtissue hematomas
– New adjacent vertebral fracture due to leakage of cement into the disc
– Pedicle fracture
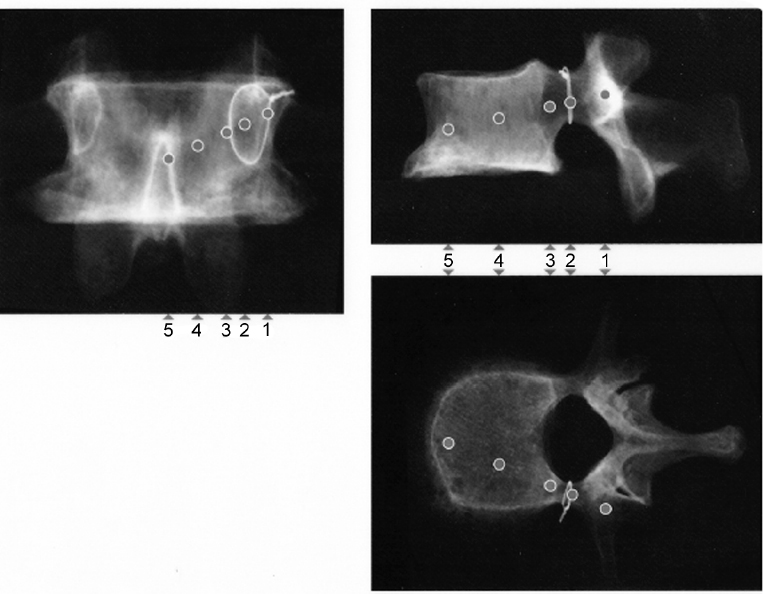
Fig. 63.2 Entry points and trajectories for the transpedicular approach during kyphoplasty. (Courtesy of Medtronic.)
V. Postoperative Care
– Mobilize early with no need for bracing.
– Clinical evaluation and plain spinal radiographs
– Discharge home when patient meets discharge criteria (usually same day or on postoperative day 1).
VI. Outcomes
– All studies reported significant improvements in pain score and functional outcome.1,3
– The risk of neurologic sequelae ranges from 0.4 to 4.0% according to various reports.2–4
– The complication rate is considerably higher for spinal metastasis due to lytic areas involving the vertebral cortex.
– A recent study by Kallmes et al,1 however, showed that improvements in pain and pain-related disability associated with osteoporotic compression fractures in patients treated with vertebroplasty were similar to those for the control group, without treatment.
VII. Surgical Pearls
– The possibility of cement leakage can be overcome through the use of high-quality imaging and slow application of PMMA in a viscous state.
– In cases of focal kyphosis due to index fracture, the levels above and below the fracture should also be considered in the treatment plan. No more than three levels should be treated at one setting. This policy minimizes the risk of microembolization (cement and fat emboli).4
Common Clinical Questions
1. Contraindications to vertebral augmentation include all of the following except:
A. Asymptomatic lesions
B. Retropulsed bone fragment
C. Epidural tumor causing myelopathy
D. Severe pain due to vertebral body compression fractures in patients with osteoporosis
2. Procedure-related complications include all of the following except:
A. Cement leakage
B. Pulmonary embolism, hemo- or pneumothorax
C. New adjacent vertebral fracture
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







