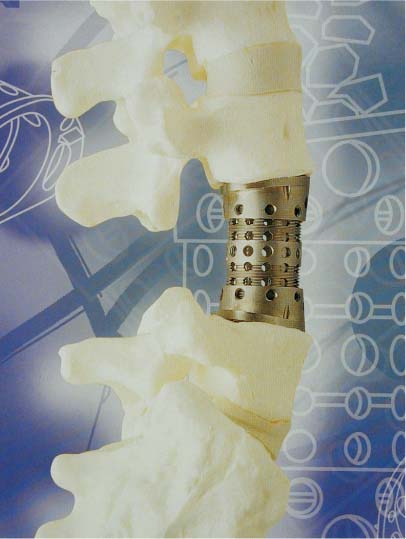
42 Primary and secondary tumors of the spine often involve the anterior and middle columns of the vertebrae.1 Invasion of the posterior elements usually occurs as a direct extension of the anterior disease. Less commonly, the posterior elements alone are affected by tumor. The goals in the treatment of spinal tumors generally include total or maximal resection of tumor, preservation of neurologic function, and maintenance of spinal stability. Total removal of tumor may offer the only chance of cure in certain tumor types (see Chapters 19 to 24). Radical subtotal resection provides the optimal conditions for adjuvant therapy and may prolong survival. However, the need for maximal cytoreduction must be balanced against the risk of causing neurologic deficits during tumor resection. In patients with metastatic disease and limited life expectancy, it would be prudent to forgo maximal tumor removal if residual neurologic function is at risk. Laminectomy alone has been shown to be largely ineffective in the treatment of metastatic spinal tumors.2,3 This highlights the fact that spinal cord compression secondary to ventrally situated tumors cannot be adequately treated by an “unroofing” procedure. In addition, laminectomy is a destabilizing procedure, particularly in the presence of tumors destroying the anterior and middle columns. Therefore, laminectomy alone in the presence of anterior column disease results in the lack of neurologic improvement and pain secondary to spinal instability. The development of various approaches to the anterior vertebral column, as described elsewhere in this book, allows maximal resection of the tumor, preservation of neurologic function, and exposure for anterior spinal column reconstruction. Just as there are several options for approaching the vertebral body, various alternatives are available for restoring the integrity of the spinal column. The type of approach used for resecting the tumor may have a direct bearing on the type of vertebral body reconstruction technique being used. Destructive lesions involving the anterior, middle, and posterior columns mandate reconstruction of both the anterior and posterior elements. Three-column reconstruction may necessitate a “front-and-back” procedure, a posterolateral,4 or a posterior transpedicular approach.5 These procedures may be performed endoscopically,6 with endoscopic assistance,7 or via an open technique. In simple terms, movements of the spine can be considered to be in three planes: axial, coronal, and sagittal. In each plane, there can be either translational or rotational movement. Therefore, there are 12 potential movements of the spine, as there are two directions of translation and rotation around each plane. Anterior spinal constructs replace the vertebral component that is strongest in axial loading (translation in the sagittal plane) and flexion (ventral rotation in the sagittal plane). In the normal spine, the annulus fibrosus, anterior longitudinal ligament, and facet joints limit the degree of rotation and extension that can be performed. Most of the currently utilized vertebral body reconstruction techniques resist flexion and axial forces well. These characteristics mimic the patient’s own vertebral body, which bears ~80% of an axial load and is strong in flexion. However, any reconstruction of the anterior and middle columns needs to take into account the rotation and extension forces that can occur across the construct. Although the intact spinal column relies on the intervertebral disc, various ligaments, and rib cage to resist these rotational and extension forces, reconstruction techniques incorporating an anterior locking plate or posterior fixation system can also provide stability in rotation and extension of the spine. Because the majority of spinal tumors involve the anterior elements, removal of these tumors frequently necessitates replacement of the anterior vertebral elements to maintain stability. The amount of vertebral body and ligamentous structures resected dictates whether instability is likely to occur after surgical intervention. Other factors to consider when predicting postoperative instability include the number of levels involved by disease, the presence of deformity, and the competency of the posterior bony and ligamentous structures. The ideal material and technique for vertebral body reconstruction would approximate the biomechanical properties of the patient’s own intact vertebrae. The replacement material should ideally be long-lasting, readily available in a range of sizes, and technically simple to use. Materials currently in use include autogenous bone, allograft, polymethylmethacrylate (PMMA), titanium cages, carbon fiber polymer cages, or a combination of them (see Chapter 13). Placement of the ventral support depends on the alignment of the spine. If a kyphotic deformity of the cervical or lumbar spine already exists, then the strut replacing the vertebral body should be placed as far ventral from the neutral axis as possible to prevent further kyphosis. If the spine is in normal alignment, then the body replacement device is placed close to the neutral axis to bear the axial loads without creating a rotational moment. The use of autogenous bone graft is associated with a high fusion rate. Autografts that include intact cortical bone, such as iliac crest, ribs, and fibula, can provide immediate structural support. The potential for exogenous infection from cadaveric donor is eliminated with the use of autologous bone. However, harvesting autologous bone may be associated with significant donor-site morbidity such as chronic pain, deformity, infection, and iliac avulsion fractures.8 The use of autogenous bone is indicated where long-term stability by bony fusion is required. Patients undergoing curative spinal tumor resection and those with a long life expectancy are obvious candidates for the use of autogenous bone graft because of the superior fusion rate. Because the most common etiology of spinal tumors is metastatic in nature, the use of autogenous bone is limited to cases of primary benign or indolent spinal tumors such as vertebral hemangioma, eosinophilic granuloma, and giant cell tumor. In cases of metastatic disease, the morbidity associated with bone graft harvest may not be justified if the operative procedure is palliative in nature. In cases where bony fusion may be impaired because of radiotherapy and chemotherapy, improvement in fusion rate may be achieved by the use of vascularized autogenous rib grafts9 or other fusion adjuncts such as bone morphogenic protein or autologous growth factors. Autogenous cancellous bone possesses the desirable characteristics of osteoinduction, osteoconduction, and osteointegration. Cancellous bone lacks structural strength when used alone, but it can be used for packing a cortical allograft, titanium cage, or carbon fiber cage, which provides immediate structural support. To minimize donor-site morbidity, a “trapdoor” technique may be used in harvesting cancellous bone from the iliac crest. A rectangular piece of iliac crest is removed with an osteotome and the cancellous bone between the inner and outer tables of the ilium is removed with gouges. The piece of iliac crest is then replaced and held in place by the overlying fascia. Allograft offers osteoinduction, osteoconduction, and structural support when used as vertebral body replacement. The availability of allograft has improved in recent years with the advent of commercially prepared and machined allograft. A lower fusion rate and delayed fusion have been reported with the use of allograft.10,11 The two most common ways to preserve allograft are freeze-drying and deep-freezing. Freeze-dried allograft offers the advantages of allowing storage in vacuum-sealed containers at room temperature for an indefinite period of time. However, the process of freeze-drying is expensive and time-consuming and has been shown to decrease the torsional and bending strength of the allograft.12 Deep-freezing requires the availability of equipment to store allograft at −70 to −80°C. Criteria for donor selection and mechanisms for bone harvest and storage need to be in place to decrease the likelihood of spreading transmissible diseases and contamination of the harvested bone. The main advantage of using allograft is the absence of donor-site morbidity, especially when a long construct is required for reconstruction. Polymethylmethacrylate (PMMA) is an acrylic cement that is formed by an exothermic polymerization reaction. It does not have the same biomechanical properties as bone. It is not osteoconductive and does not allow osteointegration. It is rigid and brittle once it has solidified. The advantages of PMMA include its ability to conform to the shape of the bony defects, the ease of application, and its widespread availability. Some PMMA mixtures are preimpregnated with antibiotics to decrease the risk of postoperative infection. Barium is added to the cement mixture to allow postoperative assessment by radiography. PMMA can be strengthened by metal reinforcement in the form of Steinmann pins or titanium mesh cages anchored into adjacent vertebral bodies. Because PMMA is not incorporated into the adjacent bone, bony fusion does not occur across the bone-PMMA interface. In patients with limited life-expectancy, solid fusion across the decompression site may not be a realistic or necessary goal. In these situations, PMMA reconstruction of the vertebral body is particularly useful as it offers immediate structural support without the morbidity associated with autogenous bone graft harvest or the cost of using allograft material. Recent follow-up data suggest that vertebral body reconstruction using PMMA may be more durable than first thought. Some patients with PMMA vertebral body reconstruction have intact and stable constructs several years after surgery despite the lack of bony union (Z. L. Gokaslan, personal communication, AO course, Marco Island, FL, September 2001). The main advantages of the titanium and carbon fiber (CF) polymer cages are structural strength and availability. Titanium mesh cages may be cut to length to fit the decompression site (surgical titanium mesh cages, DePuy AcroMed, Raynham, MA; Pyramesh, Medtronic Sof-amor Danek, Memphis, TN; SynMesh, Synthes, Paoli, PA). More recently, expandable cages have become available. These cages are inserted in their compact mode and then expanded once they have been placed in the decompression site. Cage expansion is achieved by either a screw-thread mechanism (Lift, Medtronic Sof-amor Danek, Fig. 42-1; Modulics, Stryker Corp., Kalamazoo, MI) or a ratchet mechanism (Synex, Synthes, Paoli, PA; VBR, Osteotech, Eatontown, NJ). The CF polymer cages have the added advantage of being radiolucent. This allows radiographic assessment of bony fusion through the cage. Stacking together cages of various heights allows for adjustment of implant height to fit the decompression site (Stackable Cage System, DePuy AcroMed). Shedding of carbon fibers into the surrounding soft tissue has been reported with CF implants used elsewhere in the body. Cages can be packed with cancellous bone chips or PMMA, depending on whether bony union is intended. The biomechanical considerations for various available materials are summarized in Tables 42-1 and 42-2. Figure 42-1 An expandable titanium vertebral body replacement device. (LIFT cage, Sof-amor Danek, Memphis, TN.) Bone morphogenic proteins (BMP), autologous growth factors (AGFs), and demineralized bone matrix (DBM) are various fusion adjuncts available to enhance bony fusion after vertebral reconstruction. BMP consists of a family of proteins found in bone that stimulate osteoblastic activity leading to earlier and stronger bony union. Two forms of commercially available BMP (OP-1, Stryker Corp., Kalamazoo, MI; Infuse, Medtronic Sof-amor Danek) are produced by recombinant DNA technology. Currently, the use of BMP is not indicated in spinal tumors because of the concern about BMP promoting tumor growth.
Vertebral Body Reconstruction Techniques
 Biomechanics of Vertebral Body Reconstruction
Biomechanics of Vertebral Body Reconstruction
 Materials Available
Materials Available
Autogenous Bone
Allograft Bone
Polymethylmethacrylate
Titanium Cages and Carbon Fiber Polymer Cages
Fusion Adjuncts
| Technique | Advantages | Disadvantages |
| Anterior | Direct access to ventral tumor mass | Morbidity related to thoracotomy or retroperitoneal approach |
| Avoids further destabilization of the spine if posterior elements not involved by tumor | ||
| Excellent access for vertebral body reconstruction with structural graft or cages | ||
| Posterior/Posterolateral | Familiar exposure | Extent of decompression may be hindered by spinal cord |
| Allows circumferential decompression with transpedicular approach | Choice of vertebral body reconstruction material is limited by access | |
| Allows circumferential reconstruction via a single approach | ||
| “Front and back” | Excellent access for maximal tumor removal | Morbidity related to two separate incisions and prolonged procedure |
| Excellent access for circumferential reconstruction of the vertebral column | ||
| Lateral extracavitary | Extensive soft tissue dissection | Similar to posterior approach |
| Potential for increased blood loss | ||
| Potential wound complications | ||
| Otherwise, advantages similar to posterior approach | ||
| Endoscopic | Minimally invasive | Steep learning curve |
| Specialized equipment required | ||
| Limited access for reconstruction |
| Material | Advantages | Disadvantages |
| Autologous bone | Promotes bony fusion | Donor-site morbidity |
| Same modulus of elasticity as resected bone (corticocancellous graft) | ||
| Indicated in patients with primary bone tumors with prolonged survival | ||
| Allogeneic bone | Promotes bony fusion | Availability varies |
| Lack of donor site morbidity | Chance of transmissible diseases and contamination of bone graft | |
| Polymethyl methacrylate | Resists axial loading and flexion well | Inhibits bony fusion |
| Easily molded to fit decompression site | Poor strength in extension and rotation | |
| Readily available | ||
| Titanium cages | Resists axial loading and flexion well | Expensive |
| Readily available | Radiopaque and therefore difficult to assess extent of bony fusion on x-rays | |
| Cages can be cut to length or expanded to provide tight fit |
Autologous growth factors are naturally occurring proteins found in the bloodstream that can promote bone growth. A commercially available process takes one unit of the patient’s blood, removes the cellular elements, and then concentrates the patient’s own autologous growth factors via a patented ultrafiltration device. The AGF gathered, ~20 cc in volume, is then mixed with autograft, allograft, or hydroxyapatite granules to enhance fusion.
Demineralized bone matrix contains various growth factors and BMP that promotes bony fusion. DBM is derived from bone, and various commercially prepared preparations are available. In metastatic spine disease, bony fusion may not be the goal of spinal reconstruction after tumor resection. Therefore, the role of these fusion adjuncts in tumor surgery of the spine is still being defined.
 Regional Considerations
Regional Considerations
The Cervical Spine
Due to the anatomy of the cervical spine and the position of the spinal cord, vertebral body replacement in the cervical spine is only practical from an anterior or anterolateral approach. Surgical approaches for tumor resection of the cervical spine are covered in Chapter 27. In brief, anterior decompression of the cervical spinal cord is achieved by maximally removing the tumor until the dura is visualized. When the tumor involves the transverse foramen and vertebral artery, maximal tumor resection may be attempted by skeletonizing the vertebral artery. Tumor may be left behind if one is not aiming for a curative resection. Planned resection of the involved vertebral artery along with the tumor requires careful preoperative evaluation of the patient’s cerebral blood flow reserve. Acute unilateral vertebral artery occlusion carries a low risk of delayed ischemic events even though the patient may have tolerated a period of balloon test occlusion preoperatively.13 However, one may need to consider performing a vascular bypass if there is the potential for bilateral vertebral artery compromise during the course of radical tumor resection.
A wide corpectomy, extending to the uncovertebral joints bilaterally, is typically required to ensure adequate decompression of the ventral surface of the cord. The size of the decompression site is then measured. When using autogenous bone, the iliac crest is exposed at least 2.5 cm posterior to the anterior superior iliac spine (ASIS) to decrease the chance of an avulsion fracture of the ASIS, particularly in females who are prone to osteopenia.8 A piece of bone measured to fit the decompression site is cut with a sagittal saw and an osteotome. This provides a tricortical graft, which is then shaped to fit the decompression site. A small ledge is created at the posterior margin of the vertebral bodies to prevent posterior migration of the bone graft. The bone graft is then place under slight distraction either via a Caspar distractor or with gentle traction of the head. The position of the graft is checked to ensure the absence of cord compression by the graft itself. The distraction force is then removed and an anterior cervical locking plate applied.
With the availability of allograft, cervical vertebral body reconstruction may be performed with fibular or radial allograft. Freeze-dried or deep-frozen allograft is prepared by soaking in an antibiotic solution. The cortical allograft is then cut to appropriate length and packed with autologous bone or PMMA.
Titanium mesh cages have been used in cervical body replacement. These cages are packed with autologous bone, allograft bone, or PMMA. More recently, expandable cages have become available. These expandable cages are easy to insert in their nonexpanded form and can be expanded after insertion to precisely fit the decompression site.
The Thoracic and Lumbar Spine
In the thoracic and lumbar spine, vertebral body reconstruction may be accomplished via either an anterior or a posterolateral approach. Surgical approaches to the thoracic and lumbar spine are described elsewhere in this book. The choice of the type of reconstruction technique is influenced by the surgical approach used. With anterior approaches, the corridor available for graft placement is usually wide enough for insertion of cortical autograft, allograft, or cages. Decompression of the ventral aspect of the thecal sac is achieved by bony and tumor removal until the contralateral pedicle is visualized. The adjacent vertebral end plates are prepared by removal of the annulus fibrosus and cartilaginous end plates. The bony end plates should be preserved to avoid postoperative subsidence of the graft or interbody device. Expandable cages, packed with autologous bone chips, are easy to insert and readily available. An anterior locking plate or screw-rod construct is then used to secure the construct. If the disease is confined to the anterior vertebral elements, then additional posterior instrumentation may not be required. If there is posterior element destruction or involvement of a junctional zone, then posterior instrumentation may become necessary to ensure spinal stability.
In metastatic disease of the spine, the use of PMMA as vertebral replacement may be justified due to the limited life-expectancy. Various techniques have been described for molding PMMA into the shape of the decompression site.6,14
With posterolateral approaches via the pedicles, the exiting nerve roots may be sacrificed on one side in the thoracic region to improve access to the vertebral body. Reconstruction of the vertebral body in this situation requires the replacement structure, be it bone or cage, to fit through the available corridor without any significant retraction of the thecal sac. Below the conus medullaris, some retraction of the thecal sac is possible without risking neurologic deficits. However, access to the vertebral body in the lumbar region from a posterior approach is limited by the need to preserve the nerve roots. In metastatic disease of the spine, which most frequently involves the thoracic spine, a posterolateral approach may be desirable to avoid entering the chest or abdominal cavity in these patients, who are often cachexic with a limited life-expectancy.5 PMMA is particularly suited for this purpose as it can be injected and molded to fit the resection cavity in the vertebral body from a posterolateral approach. Posterior instrumentation is required with this reconstruction technique because all three columns of the spine are weakened.
In selected patients who harbor indolent or isolated lesions, surgery with a curative intent may be performed. Total en bloc spondylectomy has been reported to provide long-term survival in primary spinal tumors15 as well as solitary metastatic disease to the spine.16 Total spondylectomy may be performed from a purely posterior approach as described by Tomita et al.15 More commonly, it is performed via a two-stage posterior/anterior approach. This involves removal of the posterior elements and posterior instrumentation followed by anterior en bloc corpectomy. Vertebral body reconstruction is then performed using any of the techniques already described.
 Future Directions
Future Directions
Technology for spinal reconstruction is advancing at a rapid pace. The case illustrations presented in the next section represent some of the currently available and accepted methods of vertebral body reconstruction. Without a doubt, newer and less invasive techniques will be developed in the future to provide the anterior column support, which is often lost in cases of vertebral neoplasms. Some of the new techniques currently being tried include percutaneous vertebroplasty with PMMA and percutaneous balloon kyphoplasty. These techniques were initially developed for the treatment of osteoporotic spinal fractures and may play a role in the palliative treatment of vertebral body tumors causing intractable pain and deformity.
 Case Illustrations
Case Illustrations
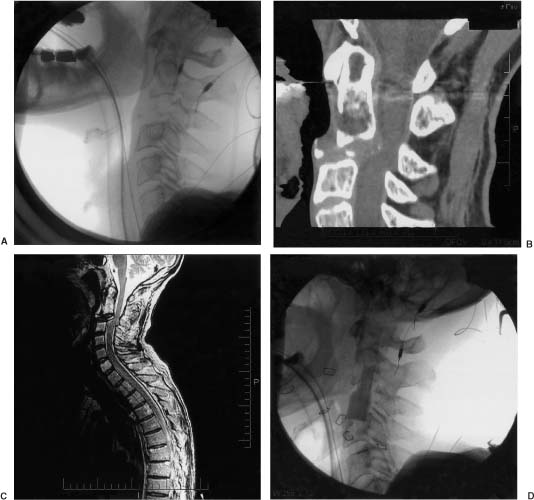
Case 1 (Fig. 42-2)
A 54-year-old man presents with severe neck pain and decreased range of cervical spine movement following a minor fall. He also had some hip pain, and further investigations revealed multiple myeloma. The patient was neurologically intact.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree